I think everyone who can play this file will find it both instructive and illuminating and actually very very …”interesting”…So go ahead, Mikey. LlSTEN TO YOUR PRESIDENT!!!!! Tee hee.
Tag Archives: seclusion
READ THIS, Michael Edward Balkunas, MD of Hospital of Central Connecticut in New Britain, CT, Before You Throw Another Psychiatric Patient Into Your Supermax Seclusion Cells!

This is from the Special Rapporteur to the UNITED NATIONS CONVENTION ON TORTURE 2013:
As the previous Special Rapporteur stated: “Torture, as the most serious violation of the human right to personal integrity and dignity, presupposes a situation of powerlessness, whereby the victim is under the total control of another person.”14 Deprivation of legal capacity, when a person’s exercise of decision-making is taken away and given to others, is one such circumstance, along with deprivation of liberty in prisons or other places (A/63/175, para. 50).
32. The mandate has recognized that medical treatments of an intrusive and irreversible nature, when lacking a therapeutic purpose, may constitute torture or ill-treatment when enforced or administered without the free and informed consent of the person concerned (ibid., paras. 40, 47). This is particularly the case when intrusive and irreversible, non- consensual treatments are performed on patients from marginalized groups, such as persons with disabilities, notwithstanding claims of good intentions or medical necessity. For example, the mandate has held that the discriminatory character of forced psychiatric interventions, when committed against persons with psychosocial disabilities, satisfies both intent and purpose required under the article 1 of the Convention against Torture, notwithstanding claims of “good intentions” by medical professionals .
Medical care that causes severe suffering for no justifiable reason can be considered cruel, inhuman or degrading treatment or punishment, and if there is State involvement and specific intent, it is torture.
63. The mandate has previously declared that there can be no therapeutic justification for the use of solitary confinement and prolonged restraint of persons with disabilities in psychiatric institutions; both prolonged seclusion and restraint may constitute torture and ill-treatment (A/63/175, paras. 55-56). The Special Rapporteur has addressed the issue of solitary confinement and stated that its imposition, of any duration, on persons with mental disabilities is cruel, inhuman or degrading treatment (A/66/268, paras. 67-68, 78). Moreover, any restraint on people with mental disabilities for even a short period of time may constitute torture and ill-treatment.78 It is essential that an absolute ban on all coercive and non-consensual measures, including restraint and solitary confinement of people with psychological or intellectual disabilities, should apply in all places of deprivation of liberty, including in psychiatric and social care institutions. The environment of patient powerlessness and abusive treatment of persons with disabilities in which restraint and seclusion is used can lead to other non-consensual
Domestic legislation allowing forced interventions
64. The mandate continues to receive reports of the systematic use of forced interventions worldwide. Both this mandate and United Nations treaty bodies have established that involuntary treatment and other psychiatric interventions in health-care facilities are forms of torture and ill-treatment.79 Forced interventions, often wrongfully justified by theories of incapacity and therapeutic necessity inconsistent with the Convention on the Rights of Persons with Disabilities, are legitimized under national laws, and may enjoy wide public support as being in the alleged “best interest” of the person concerned. Nevertheless, to the extent that they inflict severe pain and suffering, they violate the absolute prohibition of torture and cruel, inhuman and degrading treatment (A/63/175, paras. 38, 40, 41). Concern for the autonomy and dignity of persons with disabilities leads the Special Rapporteur to urge revision of domestic legislation allowing for forced interventions.treatment, such as forced medication and electroshock procedures.
JUST THOUGHT YOU SHOULD KNOW, MICHAEL EDWARD BALKUNAS, MD, YOU MOTHERFUCKER…BUT THEN YOU ALREADY KNOW THIS, BECAUSE YOU DO WHAT YOU DO TO PATIENTS DELIBERATELY AND WITH PURPOSE!
“Punishment is Just Abuse with An Excuse”


See the website Punishment Hurts Everyone, at http://abusewithanexcuse.com. This is an amazingly brave site with writing and thoughtful insights that might upset those who think that spanking kids is good for them, but for most of us, who know it only traumatizes and harms them, it will be an illuminating page indeed. Check it out! Great stuff here from a man who has put his ideas into practice and never once punished his own children, teens now and well-adjusted and happy to boot. Who’da thunk it could be done? (Well I did, for one, and maybe you too!)
Solitary Confinement is Torture and You, Michael E. Balkunas, MD, Can Go Fork Yourself!
This is from the New York Times today:
To the Editor:
Re “When Cell Door Opens, Tough Tactics and Risk” (“Locked In” series, front page, July 29):
The events leading to Charles Jason Toll’s death highlight the dangers of prison procedures, especially for vulnerable inmates who suffer from mental illness. Particularly concerning is Mr. Toll’s solitary confinement, a disciplinary technique repeatedly identified as ineffective and counterproductive, and even as torture.
The Justice Department has found that solitary confinement of mentally ill people violates their rights under the Eighth Amendment and the Americans With Disabilities Act.
Solitary confinement worsens psychological symptoms and can trigger outbursts tied to the person’s feelings of hopelessness and loss of a sense of self through extreme social isolation and sensory deprivation.
Providing mentally ill people with appropriate and compassionate mental health care, including integration of psychiatric, psychological and psychoanalytically oriented treatments, is crucial in restoring a person’s identity, alleviating feelings of loss and distress and reducing violence.
Mr. Toll’s solitary confinement, suffering and death were avoidable, and again show that the mentally ill are more likely victims of violence, not the perpetrators.
SUSAN McNAMARA
Middletown, Conn., July 30, 2014
The writer is a psychiatrist.
_____________________________
When I was a patient in May and June 2014 at New Britain’s Hospital of Central Connecticut, Dr Michael Edward Balkunas regularly imprisoned me in a horrific seclusion cell, without a single amenity but a concrete built-in bed and rubberized mattress, for nothing more than making too much noise for the approved hospital milieu. In fact, several nurses took it upon themselves, with Dr Balkunas approval, to do the same. This became literally routine. I was NOT, as is required by the Centers for Medicare and Medicaid, in IMMINENT danger of causing severe harm to myself or others. No, I was loud, disruptive and uncooperative, and I was rude. Period.
My first reaction when the double doors locked behind me was immediately to start screaming, at the top of my lungs, from the base of my lungs. But screaming brought no one. Okay, they did soon come in at me with three IM injections, but they came back every time with IM injections anyway, because as I took to calling it, these were part of the drill, they were “punishment injections.” I was pushed onto my stomach and shoved into the mattress so I couldn’t breathe and injected whether I liked it or not. I tried to say, “STOP! I will take the injections, just don’t hold me down.”
But sometimes they didn’t listen to me, and held me down anyway, and I got scared that they would kill me, because it didn’t matter that I didn’t struggle. There were four of them to the one of me, and they expected me to fight and so they forced my face into the mattress and held me tight, hard, and with all their weight….until I felt my breath go out of me. Did they have any idea that I was NOT struggling, that I felt I was going to die? Did they have any idea that they were killing me?
I don’t know. I don’t know. All I know is that I felt in mortal danger when they wouldn’t let me just accept the injections on my own, in my arm, but insisted on giving them to me by force in the buttocks, even when I said I would take them voluntarily.
Then they would leave and lock the double doors. And I would scream, and NO ONE would respond, even though I eventually learned that they could not only hear me through the intercom hidden somewhere in the ceiling, they could also talk to me. They wouldn’t but they could have. When screaming brought no one, I would strip and urinate on the floor, and I would defecate too as much as i could, and smear everything on the walls and floor. I would even eat it and paint it on my body. I didn’t care, I DIDN’T CARE! I just wanted someone to come in and help me.
Several times I washed and colored my hair with urine, thoroughly. But no one came back for hours. The urine, which completely soaked my hair, had time to dry completely. Not that they cared or noticed. If they had, they said nothing. It was nothing to them. Only Barbara RN asked me what was in my hair, and insisted that she wash it out when finally they released me. I went with her to the shower-tub room and allowed her to do so, but only one other person was kind enough to notice and do that. Everyone else just released me and expected me to somehow be reformed and “better” after my hours of punishment.
Of course that wasn’t the case. I got worse, much worse. I started defecating in my bedroom, at any hour,for any reason, any time I was frustrated or angry. They decided I had “borderline personality disorder,” that I was simply manipulating them. They failed to see that they had traumatized and broken me. They failed to see their continuing role in my behaviors…which were getting worse and worse the more they punished me. Every time they secluded me, or four-pointed me, I regressed more.
Dr Balkunas actually decided to commit me to the State Hospital claiming it would help me “get better.” But really he was just in punishment mode. You could tell, because he wasn’t using any of the methods that you are supposed to use for REAL borderline patients….If he really believed I was BPD he wouldn’t have kept at it. But he knew from my brother, a psychiatrist too, and my own psychiatrist, that I do not have BPD, so that was bogus and just an excuse to torture me. He didn’t really think I had BPD. He just needed an excuse to use solitary confinement and he knew that schizophrenia was NOT a good reason. A very BAD reason in fact, so he invented a secondary diagnosis to use. But the thing is, there are other therapies you are supposed to use in BPD, and he never bothered to treat me with anything but punishment and then threw up his hands and said, Well, the antipsychotic drugs take time to work, so you will go to the SH until they do.
Bastard! He gave up on me without even trying to help…so-called saintly doctor. Just a bastard! Because torture doesn’t work to make me better, he decides that I am the one at fault????? Well GO FUCK HIM UP THE ASS WITH A BROKEN GLASS JAR!
Nude Schizophrenic in Restraints While Bored Nurse Looks On
Actually I “deserved” four-point restraints. I was “violent.”

But I want to explain what “deserving” restraints and being “violent” at New Britain General Hospital (Hospital of Central Connecticut) means in 2014.
I also want to tell you something else even more important: In Connecticut, the staff at almost every psychiatric unit or hospital will insist that “we only use seclusion and restraints when essential, when a patient is absolutely out of control and extremely violent, and cannot be controlled in any other way.”
Trust me, I know, because they have said this to me.
But what you need to know is that they are NOT talking about some 300 pound man hopped up on PCP, waving a machete. For one thing, that person, whom I believe to be largely mythical at least in ordinary psych units, or if real now largely confined to correctional and law enforcement settings, the person they are talking about, the rule, not the exception to the rule of the “extremely violent” person whom they claim must be restrained due to lack of any other method of control, is, to put it grammatically correctly, I.
And let me tell you about me. I will turn 62 years of age in November. I am 5 feet 3 inches tall, weigh, maybe 110 pounds on a good day, and have been consistently described as “poorly muscled.” I am also unable to use my left arm for much of anything, due to injuries sustained at the Institute of Living in 2013, including a small tear in my rotator cuff and possibly more than that– a fact the HOCC nurses/security guards knew and used to their advantage when subduing me. I also want you to know that I am a decades-long vegetarian on the principle of non-violence — to people as well as to animals. I have opposed the death penalty since I was a nine year old child (when I first learned of it) and do not even believe in the principle of prisons, or in treating our convicted “criminals” the way we do now.
Yet in every single hospital I have been in since 2000, and of course for years before then (“before they knew better”) I have been brutally secluded and restrained multiple times as “OOC” — out of control — and “violent.” In addition to either physically holding me down by brute force, one person to each limb and one to my torso (this was at the only 2 hospitals that did not actually resort to mechanical four-point restraints– compared to the dozen others that did), they would routinely inject me with one to three drugs as chemical restraints.
I am the rule, not the exception to it, of their supposedly “extremely violent mental patient” who is so OOC — out of control — that Connecticut hospitals refuse to eliminate the use of restraints and seclusion, because they “might need them.” I am the typical example of the person they claim they absolutely must have the right to resort to violence against, for their own safety and mine.
Okay, so am I truly violent? What did I do to deserve their brutality? Or should we say, their “protective measures?” Well, at HOCC, in the Emergency Department, this is what happened, and I kid you not: I came in by ambulance, involuntarily, in the sense that I did not want to go but was brought in by EMTs and given the “either the easy way or the hard way” choice by police. But I did not resist it or fight. I was not restrained in the ambulance. in fact, I was mute and merely handed them my med sheet and my detailed Advanced Directive, on the first 2 pages of which is the important information about my trauma history and the critical need to know points about how to deal with me.
When I arrived I was quickly shunted to the psychiatric crisis section and into a curtained off cubicle. No one took my cell phone from me, or the single book of my artwork that I had managed to bring with me. So I texted everyone I could for as long as I could. For a while I tried to obtain a crayon to communicate with, eventually and in desperation, writing with ketchup on the outer carton of my dinner container, begging for something to write with. Instead of helping me out, the head ER nurse penned me a note saying that I would not get anything to write with, that either I spoke out loud or she would not listen to me. How very odd and evil that she wrote this to me! She didn’t speak to me, she wrote it, as if I were deaf, even while saying that she knew I could speak and would not talk with me unless I did so… The idiocy of that act just sends sparks of rage through my brain even now. She later spied my art book next to me on the gurney, and suddenly rushed me, snatched it out from under my thigh and raced away with it, holding it triumphantly as if she had won a prize. I was incensed. Why hadn’t she just asked me for it? And how did I know what she was going to do with it? Would she keep it safe and sound? Actually, though, I mostly just reacted instinctively: Someone had stolen the only thing I had of my own in my possession, and she had simply snatched it away from me, without a word or even a polite request. So I did as anyone would do, I think. I raced up behind her and snatched it back! Well, that was a mistake. That was bad, that was bad bad bad. I heard people groan and swear. I was grabbed from behind by two security guards and the book was wrenched from me again.
Remember, I was mute so I couldn’t say anything, but I tried to resist, tried to gesture that the book was mine and she had no right too take it from me. Instead of explaining that she would protect it and take care of my things, people started talking about how I had attacked the nurse, had assaulted her…She told them to put me in seclusion. The guards dragged me, resisting in panic, towards this hidden room, and I heard another nurse warn them of my medical history with a torn left rotator cuff. Hearing this, the guard on my left side, grabbed my shoulder and wrenched it higher until I let out a blood curdling scream, wordless but vocal. “Aha! I thought you could make sounds!” he said in triumph, wrenching me again until I sobbed in agony. Then they dumped me in the seclusion room, with only a hospital johnnie on me, and locked the door behind them.
Even though I had no words to speak my rage and panic, I screamed and screamed. They came through the door with needles, held me down and injected me. Then, when in a rage reaction, I disrobed, they decided to four-point restrain me. I heard a guard say, “we really have no reason to restrain her, you know.” But the other said, “It doesn’t matter, we will find a reason.” So they did . Terrified, I did not resist, because they held me down by the left shoulder causing me so much pain I was afraid they would hurt me permanently. I also hoped upon hope that if I didn’t resist, they would let me out quickly. Believe me, I had been through this routine enough to know what to try to do to minimize the consequences and the damage…
Fast forward to my being sent to the psych unit, about which I no longer had any choice, being labelled violent now and OOC as well as mute and schizophrenic (I hate that word but they used it). When the doctor who admitted me, Dr. Michael Balkunas, came to see me the next day, I was still mute. He asked me how I was and I gestured my need for a writing implement to answer his questions. He coldly told me that he would not speak with me if I would not talk out loud. Then he got up and walked out the door, with nothing more to say. I was by then so upset and outraged that I got up off the bed, which was the only furniture in the room, and slammed the door after him. I meant only to make a noise to express my frustration, but unfortunately it caught him in the shoulder. This was not intentional, not that I recall, though I confess I was so enraged by his dismissal of me, especially after the violence inflicted on me not once but twice the night before in the ER on his orders, that it is possible I wanted the door to make contact with him. What I know is that I most certainly did not intend to injure him. I only wanted him to know, before he walked away from me, that I was angry and “speaking” to him the only way I could. Dr. Balkunas’s reaction was itself swift and violent in the extreme, and extremely personal. Enraged, his face beet-red, he bellowed at the nurses to order guards to force me into “Seclusion! Seclusion! Restraints! Restraints!”
Before I could do anything or even assent to walk there, I was bodily dragged down the hall by my injured shoulder, to one of the most horrifying seclusion suites I have ever seen. A set of two cells, each lockable from the outside, completely barren and cold except for a concrete bed set into the concrete wall, with a plastic mattress on it. Nothing else. No commode, no bed pan, nothing but two obvious cameras in the ceiling, but no obvious way for me to communicate with anyone. They locked me in, locked the second door a room away, so I was thoroughly alone and soundproofed from the rest of the unit, and walked away. I panicked immediately, and urinated on the floor in my panic. I took off my clothes. I screamed — wanting someone to talk to me, I wanted warm dry clothing to wear, but there was no response. I screamed and screamed. Nothing. Not a word. I did not even understand at that time that there was an intercom they could hear me through. I thought I was completely alone and abandoned, but for the eye of the camera. So I did what I had to. I KNEW what would happen, I knew this because it was SOP. But I was freezing in there, with the A/C on full bore and at 110 pounds and a history of frost bite I cannot tolerate being cold. I also had NO inkling as to how long they would keep me there, one hour or sixteen. All I knew was that I could not tolerate the isolation, one, and I would not survive the freezing temperature, two.
So I took the urine-wet johnnie I had taken off and I rolled it into a rope and tied it around my neck. I pulled on it as if to strangle myself. It was useless of course, because I couldn’t keep pulling it without letting go and then I would breathe. And I didn’t want to die, I just wanted it to LOOK as if I were strangling myself so someone would come in and I could explain that I was COLD! Well, finally the intercom crackled to life and someone said, “Pamela, take that away from your neck now.” I gestured something that clearly indicated, “I’m freezing cold!” The voice spoke again, “If you don’t remove that from your neck, we will restrain you.” I answered silently but in clear gestures, “I need something warm to wear!” Well, this was a battle I was destined to lose, of course. And eventually but not so quickly as to indicate that they were seriously concerned about my safety, guards and nurses entered the room, along with a gurney, and they did as they had threatened, injuring me in the process. They grabbed me and hoisted me onto the gurney and locked me into leather restraint cuffs, in a painful and illegal spread-eagle position, despite my groans of pain and protest, then they refused even to cover me with a blanket. Someone threw a small towel over my lower torso and that was all. They they positioned an aide at the door and trooped out. I screamed my lungs out, and gestured my desperate need for water and warmth, but the aide simply ignored me, saying she wasn’t permitted to talk to me, and couldn’t get me what I needed. That was how violent I was. And that is how the most violent patients are treated and why they MUST be restrained, for their own safety and the safety of others…Right? NOT! ALL the other times I was secluded it was because i was disturbing the peace of the unit. I was loud and complaining, or simply “agitated” because i walked the halls too much.
That was it. That is the rule not the exception, and if you read my posts about my incarceration at the Hartford Hospital Institute of Living in the winter of 2013 you will get a similar picture. I am not the 300 pound crazed man on PCP wielding a weapon, no, I am a small, elderly woman who is non-compliant with the unit milieu and wants only to be warm…that is about it. But each and every hospital claimed that I had to be restrained, that they had NO alternative, that I was so violent that they had no choice, even though it often took only one or two people to do so, because I didn’t resist or say a word, just lay there while they pinioned me to the bed. Now you tell me that restraints and seclusion are necessary ‘modalities of treatment” that cannot be done away with because they might be needed in an emergency. Emergency schmergency. I am that emergency and they were and are NEVER needed, EVER.
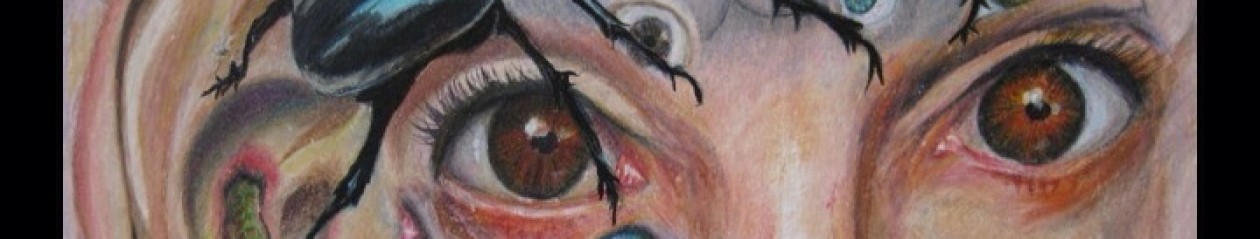
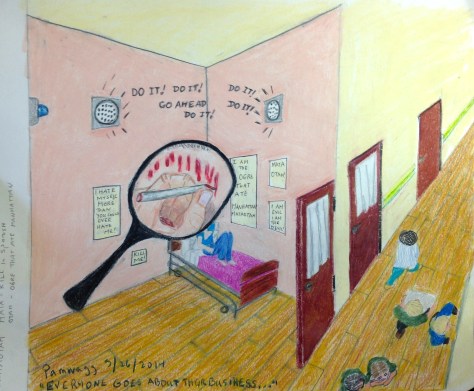
Hospital Seclusion Room…plus

When I was at New Britain General Hospital in the spring of 2014, the security guards stripped me naked and left me in the freezing and barren seclusion room…This is a depiction of a younger woman largely because no one gives a damn about what happens to a 61 year old woman anywhere..but the seclusion room is pretty danged accurate.

AUDIO Interview with Pamela Spiro Wagner: WNPR on Connecticut Hospitals’ Use of Restraints and Seclusion
(***SEE PAMELA’S COMMENTS AT BOTTOM OF PAGE…)
Connecticut Hospitals Responding to Psychiatric Restraint Numbers
Pamela Spiro Wagner
Pamela Spiro Wagner’s apartment is full of art she’s made while in psychiatric care. One piece dominates the room. It looks like a painting at first. It shows a threadbare seclusion room and a restraining bed.
“That’s made of Vogue magazines. If you look at it, you’ll see there’s a little label of Prada leather on the leather restraints, which was done on purpose,” Wagner said. She made it while alone in a hospital seclusion room. The magazines were the only art supplies she had.
Wagner has schizophrenia. She’s been in and out of Connecticut hospitals for decades, and she knows what it’s like to be restrained. “They use leather, or rubber, or plastic, or whatever restraints that they wrap around your wrists, usually tight because they don’t want you to get out. They pull them as tight as possible to the sides of the bed,” she said.
Wagner was put in four-point restraints. That means each limb is bolted to the bed, and she said she’s stayed there for nearly a day at a time. “I would just scream from the base of my lungs,” she said, “like the screams that if you had any heart, your heart would break if you heard me scream.”
“Restraint is Pretty Traumatic”
Patricia Rehmer, Commissioner of the Connecticut Department of Mental Health and Addiction Services, said the department has cut down on restraint since receiving a federal grant in 2008. “We know,” she said. “The literature is clear; the clients are clear. Seclusion and restraint is usually a pretty traumatic event. If we had our way, there would be no seclusion and restraint. We’d love to get to zero, but that’s not always possible.”
The Department of Mental Health and Addiction Services oversees state hospitals in Bridgeport, New Haven, Hartford, and Middletown. Rehmer said that because patients stay longer at state hospitals, doctors and nurses have more time to work with them on ways to avoid restraint. “Frankly, there are differences between our hospitals, our hospital beds, and general hospital beds, for example,” she said.
Read C-HIT Report: State Restrains Psychiatric Patients at High Rate
Restraining or secluding patients used to be commonplace in psychiatric facilities, but ten years after a series of deaths nationwide, there’s been a push to lessen the time patients spend restrained. Federal data released earlier this month showed that Connecticut’s rates of restraint are still high compared to most of the country – more than double the national average. The state ranks eleventh nationwide, and third for use of restraints among the elderly.
Connecticut Institutions Adapt
Bridgeport Hospital topped the list statewide. The hospital has a large geriatric unit, and the numbers were high for elderly patients.
“We realized about a year and a half ago that we were really having a problem,” said Ryan O’Connell, Bridgeport Hospital’s vice president of performance and risk management. He pointed out that the numbers only go up to the middle of 2013, and said that the hospital started changing its practices since then. “It was much more common for us to go to some type of restraint,” he said.
O’Connell said the image of the barren room and four leather straps is all wrong at Bridgeport. They’re mostly trying to keep patients with dementia from wandering off and into danger. “I think it’s really important,” he said, “that nobody thinks that we were tying people down [by their] hands and feet.”
Bridgeport is moving toward something called comfort rooms, with colorful wallpaper, toys, games, or comfortable furniture. They’re becoming common alternatives in a lot of institutions, like Connecticut Valley Hospital in Middletown — a state hospital that cut back on using restraints by about 88 percent in the past decade.
In 2002, a patient died after being restrained at CVH. The hospital conducted investigations after the death, but Director Charles Dike said they’d already decided to make a change before it happened. “Our target is to make sure we use it as sparingly as possible, only when it is absolutely necessary, and that we discontinue it as quickly as possible,” he said.
CVH started using comfort rooms years ago. Dike said that instead of putting a patient in restraints, they try to encourage a patient to spend a little time alone doing something relaxing. He said, “If somebody says to me, when I’m not doing so well, I like to go into my room and play music, and that helps me calm down…” He said that nurses will remember, and bring it up if the patient starts to lose control.
Dike doesn’t expect to stop using restraints. He said there will always be outliers — patients who come straight from emergency rooms and prisons.
Ellen Blair is the nurse director at Hartford’s Institute of Living, which is part of the Hartford Hospital system. Figures for 2013 show Hartford Hospital restrains patients at a little over the state average, but she said they’ve cut back since then thanks to new training programs and more comfort rooms.
Blair said that when a patient does go into restraints, they’re looked after. “I personally go and make sure I know that patient,” she said. “We all talk about it at least every couple of hours, because we don’t want to keep it going any longer than we have to.” She said patients aren’t left alone, and that restraint is only used as a last resort when patients are dangerous to themselves or others.
“Every day,” Blair said, “we come here thinking, okay, we’re going to have a good day. We’re going to prevent people from getting agitated and having to go to that level.” Restraint, however, remains a last resort these hospitals said they don’t plan to take off the table entirely.
Seclusion Room: Cell or Sanctuary — Amazing Article from 1959

THE SECLUSION ROOM – CELL OR SANCTUARY?
By HUMPHRY OSMOND, M.D., 1959
Superintendent The Saskatchewan Hospital, Weyburn
SECLUSION ROOMS, found in most psychiatric hospitals, too often look as if they were intended as temporary quarters for wild animals, or perhaps as storerooms for dangerous chemicals, rather than as shelters for sick and distressed humans.
Yet, the purpose of seclusion is clear and admirable. It is intended to reduce interaction following a rupture in interpersonal relationships between the patient who is being secluded and other patients, or members of the hospital staff.
Seclusion usually occurs when there has been acting out or a threat of it. While skilled psychiatric nurses can often handle such situations without using seclusion, it is proper that a patient, in an explosive situation, should have an opportunity to withdraw to a suitable spot to be alone for a time or in the company of someone he trusts.
When children quarrel with siblings or parents, they are often sent or asked to go to their room and be alone with toys and playthings. Adults retire to a bedroom, a study or even to the toilet. Although it was once common practice, it is no longer thought admirable to lock a child in a dark cupboard. In his own room, he gets comfort from his toys, just as an adult will soothe himself with a book, a pet animal, possibly with music, or just by being alone.
The mentally ill person, who has had a rupture of interpersonal relationships, likewise needs space under his own control where he can “pick up the bits.” The best place would be a room of his own, with familiar furnishings and his personal possessions easily visible. Wherever his retreat, it should give external stimulation as well as support and comfort.
Bare, Drab Rooms Affect Perception
Seclusion rooms in many hospitals are built to some stereotyped plan, and are poorly-lit, bare, drab rooms of a curious cube-like construction which makes them seem unduly high. There is little or no furniture, often only a mattress. Walls are usually tiled in one color only, and this sometimes white. Windows covered with heavy screening, ceiling lighting often high and remote beyond the patient’s control, heavy imprisoning doors sometimes the same color as the walls, and in the middle of the floor a brass grating over a drain hole―no wonder these rooms are suggestive and frightening. Such rooms strongly resemble the reduced environment described by Hebb* in which even well people can experience major 18 changes in thinking,. perception and mood, larked in certain non-experimental situations, notably brain washing, such environments are deliberately used. to. encourage alterations in perception. Surely then it is un-wise to place psychotic people in a situation which, since it will not afford them even minimal external stimulation, is likely to increase the perceptual disorder which many of them already have.
The need for sufficient stimulation, particularly of a visuo-auditory type, combined with carefully selected tactile and olfactory stimulation, is strongly suggested by Goldfarb’s recent work at the Ittleson Family Center with children. His work indicates that many schizophrenic children tend to inhabit a tactile-olfactory world, rather than the more common and culturally acceptable visuo-auditory one. It seems probable that schizophrenic adults may be in much the same position.
Clearly then we must provide our disturbed patient with an adequate amount of pleasurable visuo-auditory experience while in seclusion, and also let his environment be rich in socially acceptable tactile-olfactory pleasures, lest he seek the only remaining gratification―tactile-olfactory ones from his own body. Specifically, let us imagine a patient, greatly disturbed, shut up in a bare room, with bare walls, little or no clothing, and possibly only a mattress or blanket as furnishings. The visuo-auditory and tactile-olfactory enjoyments to be obtained from such surroundings are very small. Is it surprising, therefore, if his seclusion results in apsophilic (auto-erotic) activity, in the tactile experience of staff members or even in reviving a tactile and olfactory interest in his own body products of urine and feces?
These apsophilic activities, the touching and snuffling on the nursing staff, and the handling of feces and urine are likely to produce great anxiety and great resentment in those who must care for the patient. He will naturally interpret this as dislike and rejection, and a vicious circle is established. He is driven deeper and deeper into his tactile-olfactory experiences, and probably also into full hallucinatory experience. Since we are woefully short of really sophisticated staff, we must make .very vigorous efforts to see that this type of “reduced environment” seclusion is banished from the mental hospital as quickly as possible.
The seclusion room, therefore, must be not merely pleasant, but the very best room on any ward. There are several reasons for this. For one thing, if the room is pleasant, it will take away the idea of punishment―not merely by a verbal gesture, but by a change in the attitude of everyone on the ward, patients and nurses, who will both be far more impressed by the fact that the seclusion room is the best on the ward than if there is simply lip service to the effect that seclusion is not punishment. Money invested in making this room conspicuously better than other rooms “because it is for those who are the most unwell” will indicate to both nurses and patients that the hospital particularly concerns itself with those who are the sickest. The fact that the room is an object of pleasure and satisfaction to all the patients on the ward will exert considerable pressure on the disturbed patient to use this joint possession properly. This pressure will be extremely effective in preserving the room from damage.
Dimensions and Decor Important
What, then, should this “best room in the ward” be like? Particular attention must be given to its size and proportions. A small room of great height is extremely oppressive to most people. and if such a room must be used, perhaps a false ceiling should be built in. The lighting must be good, and must, at least in part, be under the patient’s own control. The walls should be pleasantly painted in bright and reassuring colors. There should be pictures on the wall, and a mirror (a metal or unbreakable mirror is permissible). The bed should be comfortable and the bed cover pleasant. Sheets, pillows and mattress must of course be provided. There should be chairs and a desk, the chairs self-colored and if possible, textured. Patterned material is best avoided, since it may have a disturbing, Rorschach-like effect. (Until we know more about the effect of patterns on patients’ perceptions, we should be cautious about patterned materials.) A carpet or rug, preferably nylon, should be on the floor, which may be of tile or linoleum, but should be light in color. To avoid uncertainty about the passage of time, a clock and a calendar should be clearly displayed. If a toilet cannot be readily available, a modern commode chair may substitute, if it is explained to the patient.
It is important here, as elsewhere in the hospital, for the furniture to be light, strong and elegant, rather than heavy or cumbersome. Heavy furniture quickly becomes a challenge to some patients to see if it can be broken. It encourages all patients to lose one of the most important skills which we all acquire in childhood―the ability to maneuver through complicated mazes of furniture. This ability includes all sorts of skills, especially subliminal psychomotor movement. Mental patients frequently lose this ability through disuse, and all too often the arrangements in the mental hospital give them no opportunity to re-acquire it, or what is even more important, to correct early the tendency to lose it. Experimental work shows that, given the opportunity, people frequently correct perceptual errors on their own. But a bare room, fitted with one massive piece of furniture affords neither encouragement nor motive for correcting an error of any sort.
In the seclusion room, the patient should have diversions from the very start. Games, books, perhaps a slide projector, a television or record player under his control are all possibilities. Cut flowers and potted plants should decorate the room. Writing materials should of course be available, and if the patient has difficulty in writing, as some psychotic people do, he might be provided with chinagraph (grease) pencils and an ample supply of paper. Part of the wall might be processed for drawing. which people sometimes find pleasant when they are upset. Plasticine and paint should be provided. A way might also be devised for the patient to brew his own coffee or tea. A tape recorder could be provided to allow the patient to hear his own voice, and get accustomed to the fact that he really is there, though this should be handled with caution, because some people find it rather a disturbing experience.
All these measures must, of course, be combined with friendly interaction with a member of the hospital staff, one with whom the patient feels comfortable and can speak freely, but who, like the room itself, will keep him as close to reality as possible.
In brief, the seclusion room is ideally a place where the patient, after a rupture in interpersonal relation-ships, can re-assert his adultness and recover his poise, rather than a place of punishment where he is treated like an abandoned child in a dark cupboard or a bear in a pit.
(See link to original article for photo of music therapy session.)
*Dr. Donald Hebb, McGill University, conducted experiments in which the subject was placed on a bed in an air-conditioned box with arms and hands restrained with cardboard sleeves and eyes covered completely with translucent ski goggles. Hallucinations and delusions of various sorts developed, mostly in those who could stay longer than two days. Many subjects left at about twenty-four hours
http://journals.psychiatryonline.org/data/Journals/PSS/20510/18.pdf
Pencil Art done under Barbaric Conditions at Hospital of Central CT: Brutal Aversive Conditioning.
CLICK ON THE PICTURES TO ENLARGE THEM.
There were few rewards for behavior that toed the line at New Britain General Hospital (HOCC). Mostly it was punishment. If I was found with even a stub of a forbidden pencil, I was carried off to the Supermax seclusion cell, stripped naked and left alone.
At that point, being teeth-chatteringly blue with cold, I would swat a nurse in such a way that she would feel assaulted and bring on the goon squad of “I want to hurt someone today” guards to put me in four point restraints.
Why would I induce this? Because then they would at least cover me up afterwards with the mercy of a sheet, for modesty not warmth mind you, and I would beg for a blanket in vain. But at least my body would be protected from head to toe from the blasts of the A/C up full bore, and I could rest after I had had screamed out my lungs and my despair for a lonely twenty minutes or more.
No one cared, no one heard or paid any attention. The doors were double, and the cell was utterly soundproof. NO one ever even knew I was locked in there. When my screaming was too heart-wrenching for the softer ones of the staff down the hall in the room where they had retired to, they simply turned down the monitor and intercom so they didn’t have to listen.
I know, because I heard when the telephone rang, telling the person sitting outside the inner door they could turn it back on now (after I had quieted down). This was brutality of the nth degree. But they always called it treatment for safety, though I mentioned the CMS regs to the security guards one day as they were inflicting their usual pain in order to bring me to the room, and they stopped in their tracks.
“You’re kidding,” one said, “Its true that the only legal reason for seclusion is Imminent Danger to self or others?” (I had been brought there for disturbing the peace…)
I nodded, Look it up. She looked gravely at the others. but proceeded o do what she had been ordered to do anyway. And I proceeded to behave in a wildly immodest and terrified fashion likewise…knowing I would be left alone and freezing for at least two to three hours, no matter how fast I calmed myself.
They didn’t care. it was PROTOCOL…




Hospital Of Central CT: Smearing Shit at W1: An Angry Poem but an Honest one.
HOLY SHITE AND URINE TEAM
Her cool wordless RN face expresses nothing
as she scoops the ice cream turd and quickly disinfects.
But I think for her, thinking, knowing this:
“Asshole, shithead, you think
your shit don’t stink…” While I have no working sense of smell,
I know I’m an unofficial pain in the ass here
because no one can be officially PIA
on a psychiatric ward, not even I, the wild shit smearer
who knows no disgust first hand
for not smelling it.
What I know well and sadly is
the consequences of disgusting others,
the distancing, the shunning,
how killing the ultimate loneliness is, double-locked away
in a soundproof seclusion cell.
Shackled naked into leather 4-point restraints, I shriek my soul away,
from the bottom of my lungs for 20 minutes straight.
The illegally silenced intercom remains dumb.
Even the 1:1 monitor positioned behind the door.
peering lazily through the judas-eye of a small plexi-port-hole,
doesn’t really pay attention. Why bother, the shit smearer
gets what she deserves.
Oh, I know I disgust them, what with my out of control turd throwing
and my illegible scribbling with my feces on the wall
but they refuse me so much as a marker and board,
and they won’t sit down to listen when I speak.
Mute for 16 days, I will be heard now, one way or another.
But this is no way to think, and i think without thinking, just do with do do, mindlessly, enraged by trauma.
I foul myself because no one cares,
because their disgust is threaded, even so heat-felted with hatred
they have long forgotten I’m just another patient
with problems bigger than the shit I fling.
Instead, cucumber skinned nurses sneer their disgust,
Bad dog! Bad, bad dog!
But I know dog is just God spelled backwards.
And God created the living world
from dust and mud and excrement.
I am no god, I am Live backwards to Evil:
I create chaos from utter chaos within.
There are always turds to form and fling.
And in the end all they can do is kill me.
Fuck me! Do me a favor you turds, kill me!
But first, you have to silence the hate on your faces,
clean the smeared walls,
and pretend I am nothing to you.
When you came in to take me down,
restrain me for any excuse, even for just wanting a blanket.
you had to breath in my shit, that fear,
and knew what it could do to you.
You’d heard the stories, deadly E-coli, C diff.
Something in me might kill you,
I don’t know what scared you more, my wildyelling
or my excrement.
That was always the struggle. Shit stinks. I stank.
You hated me for my smell. You feared me for what I did.
I know your fear. It was: what would happen if you
lost control of yourself.
Would you, control freaks,
too dance naked in dung?
Article From New Haven Register On Connecticut’s Excessive Use of Restraints, With Full Commentary…
FROM: THE NEW HAVEN REGISTER May 31, 2014
Connecticut hospitals restrain psychiatric patients at double national average

As Connecticut works to improve its mental health system, new federal data shows that hospitals in the state restrain psychiatric patients at more than double the average national rate, with elderly patients facing restraint at a rate seven times the national average.
In addition, the state lags behind in providing adequate post-discharge continuing care plans for psychiatric patients, especially teens and the elderly. Connecticut’s 28 inpatient psychiatric units and hospitals developed continuing-care plans for fewer than 70 percent of patients they discharged from October 2012 to March 2013 — indicating that thousands of patients may have left facilities without adequate treatment and medication plans.
A C-HIT analysis of the federal data, released by the Centers for Medicare & Medicaid Services for the first time, shows that Connecticut ranks in the top fourth of states (11th highest) in the use of physical restraints in inpatient psychiatric facilities — and is the third highest state in restraining patients 65 and older.
Two psychiatric units — at Bridgeport Hospital and Masonicare Health Center in Wallingford — have the 10th and 12th highest rates of restraint use, respectively, among the 1,753 psychiatric facilities nationwide that are included in the federal reports, which cover October 2012 through March 2013.
State and federal guidelines — tightened over the past 15 years, partly in reaction to deaths in Connecticut facilities — say that restraints should be used only in cases of imminent physical danger to a patient or others. They call for less restrictive interventions when patients are acting out aggressively.
But the data show that Bridgeport Hospital, Masonicare and three other Connecticut hospitals — Waterbury, Hartford, Danbury — restrain patients at more than triple the national rate.
James McGaughey, director of the state Office of Protection and Advocacy for Persons with Disabilities, said he was disturbed by both the high rate of restraint use and the low rate of post-discharge plans.
“The numbers are pretty compelling,” he said. “Some of our hospitals have done a significant amount of work on this, but clearly there’s more to be done.”
He suggested that the Department of Public Health, which oversees hospitals and is charged with reviewing annual reports of restraint and seclusion, should “get a little less timid in looking at this.” Hospitals rarely have been cited or penalized in recent years for improperly using restraints, a review of inspection reports shows.
McGaughey noted that the state-run Connecticut Valley Hospital in Middletown has pursued a reduction in restraints and seclusion that has cut its restraint rate significantly in the last five years. The new data show CVH’s rate at .52 hours per 1,000 patient hours — below the statewide rate of 1 hour per 1,000. The national average is .39.
“It’s ironic that our one remaining large state hospital has done such a good job of reducing restraint and seclusion, but you have some very different results at private institutions,” McGaughey said of CVH, which was cited for excessive restraint use in 2007 by the U.S. Justice Department. “What it shows is that it’s possible to address this issue, but you need leadership to effect this kind of culture change.”
Mental health advocates say seclusion and restraint should be avoided because they are traumatic and dangerous to patients and staff.
Alternatives include individualized aggression-management plans, the use of “comfort rooms” or time-out spaces, and one-on-one interventions. Among the innovations at CVH are 22 “comfort rooms,” designed to calm agitated patients, and a reduction in the time interval that a physician’s order of restraint or seclusion can remain in effect, according to a state report.
Yale-New Haven Hospital has a restraint rate of .36 hours per 1,000 patient hours — just below the national average of .39 hours. But its rate of developing care plans for discharged patients is relatively low — 50.36 percent, compared to a national average of 73.5 percent of cases.
Officials at Connecticut hospitals with high rates of restraint say they are working to reduce those incidents, and they stressed that even minimal mobility restrictions, such as soft wrist restraints or brief therapeutic holds, are counted in the federal numbers.
Robert Bernstein, executive director of the Bazelon Center for Mental Health Law, a national advocacy group that successfully sued Connecticut in 2006 to stop housing psychiatric patients in three nursing homes, said he worried that progress made in the early 2000s to reduce restraints might be slipping in some hospitals because of staff shortages and “pushback” from clinicians.
“Some of the procedures put in place may have been weakened, because it’s a lot of work” to use alternative interventions, he said.
Although patients subjected to improper restraint can file complaints, few speak out, Bernstein and others said. Among the exceptions in Connecticut is Pamela Spiro Wagner, a Wethersfield writer and artist with schizophrenia who has cycled in and out hospitals.
In an April “open letter” to the director of a Connecticut psychiatric hospital, Wagner readily conceded that she is a difficult patient — “easily roused to irritability and hostility” — but insisted that her behavior has not warranted her repeatedly being placed in restraints and seclusion, for hours at a time.
“Once you allow staff to use restraints a little, it only takes a little to use them a lot.”
CONNECTICUT VS. THE NATION
Nationally, the states with the highest restraint use are Minnesota, Washington, South Dakota, Tennessee and New Hampshire. For patients 65 and older, only Nevada and New Hampshire have rates higher than Connecticut, which restrains elderly patients at an average of 7.69 hours per 1,000 hours. Thirty-five states have rates of less than 1 per 1,000 hours; the national average is 1.01 hours per 1,000 hours.
The U.S. facility with the highest restraint rate is Park Ridge Health in North Carolina, which reports 722 hours of restraint use per 1,000 patient hours overall. Among facilities that report serving children ages 2 to 12, Lakeland Regional Medical Center in Florida has the highest restraint use, at 200 hours.
The federal data shows Connecticut psychiatric facilities fare well in some categories, including lower-than-average rates of restraint for children and teenagers. Five hospitals reported no use of restraints for any age group: Sharon, MidState Medical Center, Bristol, John Dempsey and Natchaug hospitals.
And Connecticut’s rate of keeping patients in seclusion is lower than the national average, with half of the state’s psychiatric facilities reporting that they did not use seclusion at all. Nationally, South Dakota, Montana and Washington report the highest use of seclusion, defined as involuntary confinement where a patient is prevented from leaving.
But the state’s over-65 restraint rate is fueled by excessive rates at Masonicare (35.99 hours), Bridgeport Hospital (37.92) and Hartford’s Institute of Living (9.19).
Officials at those hospitals say they have taken steps in the year since the data-reporting period ended to reduce restraint use.
This is the first time that quality measures from psychiatric facilities have been made available by CMS. The federal agency does not penalize facilities for high rates of restraint or inadequate discharge plans. Instead, an agency spokeswoman said, the public reporting is intended to encourage quality improvements and help consumers to make informed decisions.
At Bridgeport Hospital, Dr. Ryan O’Connell, vice president for performance and risk management, said the hospital’s geriatric psychiatric unit serves many patients with dementia and behavioral problems that cannot be managed in other facilities. About 18 months ago, he said, the hospital put in place an “action plan” to reduce restraints, including using “comfort” rooms. Also, in January, a new policy was implemented requiring that the nurse manager be called before any patient is restrained.
“We realized we were going in the wrong direction with restraints” and have since seen a “dramatic drop” in their usage, O’Connell said.
Hartford Hospital’s Institute of Living (IOL), which has a geriatric unit for complex dementia patients, has made similar changes over the past few years, nursing director Ellen Blair said. She said restraints are now rarely used, and only for patient safety. The IOL requires that a physician’s restraint order be reviewed every two hours, rather than every four, which is the standard of care.
“We look at our data every single day” to ensure that restraint and seclusion are being used only as “a last resort,” Blair said.
Masonicare’s acute psychiatric unit serves geriatric patients who frequently are referred because of difficult behaviors and aggression, said spokeswoman Margaret Steeves. When restraints are needed, the hospital uses “the least restrictive restraint, which is typically a seat belt,” she said. Masonicare has an interdisciplinary team reviewing restraint use.
Statewide, the Connecticut Hospital Association has been working with the state Department of Public Health to minimize the use of restraints, said Dr. Mary Cooper, the group’s vice president and chief quality officer. She said the new federal data “indicate that there is more work to be done in this area” and will help to identify best practices.
Nationally, the federal government tightened rules on the use of restraints and seclusion between 2001 and 2007, including time limits on physician orders and strict documentation requirements. The changes were prompted by a series in The Hartford Courant, “Deadly Restraint,” which documented restraint-related deaths in psychiatric facilities nationwide.
In 2007, the U.S. Department of Justice cited the state-run CVH for excessive overuse of unnecessary restraint and seclusion. Since then, policy and training initiatives have significantly reduced restraint episodes — from 26,290 hours in 2000, to 529 hours in 2012 — a state report shows.
State DPH spokesman Bill Gerrish said the agency collects restraint and seclusion reports from hospitals and works to “ensure that care is appropriate.”
LAGS IN DISCHARGE PLANNING
McGaughey and Bernstein said they were especially troubled by the failure of many hospitals to develop continuing care plans for discharged patients, and to transmit those plans to the next level of care.
Statewide, Connecticut facilities developed adequate discharge plans 69.4 percent of the time — lower than the national average of 73.5 percent. For teens, hospitals transmitted care plans only 55 percent of the time — lower than the national average of 74 percent — and for seniors, just 42.7 percent of the time, below the national average of 56 percent.
Discharged patients are supposed to receive care plans containing their diagnoses, reasons for hospitalization, medications and treatment recommendations.
The federal data shows that 10 Connecticut hospitals, including Waterbury Hospital, Masonicare and Yale-New Haven Hospital, properly transmitted care plans to the next provider in less than half of cases.
A few hospitals — St. Mary’s, Bristol, Norwalk, Natchaug Hospital and Southwest Connecticut Mental Health — transmitted care plans more than 90 percent of the time.
McGaughey said that without continuing care plans directing further treatment, many discharged patients may languish in nursing homes, shelters or land back in the hospital.
“The lack of continuity of care, to me, is a huge issue,” he said. “It’s a pretty brutal business — insurance companies want you to medicate and discharge as fast as possible. The question is, what happens after they’re out?”
Bernstein said the lack of attention to continuing care plans was “jaw-dropping.”
“Those numbers should be at 100 percent,” Bernstein said. “It’s shameful.”
Hospitals with low rates of discharge care plans blamed much of that lag on their failure to document that the paperwork was done.
At Masonicare, for example, Steeves said the 31.3 percent rate of developing care plans was due to problems with the “tracking of the discharge document . . . not that it wasn’t actually sent.”
This story was reported under a partnership with the Connecticut Health I-Team (www.c-hit.org).
COMMENT:
This is the comment that I posted online at the paper a few days after the article was published, (as it happened, while I was a patient being tortured at the former New Britain General Hospital, the present day, Hospital Of Central Connecticut).
Pamela Spiro Wagner: “As someone who has been subjected to more use of seclusion and four-point restraints over the past “decade of change” than in the two decades previous it boggles my mind that anyone would even dare to state that things are improving in CT mental health care institutions. During my nearly month-long captivity in the winter of 2013, the Institute of Living in Hartford regularly restrained me to a bed for as long as 19 hours at a time, without ever releasing me for so much as a bathroom break — I had to defecate in my clothing. I was not even released to eat. When I was not in four point restraints “for not following directions, I was in seclusion, which they called the “Quiet Room” and not seclusion, but by CMS definitions, it was seclusion as I was separated from the rest of the patient population by force, and was not permitted to leave the room I was isolated in.
The one time I did actually saunter away, walk down the hall to look out the window, and return to my non-seclusion Quiet Room, I was punished with immediate use of four point restraints, into which I was placed without a struggle, hoping that would make it easier to win my freedom. Alas, for me, there was no way to earn freedom from restraints I never “deserved.” The entire point was discipline, and that would last as long as the staff wanted me to be in shackles to learn my lesson. There was literally nothing I could do, –stay calm, sleep, quietly ask for release — nothing, until they were finally satisfied that I was submissive enough to obey their orders, some 6-19 hours later. But I had to cry Uncle, and submit to a set of degrading humiliating “debriefing questions” that assured them that I took responsibility for my own being restrained and that my behavior would henceforth conform to their norms.
I was surprised to see Natchaug Hospital being given good ratings of any sort. One of their chief psychiatrists on the Adult Unit, a longtime presence their Emeritus psychiatrist you might say, was so insouciant about this job as to be nearly incompetent, but probably hard to fire even for negligence. HIs name I will not mention. He routinely did drive-by visits with his patients– a wave in the hallway might not be a completely standard morning meeting, but it happened often enough that peatients knew that would be all of this doctor they would see for the day. He routinely discharged patients with GAF scores at or around 60, the highest “global assessment of functioning” that one can have and still be rated “disabled” — not because he knew this level of functioning to be the case, but because it made him and his psychiatric ministrations at Natchaug look good. After all, if person comes in with a GAF in the 20s, and barely able to function, and you discharge him or her a week or two and some drive-by counseling sessions later with a GAF of 60, you must be doing a terrific job, esp for a 75 year old doctor not too keen on using anything like trauma-informed or patient-centered care. I had never left a hospital before Natchaug with a GAF higher than 40, but suddenly I rated a 60….by a doctor with whom I never spoke.
Natchaug Hospital, when the nursing director was Sharon B Hinton, APRN, was a decent place, because she made certain that abuses like restraints and seclusion rarely to almost never happened under her watch. I know, because I was there about three times during her administration. I also knew her when she was Hartford Hospital’s psychiatric Head Nurse at CB-3, where she and her never failing humanity and respect for the dignity of every patient made all the difference in the world. I might have come from an abusive hospital in the early 90s, like University of Connecticut’s Dempsey Hospital, which in those days four-pointed people to an iron bedstead, by shackling them spreadeagled to the four corners of the bed, a stress position that is not just tantamount to but is in fact torture. But I would be rescued by someone finding me a bed at Hartford Hospital, where Sharon would discover me arriving there in tears and tell me, unfailingly,”Its not you, Pam, you did nothing wrong, It is the hospital that treats you badly…We don’t have any problem with you, because we treat you well and you respond to it. When they treat you with cruelty, you respond badly…That’s very normal.”
But as to Natchaug…Bravo if they have done away with restraints completely. They had not done so when I was there last in 2012. Nor with seclusion, which was imposed in mostly a disciplinary and arbitrary fashion. Largely it was used to force medication on loud obstreperous patients or for angry fed-up senior nurses to take out their peeves on patients they didn’t particularly like (e.g. me). I still remember one APRN demanding that I be dragged to locked seclusion, and left there alone (despite all Sharon’s previous assurances that such would NEVER happen, that someone would ALWAYS remain in that room with me if I ever ended up there.. Alas, Sharon had left by then, so rogue nurses like D could have their way…) and when I peed on the floor in panic, and took off my clothes they rushed in to take them away from me, and inject me with punishment drugs, then made me stay for an hour alone on the pee-soaked mats, freezing cold, pretending to sleep and calm myself just to convince them I could leave and not bother anyone. I managed to do so, or at least the APRN D. got over her fit of pique and finally released me, but I was not really calm, and when they finally draped two johnnies over my naked body so I could decently traverse the distance to my room, I left, disrobing as I went…Who gave a damn about my flabby flat behind? I certainly did not. And it served them right if everyone got an eyeful…served them right..
Natchaug’s biggest problem was and probably still is a lack of staff cohesiveness and bad morale between the staff nurses and the well-educated techs/mental health workers who were all very dedicated college grads but were treated like grunts…The MHW’s did most of the important patient contact, but were not trusted to write patient notes, or the notes they wrote were never read, or accorded any import. This was not just despicable but very unfortunate in more than one instance during my stay, as the notes they took personally might have saved me from some terrible misunderstandings and outrageous misdiagnoses that harmed me terribly..
Most places use techs who are trained by shadowing for a day or two, which means, badly trained, if at all…
You have to take all such in-hospital diagnoses with such a heavy grain of salt, you know, even when they are labeled with the words, “THIS IS A LEGAL DOCUMENT.” Because they get so much of fact-checkable, factual material garbled that you cannot believe a word it says. And as for diagnosis, well it is all of it opinion, one, and two, it depends largely upon whether you are a likable patient or a disliked one, what they finally say about you on any given day. No one should have that sort of power over another human being, frankly. And the idea that they can brand one for life with certain psychiatric diagnoses just sickens me.
Be that as it may, my recent last experience was beyond the beyond, at Hospital of Central Connecticut, The old New Britain General…and I expect to go back to talk to someone there about it. I always do And I have much to say to them, after the pain and rawness have worn off a little. They considered it SOP to strip me naked and leave me alone in a freezing seclusion cell without any access to human contact, unless they chose to speak to me over a loudspeaker hidden in the ceiling. If not, I was utterly abandoned, no contact or even view of another human being for as long as they wanted to keep me secluded. They also restrained me, having male security guards four-point me stark naked to the bed, before they had the decency to cover me with a light sheet, even though I begged for a blanket for warmth. (A nurse manager came in and shivered, saying “Brrr its cold in here!” but did they relent and let me have a blanket…No, clearly I was not human, didn’t need warmth.)
This is just the tip of the SR iceberg in CT in the current years, Remember this is happening right now, not ten years ago, or before the so-called reforms. Nothing is getting better. Things are worse than ever, And when you are a patient in these hospitals, you have no help, no recourse, anything and everything can be done to you and you have no way to refuse or say “no”. No one will help you, or offer assistance. They can just grab you and seclude you or restrain you without your having the power to stop them or any recourse to make them pause and reconsider. You are powerless to stop anything…And so they get away with it every time. And once it is done, who will fight for you? What lawyer will take your case if the guards hurt your shoulder rotator cuff, or bruise you up, or degrade or humiliate you? No one….so you are deprived of your human and civil rights, completely, but the hospital knows that no one cares enough to fight for you, so they get away with it each and every time, and they know this when they do it. They have nothing to worry about,….You are just another mental patient, a nobody, a nothing.
That’s what you are if you are diagnosed with schizophrenia and hospitalized in CT hospitals in 2014. A nobody that the hospitals can abuse with impunity and will. Just wait and see if any of this changes…I doubt it highly. They have no motivation to change. They don’t think they are doing anything wrong now.”
Open Letter to Harold I. Schwartz, MD, Psychiatrist and Director in Chief of the Institute of Living at Hartford Hospital Behavioral Healthcare
April 16, 2014
Dear Harold Schwartz, Director of the Institute of Living at Hartford Hospital
I believe that I was profoundly harmed by the treatment I received in 2013 on Donnelly 2 South at the Institute of Living at Hartford Hospital, and that what the staff did to me was not only unethical and cruel but that it crossed the line into illegality from the very first. Psychiatric patient abuse is a pattern in Connecticut hospitals, but it was most egregious at the Institute of Living because the staff told me that they knew what they were doing was wrong but that they would get away with it anyway.
That I know I was a difficult patient never justified staff behavior towards me. I was loud and upset and hard for them to deal with, yes. That is precisely why my Psychiatric Advance Directive (PAD) was written out the way it was, and why I made my medical and psychiatric history online so available. When ill, I am frightened and paranoid, which makes me easily roused to irritability and hostility. I know this, from a distance as it were. But knowing this now does not mean I was in control of my emotions. I am by nature neither temperamental nor prone to temper eruptions or throwing things. In addition, I am extremely modest, hardly one to disrobe or urinate in public. My friends and family have at times variously labeled me “stoic” and “peacemaker,” which should tell you a lot. But that I disrobed and urinated on the floor on Donnelly 2 South both horrifies me and concerns me because these behaviors point to something going on distinct from my psychosis: they point to my having been subject to abuse and trauma at the hospital itself.
Let me make it very clear that if I have behaved in such ways before it was only in response to similar extreme circumstances – as when i was subjected over and over to restraints and seclusion in a horrific and sadistic fashion at Manchester Hospital in 2009 and similarly at Middlesex Hospital in 2010. It is too bad that when Sanjay Banerjee MD and Amy Taylor MD took it upon themselves to violate my HIPAA privacy rights and investigate my previous admissions, without my permission (which I expressly refused to grant) they failed to make the connection between the abuse, and my subsequent behaviors…It turns out all they drew as a conclusion was that if those hospitals could use restraints and seclusion ad libitum, so could they. It didn’t seem to matter to Dr Taylor in particular that in 2009 and 2010 measures such as seclusion and restraints not only didn’t work, they made things worse. Not surprisingly, when Dr Taylor followed these examples I regressed completely, just as my PAD predicted.
I was admitted to Donnelly 2 South, and I came in with a very detailed Psychiatric Advanced Directive as I said. I made it very clear that my online electronic medical record was also available. It included documents such as my narcolepsy diagnostic consult and special documentation assessing my need for a higher than usual dosage of Ritalin, written by my former sleep specialist, Mary B O’Malley, MD PHD who was also my psychiatrist from 2000-2009. Included as well was a letter she wrote to my present psychiatrist, Dr Angela Cappiello, explicitly stating her conviction that I do not have a personality disorder, NOS, borderline traits, or otherwise.
According to Dr. Sanjay Banerjee he read every page of these documents. That is what he told me. He even praised me, saying he wished every patient would come so prepared. Moreover, when he spoke with Dr. Cappiello, he brushed off my concerns about anyone misperceiving me as having a personality disorder. My brother, Philip Spiro, MD, himself a psychiatrist, brought up the same matter when in discussion with Laurie Denenberg, LCSW, but her response was much the same: “Personality disorders are not a part of the picture here. We intend to honor her PAD. We are glad that she has had the foresight to prepare such a document.”
If this was so, then how did it come to pass that Amy Taylor, MD wrote on my history and discharge summary that I have a “long history of Borderline personality disorder” and herself diagnosed “Personality disorder NOS with borderline traits”? I was being treated for four weeks for an active psychotic disorder Axis 1. In any event, she could have no way of knowing whether or not I had a personality disorder, given an active an Axis I diagnosis.
On or around February 4, 2013, I walked in frustration away from the quiet room where I had been held captive for nearly three weeks, strolled down the hall, looked out the window and slowly retraced my steps back to the quiet room, which I had been expressly told was NOT a seclusion room (the definition at Hartford Hospital’s Institute of Living of a seclusion room is a “room to which the door is locked.”) But when I arrived I was confronted by a cohort of staff who proceeded to 4-point restrain me to the bed, even though I was quiet and put up no resistance. Not wanting to give them any reason or justification, I passively lay down on the bed and placed my own limbs out for the restraint cuffs, saying, (I quote my journal entry made later that evening): “For shame. You ought to be ashamed of yourselves. I am not and never was a danger to myself or others.” Their response was “ You refuse to follow directions so we do not know what you will do. This is not punishment, Pamela, this is what your behavior brings on every time.”
From that point on, the threshold for restraints was extremely low. They always restrained me, spread-eagled, so tightly I couldn’t move a muscle. They never permitted bathroom breaks or even used a bedpan, instead they made me defecate in my clothing. They never even let my hands free to eat. I would fall asleep rapidly after three routine punishment needles in the buttocks: Haldol, Ativan and Benadryl—whether I just had my regular meds or not, and they would invent reasons to maintain me in restraints even after I had been asleep for hours. When I woke, groggy and hardly dangerous to anyone, they would grill me with questions that I could not answer. They would then use my inability to respond as reason not to let me out, even when I asked, as the chart recorded, in a “soft sedated voice” for release. They would re-inject me, to put me back to sleep instead.
In the evening on Jan 5th, for the second time that day, they brutally restrained me for throwing half a graham cracker at the wall. Then, as usual, they left me like that for six hours, even after I fell asleep. But in point of fact, though, I could never earn my way to release from restraints by good behavior or quietly, calmly asking for release. I had never done anything to earn my way into them in the first place. I was never violent until they threatened me. They refused to release me until I literally cried, “Uncle” when they told me to.
As to those vaunted “shows of force” what did they expect? Presented with a cohort of threatening staff personnel I saw one thing: an impending assault. I know they anticipated my panic; they said as much in my chart. Isn’t that the point of a planned “show of force” – to induce fear and panic? Why else do it? So why should it be any surprise, when I defended myself when they forcibly, physically grabbed me? When they stuffed me into a body bag and were trying to tighten the straps, surely you can understand why anyone would bite the hand of an attacker whose digits came near the face. I had done nothing but refuse to enter the body bag willingly. I simply was passive. I did not fight or resist until they grabbed my body and assaulted me.
But none of it should have happened. My Advanced Directive explained in exquisite detail exactly what to do and what I respond to better than fear tactics and force. In fact, It is beyond me, knowing that one of the admission diagnoses I came in with was PTSD, how anyone could possibly approve in advance, permission to use restraints and seclusion “just in case they are needed”. Why not counsel the person asking for this advance “right to restrain” to do all in his power not to restrain me and to work with the PAD instead?
Here’s what SAMHSA the substance abuse and mental health services administration publication has to say on seclusion and trauma:
“Studies suggest that restraints and seclusion can be harmful and is often re-traumatizing for an individual who has suffered previous trauma…
“Further, there is a common misconception that seclusion and restraint are used only when absolutely necessary as crisis response techniques. In fact, seclusion and restraint are most commonly used to address loud, disruptive, noncompliant behavior and generally originate from a power struggle between consumer and staff. The decision to apply seclusion or restraint techniques is often arbitrary, idiosyncratic, and generally avoidable.
“Moreover, some studies indicate that seclusion and restraint use leads to an increase in the behaviors that staff members are attempting to control or eliminate.
I have been traumatized, and not just by hospitals. I was date-raped three times in my twenties and experienced traumatic domestic abuse by a long-term roommate. The cover sheet on the PAD made very clear that due to these trauma issues, I could not tolerate being secluded or restrained without serious consequences: regression and serious worsening of symptoms. Unfortunately, as soon as the staff saw fit to use physical methods of coercion and control on me from the first time a staff member grabbed me and pushed me with his lower torso, I ceased improving, and my symptoms went downhill. Did they really think they were being kind and compassionate?
Staff violence begets violence….
I tried to get help even when on the unit, at least I tried when I was free to, to make calls or leave my seclusion… that is to say, forced three -week-long stay in the quiet room last winter. I made many calls to the hospital’s patient advocate office, but the sole time anyone made contact was when the advocate came to hand me some paperwork – I believe I was actually in 4-point restraints at the time — papers I could not read about the forced medication hearing. I needed her advocacy, but she never responded to my panicked calls in any way that was helpful to me. I wanted her help, but she never came by to ask me what I needed. She was less than useful, the fact that I had to go through her, essentially a hospital employee, and her refusal to respond, contributed to my ongoing panic and desperate feelings of aloneness and depression. No wonder Dr. Sanjay Banerjee attempted to force ECT on me, without any prior discussion of it with me whatsoever.
And where did the ECT discussion come from? My PAD states in no uncertain terms that I will refuse ECT under any and every circumstance. My brother would be my conservator if Banerjee had sought to go down that road, and he would never have made any decision to counter my wishes on that subject. If Banerjee really read my PAD, he would have known that. I have already had FORCED ECT and it traumatized me terribly. Also it failed to work.
Banerjee had stopped my 75mg of the antidepressant Zoloft during the first or second week I was there. “Do you really need that?” he had asked, “You don’t seem depressed to me.” Obedient, and in any event glad to get off any medication at any time, I shook my head, assenting to the change. A week later, instead of reinstating the Zoloft, Banerjee blamed my sudden “depression” on my refusal of the anti-seizure medication, Lamictal, a drug I had not taken in 6 months. Now he was applying to force me to take ECT, something I was terrified of, and to have calculated brain damageIt was this threat, and the brutality with which the decision was handed down, that started the downhill course of my IOL stay.
The very next weekday, all hell broke loose. When I entered the conference room, I pushed some important notes across the table that I wanted Dr Banerjee and Laurie Dennenberg to read. They refused, claiming that I threw the papers at them. Instead, Dr Banerjee proceeded to berate me, and told me how he had consulted with other hospitals and providers and had read my records against my instructions and Advance Directive, thus violating my HIPAA rights. Moreover, he threatened me with a behavioral treatment plan that would not permit me to do art or writing unless I “behaved.”
I hit the roof, telling him I would sue the hospital and complain to JCAHO, then summarily left, slamming the door, an act that stemmed from feelings of utter impotence, because I couldn’t actually say in words anything more effective.
It could have ended there. I could have been left alone, to cool down and calm myself. But, no, Dr Banerjee had to write for stat meds again, and even though I was on the phone and trying to find someone to talk to, to calm myself, I had to be physically dragged off the chair I sat on, away from the phone and brought to the floor in a physical struggle (because they had attacked first, i.e. physically grabbed me, I defended myself, instinctually). They could have waited for me to finish the call. They could have waited to see if I calmed myself. I was not hurting anyone or even threatening anyone or myself with harm. All that I had done, in terms of physical threats, was to throw a lightweight chair at the wall. And that, it was clear to everyone, was intended not as a threat to anyone. Furthermore, it was done and over with. I had left that area and gone to my room. I had then come back and now sat on the chair by the phone, speaking to my interlocutor on the other end. There was no need to pick a fight or encourage a struggle. A wait-and-see policy could have successfully guided the situation to a better resolution not only for the situation at hand but for the entire hospital stay. As the poem by Dylan Thomas goes: “After the first death, there is other.” Once they decided to use four—point restraints, there was no going back. The first time broke everything, So they used them again, and again, and more and more freely and without justification but for convenience and punishment.
Back to Feb 5 or 6, after sleeping for six hours, I was taken out of restraints conveniently just in time for a visit from Dr. Angela Cappiello, my outside psychiatrist. Observed by my 1:1 monitor, I only dared whisper and dared not tell the doctor the full extent of the abuse that had been happening. Nevertheless, she took one look at Amy Taylor MD’s behavioral treatment plan posted on my wall, and told me that it would be impossible for anyone, even someone who was well, to follow it properly. She was so worried about me, and about my ability to complete the treatment plan’s requirements, even for the required “24 hours,” that she intervened. The next day, the single day that Dr. Taylor planned to be out of town, Dr. Cappiello asked Dr. Mehendru to evaluate me for discharge, telling her that she feared a power struggle had been set up that I could never win.
When Dr. Mehendru came to see me, at first I was angry, as the chart indicates, thinking she was just another Taylor flunky, preparing to use more restraints and seclusion, But when she asked if I would like to go home, I took one look at her, saw sincerity in her eyes, and burst into a smile, ready to say yes to anything. Miraculously “cured,” I left the IOL that very same day, less than 12 hours after being released from 4-point restraints and not 4 hours out of seclusion.
However, I was not well. Within two weeks time, I was back in the hospital, this time admitted to Yale New Haven Psychiatric Hospital, via their emergency room. Over the next 3 weeks I experienced an entirely different kind of care. At Yale I did not find a staff ready to fight or try to seclude or restrain me.
I was still the same person with the same problems, loud and angry at times, even “violent” to property in my frustration, and still psychotic, yet they never responded with a show of force. Why would they? At Yale it would be absolutely anathema to deliberately frighten a patient. What would be the purpose in that, they would think. They also never pushed me into a seclusion room or strapped me down in punitive 4-point restraints, or any of the other ill-advised responses that my PAD explains are the worst things to do to anyone who is struggling, scared and paranoid. In point of fact, Yale Psychiatric Hospital’s Washington Square unit does not have a seclusion room. They also have a “restraints-free” policy, so they didn’t use those at all either.
The Institute of Living on the other hand with its “We only use restraints and seclusion if we have to” policy, restrained me countless times, and for many more hours than was even legal. When I woke up that last morning, the room opposite me was occupied by yet another person in 4-point restraints! That is because once you allow staff to use restraints a little, it only takes a little to use them a lot. And once you sanction the use of restraints and seclusion at all, it is only time before someone abuses them and abuse becomes the norm.
I would like your response to this letter, I have sent it to many people within the state government and outside of it, But you may have the first response. Also you may be interested in the youtube video of my artwork which can be found at this site:
Prior to when you allowed the staff to body bag and restrain me, when I had done nothing wrong but leave the non seclusion quiet room, and you refused to come to my assistance, you had asked to see my artwork. Instead you left me to be tortured. Well, here is some of the art you might have seen had you rescued me from my abusers.:
Sincerely
Pamela Spiro Wagner
The final one you never saw in featured in the post below this one.
YouTube Video: Mental Hospital Treatment and Abuse -Reality in Art
This time you should be able to view this on an Iphone or Ipad.
Original Art: How NOT to Treat Schizophrenia: with sound
Trying again…
Still not playable on ipads or iphones, not sure why. I think the sound will work. for what its worth…
Youtube video with sound available for all devices here:
How Not to Treat Schizophrenia or any other Mental Illness: Slide Show
No music or sound, sorry. Best viewed in small screen as the conversion to Quick-time made the files smaller and hence less crisp when seen on a large screen…I’m sorry but this doesn’t seem to be viewable on an ipad..Dunno about android devices. At least I notice that the controls are unavailable on my ipad at any rate…Will try to find another format that will work and re do it…SO SORRY!
Youtube video with sound here :
In 4-point Restraints for Disobeying the Rules at the Institute of Living, 2013





So that is all I have to post today as I have too many errands to do before my meeting at the Institute of Living. Wish me luck everyone! I don’t expect much from them, I must say. Not much at all, after all, no one is going to acknowledge any wrong doing, much less apologize or even want to improve the situation. Not as at Natchaug where at least they gave lipservice, though it turned out to be lip service ONLY…to wanting to make Natchaug a better place. (Yeah, it turns out they — THe MFs at Natchaug Hospital who said they wanted me to speak — were just stringing me along, never did have any intentions of having me back to speak to the Medical staff, just mollifying and mollycoddling me as I sort of thought they were…Dr Deborah Weidner, the Natchaug Hospital CMO, is a politician as much as a psychiatrist and has to be, right? NO…but that is another subject altogether. I won’t be going back to Natchaug ever again either , not as a patient, as was understood. They don’t have a doctor who will see me, so why would I care about helping them improve? I did care. I do care about all their other patients and I care about their Mental Health Workers, who were the one group that really did do their jobs…and most of the nurses too…But the problem is the Admin of Natchaug doesn’t care, and the senior nursing staff is burned out and problematic…But I am not going to go there. Because THEY DON’T CARE that I care!)
Anyhow, as I said, I have errands to do and I guess I should maybe wash before I go to the IOL, seeing as how I haven’t done so since my trip to NC…It might be a good idea, though a real drag. I hate it…I hate the very idea of getting under the running water and getting wet is such a hassle. But gotta keep up the appearance for today! After that, who gives a damn…
Okay, so thats it for now. I’m outta here. Thanks for all the FB support, guys. I will let you know how it goes.
My Psychiatric Advanced Directive — IGNORED at the Institute of Living at my Expense
These are the first two pages, including a note from the cover page, of my very very detailed Psychiatric Advanced Directive, and I think you will see why what happened at the Institute of Living, the psychiatric section of Connecticut’s Hartford Hospital, NEVER should have happened. Not only did I bring a hard copy of this PAD, but I wore a medical bracelet with a code for a very complete online medical record, with uploaded documented evidence, both of narcolepsy diagnosis and need for medication, proof from longtime outside mental health providers that I do NOT have “borderline personality disorder,” and other such assistive documents…ALL were soon ignored completely in the effort to discipline and punish me “for not following directions” i.e. not getting better fast enough and speaking my mind to the psychiatrist.
__________________
Prominent NOTE on cover page:
Miss Wagner has experienced multiple episodes of severe psychological and physical trauma. She must NOT be subjected to either physical or mechanical restraints or involuntary seclusion at ANY time. The use of either imposes a serious risk of re-traumatizing and injury, leading to regression and severe worsening of symptoms.
Pg 2.
HOW TO INTERVENE IN A CRISIS:
DE-ESCALATION IS ESSENTIAL
- 1. PLEASE REMEMBER: I can calm down if YOU follow these steps and do not threaten me, order me around, or approach me in anger or in fear.
- I need one person to talk to. I should be approached calmly, by someone who will speak in a kind and respectful manner, understanding that above all:
- I AM SCARED and my anger masks fear. I am not dangerous. I WILL ONLY FIGHT IF YOU ATTACK ME. Please remember that any show of force and people ganging up on me to administer forced medication will be felt as an attack.
- I can be persuaded to take oral medication, usually, if this is negotiated with dignity and kindness and not by means of threats.
- DO NOT ISSUE ULTIMATUMS you won’t back down from…That will push me into a corner and you too, and will serve nothing but to escalate the crisis.
- A calm unthreatening and unthreatened person should ask me calmly and patiently if I can speak in a lower tone of voice, so she can hear me better. Ask me if I can take a deep breath and try breathing techniques that will have flown my head in the moment of crisis.
- Should you have a COMFORT room available, you can guide me gently to it but do not close me alone. Make sure I am warm…
- ABOVE ALL YOU NEED TO BE PREPARED TO LISTEN TO ME. This is not just a matter of forcing medication. Medication may not even be needed if you hear what is going on and what the problem is.
- If you take these simple steps, it is virtually guaranteed that the situation will resolve calmly and without any need to resort to the sorts of violence that would permanently damage and re-traumatize me (or produce secondarily negative behaviors afterwards): seclusion, forcible injections, or mechanical restraints or physical holds.
p 3
STATEMENT TO CAREGIVERS
It is vitally important that you understand that despite a few previous in-hospital assessments, I do not have a personality disorder, borderline or otherwise (you can confirm this with any of my longtime outpatient providers) and that if my behavior seems out of control, it is because I am out of control: I literally do not at the time know what I am doing or why. I am not manipulative or attempting to achieve secondary gain. The fact is I have had tertiary CNS Lyme disease and after positive PCR and Western Blot tests during treatment, I was informed the condition is likely incurable. (Dr ******* of ****** NY, will confirm this.) During the initial illness, my brain developed multiple lesions, visible on MRI, which may predispose me to temporary emotional and behavioral extremes and abnormalities but these are NOT my norm. Anyone who knows me well would confirm this, if you asked them.
You need to understand that I am not always able to communicate the extreme fear I feel, the global paranoia that I experience, but because I feel so threatened and unable to communicate clearly about it I may become very angry at the hospital situation. I am not an angry person. I do have trauma issues, as many people do, which may be exacerbated by being in the hospital.
Please be aware in advance that my “memory in the p.m. for what happened in the a.m.” is often faulty. That is just how it is. When in crisis, I have little ability to recall from moment to moment what happens. This is why it is essential that I be able to write things down. I have lost many years to this amnesia and if I suffer additional trauma it will only make it worse.
I beg of you, do not make assumptions about me. Do not make assumptions about my state of mind. Do not “put two and two together” in your mind without asking me if the conclusion you have drawn is the correct one. You do not know what is inside my head without asking me.
Ascertain whether the information you have at hand is correct. Too many records and hospital charts have been drawn up (because “patient is not communicating”) on faulty information from earlier charts or information gleaned from others but not from me, and the consequences to my treatment have been devastating. PLEASE CHECK MY INTERACTIVE HEALTH RECORD ONLINE at www. — .com Use code ***** to get access.
I have been traumatized by abuse, sexual assault and by brutal treatment in hospitals, from being deliberately choked and given forced ECT to being kept in four-point restraints for several days at a time. So if I experience seclusion or restraints or even that euphemistic obscenity called a “therapeutic hold” it will be devastating and counterproductive. Such treatment invariably leads to increased anger, regression and worsening of symptoms, and my behavior becomes unpredictable afterwards. This is a response to trauma NOT because of any inborn temperamental disorder. I have already outlined a better way to deal with me and help me on page 2.
I KNOW YOU MAY NOT APPROVE OF POLYPHARMACY. But you need to understand that I must take the antipsychotic drug combination: Abilify 15mg with Geodon 160mg, a TWO-Drug regimen. Monotherapy does not work. I have tried many solo drugs over the course of 4 decades – Thorazine, Mellaril, Haldol, Prolixin, Clozaril, Risperdal, Seroquel, Zyprexa and others – ALL monotherapy has failed.
I will not take any drug that induces weight gain. If you force the issue, know that it will be a useless endeavor because I will stop taking it immediately upon leaving the hospital.
Finally, understand that if I am here in the hospital it is for a reason, and I want only one thing: to get better and be out of here as soon as possible. You can traumatize me and worsen my symptoms and keep me here too long, or you can work with me to achieve my goal, which should be the same as yours. I don’t see any other alternative.
Respectfully,
Pamela S. Wagner
Now, I think that is about as crystal clear as it can be, no? And indeed, Dr Banerjee, my first psychiatrist LOVED it. Said so, and raved about how complete both were, both the PAD and the online medical history which he downloaded, printed out and brought with him to our first consultation. So what happened? YOU tell me! I will write more about what I think happened later. I am still trying to figure it all out.
SISTERS OF NO MERCY
POEM IN WHICH I SPEAK FRANKLY, FORGIVE ME
GOMER: ER-speak for a troublesome, unwanted person in the emergency department, acronym for Get Out of My Emergency Room
So many times gurneyed in by ambulance and police escort
“dangerous to self or others,” and too psychotic
to cooperate or scribble consent, you suspect by now
you are just a GOMER to the snickering scrubs in the ER
who whisk you in back with the other disruptives
lying in beds, waiting for “beds.”
One time you dip paranoid into the inkwell of your purse
extracting a paring knife more amulet than effective protection,
they strip-search you, then, unblinking, eyeball you all night
through a bulletproof plexiglass window.
In the morning, 15-day-papered so you can’t leave,
they send you ominously upstairs.
Later, at home, the voices decree your left leg
should go up in flames to atone for the evil within,
and you listen, and you do it, you do it:
the searing flare of cobalt actually crackles.
This time you tell no one, the char too deep for pain,
until fear of worse trumps your fear of being taken away.
This is not the story of your life.
It’s not the story of your life–
but every time a hulking goon squad clamps restraints
around your flailing wrists and ankles, threatening
to prosecute you for biting those hands that shackle you,
you wonder if there will be any other…
© Pamela Spiro Wagner. All rights reserved (Please note that I request that you do not reblog, reprint this poem or save this poem for anything but personal use. The rest of this blog post may be used if you credit Wagblog properly.)
________________________________________________________
A new reader, Rachel, has had training as a nurse, and is not reluctant to share her insights from the other side of the gurney, so to speak. Her comments have been enormously illuminating to me and contain so much helpful information that I have asked her if I might post them on Wagblog itself so others might have the opportunity to read them “first hand.” I have collected all of the ones here at Wagblog (there are others on my http://www.aboutschizophreni.blogspot.com site) and will try to provide some context for each one so they make sense, if they do not by themselves.
This first comment was in response to my post, AM I CRAZY…Nov 4, 2012 — when I doubted the veracity, of fact if not experientially, of what happened to me at the ED last summer.
Here is what Rachel wrote:
“OH….. Pam. I completely relate to this post…
Is anything more traumatizing than not being able to trust your own perceptions? I don’t think so.
I have so much swirling around in my head that I could say about all this, it’s hard for me to sort it all out, but I will try.
15 years ago I went through nursing school. One of the things that was greatly impressed upon us in our training was the fact that medical charts are Legal Documents – therefore, you must be ultra-careful about what you write in the charts! Also, there is so much charting and other paperwork required, to meet the legal demands of insurance, etc., that it is truly impossible to do the charts “right,” and still find time to do the actual job of patient care. So… just because important happenings are not recorded in your medical chart, that should by no means be taken as proof that it did not in fact happen, in some fashion.
As for that security guard…. sigh… I’ve led a strange life… about 20 years ago, for part of one year, I worked as a security guard in a bank. The security guard who trained me was one very scary dude. All he did was talk about his wonderful collection of guns, and his beloved hobby of shooting those guns, and bragging that he would have made a satisfying career out of being a hit man, if it weren’t for these pesky laws against being paid big money to commit murder! I became so alarmed by this fellow’s homicidal rants and ramblings that I told our boss all about it. The male boss, a retired U.S. Marine, dismissed my concerns out of hand. “People who talk about killing never do it,” he said.
A few months after I left that job, the hit man wannabe shot his fiancée. It was an accident, of course, he having so little experience with guns….
I am so sorry for this latest cruel trauma you have endured, Pam. Just being treated so roughly is enough to put any person at risk of losing touch with reality. As the late Viktor Frankl, MD, PhD, survivor of nearly 3 years in Nazi concentration camps, said in his life-changing book, Man’s Search for Meaning: “An abnormal reaction to an abnormal situation is normal behavior.”
I believe that is probably what happened with you this past July. You were thrust against your will into an abnormal, traumatizing, soul-annihilating situation, which undoubtedly unleashed multiple memories of similar traumatic indignities in the past. You were being treated, not with the kindness and compassion that you needed and deserved, but with palpable disdain. Harsh thoughts and hateful emotions are communicated, far more than with words, via body language, facial expressions, the eyes, the tone of voice, the “vibes” – even a so-called dumb animal instinctively knows when it is not safe, when the people in charge are not to be trusted.
A nurse, concentrating on giving injections in the proper way and in the proper amount, is not going to be paying any attention to what exactly a security guard is doing, or saying. Also, if she realizes after the fact that she gave an injection for which the order had already been cancelled, I am sorry to say that too many nurses, AND nurse instructors, are NOT going to admit that in the chart. I know this, for I’ve witnessed it firsthand. It’s sad, it’s illegal, immoral, and potentially deadly dangerous , yet it is true.
As for having a run-in with a security guard who has a homicidal attitude? I’m sorry to say that they are not at all uncommon, either.
Did your terrified, traumatized mind fill in the blanks with words he did not actually say, as a way to make some kind of sense from what he had done to you? Maybe. But the fact remains that your autonomy, your power, your rights as a human being, were taken away from you, and you were thrust into a terrifying, traumatizing, abnormal situation. For you to be put into such an extremely abnormal situation, particularly in light of all the old trauma memories it undoubtedly evoked in your mind, an abnormal reaction on your part in such an abnormal situation is, really, truly, Normal Behavior.
Rachel
My response to her comment:
All I can say to these things, Rachel, is WOW! I may have to rethink my blog post. Maybe some of what I thought was not delusional but did in fact happen. For instance, I wrote so often that I got those 3 shots. Now I am thinking, maybe i did indeed get them, because why would I pass out so immediately from a mere 20mg of Geodon and 1 mg of Ativan. But with 5 mg of Haldol added it would make more sense.
As for the guard (I refuse to call them security guards as they provide NO security and are in my opinion out of control thugs) I think he may indeed have compressed my neck, if only by holding me down in such a way as to restrain me roughly. Whether or not he intended to strangle or kill me, I dunno. And I have no idea whether or not he said those words, only that they do echo precisely what those nurses said or I hallucinated they said over the hospital PA system about my phone call, which they claimed to have recorded and were also replaying over the same PA system…So if those were the same words, perhaps it was only a hallucination. But perhaps only the words, not the rest of it. Thank you SO very much for validating as much as you have. I truly appreciate your contribution to this site and hope you will continue to offer what you know and have experienced. It is so welcome!
Pam
Rachel’s next comment was in response to my two new artworks: first the Killer Nurse collage, and then the Monet “take-off” of Argenteuil boats at evening…:
…Killer Nurse, HAHAHAHA! When I was in nursing school, a group of my fellow students dubbed themselves (oh you are going to love this): “Sisters of No Mercy.”
They were, too! By the way, I was elected class president by my fellow nurse students, an honor I did not seek out. When I realized by the end of the first semester that I am not cut out to be a nurse, I thought I could not let down my much-younger classmates who had honored me so, by dropping out! Thus I kept slogging doggedly away, and made it through to the bitter end, making all A’s or 4.0s, I’ve forgotten now how we were graded. Then I took the final big test that determined one’s eligibility to get a license, shocked myself by scoring in the top 1% in the entire nation, gave the big Class President year-end speech at graduation, got my diploma, obtained my license, and…. I worked 3 or 4 days as a nurse, hoping to get my money’s worth out of my costly education, but I still wasn’t emotionally cut out to do the hard job of a nurse and I knew it, so I abruptly quit, and let my license expire.
If you have to be a “Sister of No Mercy” to make it in that profession, you can count me out!
Rachel
Then her latest comment is again in response to my blog entry titled AM I CRAZY? and my response to her first comment.
You are most welcome, Pam, I’m so glad my words could help.
I just want to add this, though: most of the security guards I worked with so long ago were very good people. There was only a small percentage of guards who had that scary macho-swagger itching-for-trouble attitude. You find people like that in every segment of the population, as I’m sure you know. But it truly did seem to me that a higher-than-average percentage of such types are drawn to work that allows them to wear a uniform and carry a weapon and push people around. These types are more like children playing at cops-and-robbers, than adults doing a serious job.
On a typical day, standing around in a security guard’s uniform watching the world go by is the most boring job on the planet. When finally “something happens,” these “Make My Day” gung-ho types come alive, and in the worst way.
As for the job of nursing… that’s a very different thing. I worked for a couple of years as a nurse’s assistant, before I finally went to nursing school. Nursing is HARD. Really, it’s an almost impossible job. There are never enough nurses, meaning most hospitals and nursing homes are chronically understaffed, and therefore there is never enough time to get everything done that needs doing. The work is absolutely overwhelming at times. You can work your entire shift at a flat-out RUN and STILL not be able to do it all, and do it “right.” You need 6 hands, you need a stomach made of cast iron, you need a backbone made of steel, and you need feet that can take an unbelievable pounding.
A person can go into nursing with a heart of pure gold, caring and compassionate and empathetic to the max, and the day-in-day-out unrelenting MISERY you see all around you will either kill you, or make you harden your heart in self-defense. As a nurse in a busy hospital, a nursing home, and most especially in an emergency room, the world is one big gaping aching wound, a bottomless pit of sorrow and need, and nothing you do is ever nearly enough. You need to be in 10 places at once, doing 10 different things, and almost everyone demands and criticizes, if not the patients, then very often their family does the complaining.
Stay in nursing long enough, and it is almost impossible to hang on to both your sanity, and your heart. This is why I could not do it! I only worked one week in an emergency room, this was as part of my nurse’s training, and that one week of non-stop, often life and death emergencies, almost did me in!
As I read your vivid, beautifully written description of what you endured last July, I could SEE it in my mind. In the eyes of the nurses, you were not a suffering human being with worth and dignity and rights no less important than their own, you were merely an unwelcome interruption, a problem to be dealt with, quickly and firmly and with a minimum of fuss and paperwork. This was not YOUR fault, it was the fault of the system, for want of a better word.
But knowing how HARD nursing is, does not in any way excuse the harsh, hateful, disrespectful attitude you were shown.. yet it does, in my mind at least, explain it. I have seen and experienced it myself, from BOTH sides of the medical charts, this harsh, disdainful attitude.
I have witnessed this, both as a nurse-in-training, and as a patient. When you’ve been called from the bedside of a child whose body was crushed less than an hour ago in an automobile accident, and his mother is dead, his father is hanging by a thread, and if the child survives, he will most likely never walk again… and here is a patient who has nothing visible wrong with her, only she is “inexplicably” freaking out – the disdainful, put-upon attitude from the medical personnel who simply do not “get” the first thing about the very real horror of psychological distress, is very real. It’s not your imagination, and it’s not your fault, either. It’s just that they don’t get it, and they are overworked and exhausted and stressed and overwhelmed with the horrors of life in the trenches.
I hope you know what I am trying to say here? To you, in your time of extreme duress and suffering, the snappy bitchiness and cold-heartedness of the medical personnel, coupled with the terrifying physical roughness of the guard, must have felt so very personal. But YOU were not the real target, in my opinion. The nurse was probably (inexcusably!) bitchy because she was already behind in her duties when you were brought in with your immediate pressing needs, and the guard was probably an overgrown boy playing macho-cop-wannabe, who finally got to see some adrenalin-pumping ACTION.
Someday, if they live long enough, that guard, and the nurses, will become old and infirm, and they will most likely experience, in some fashion, what it is like to be the one who is disempowered, hurting, fearful, and in need of compassionate help, while being treated like they are nothing more than an unwelcome interruption, a pain in the ass, an unimportant, non-person. Someday, I believe, it all comes back around. At least, that’s my hope!
Rachel
Finally, the following comment concerns my post “Open Letter to Dr Deborah Weidner (Sept. 9, 2012)”
The memories this post brings back…. I was shaking inside as I read it. It was hard enough going through this kind of mistreatment as a powerless teenage girl in a state mental institution, I can’t imagine going through this now, at the age of almost-60. I’m so sorry you were put through this. Until I read this just now, I thought your emergency room mistreatment of last July was the worst you had gone through recently. But this…. I don’t know how you came through it. I think if this had been done to me, I would have permanently checked out of reality.
Your feistiness is what’s keeping you alive. The very thing in you that the “wardens” of the mentally ill want to drug and shame and torture out of you, that undying spirit of yours is why you are still here, still breathing, still functioning, and still able to coherently tell your story. You are amazing.
Rachel
Am I Crazy? Hallucinations, Delusions or Consensual Reality
What is real? Is anything true and factual? Or are we all just deluded and mad as hatters? This is a serious question.
What I recall and what was written down in my chart about a certain four days in July 2012 are so different it is difficult to figure out whether my experience was fact in any sense of the word or, as “they”claimed, simply paranoid and delusional. Of course there is some truth in paranoia and delusion, since even a paranoid’s beliefs are based in feelings that arise honestly and from a foundation, I firmly believe, in true things sensed but unacknowledged. Feelings always have their own veracity. But whatever the philosophers may say about the fiction of facts, still there is, there must be, something more to the consensual world of what happens than mere perception.
I mean, either that security guard in the Emergency Department last July deliberately attempted to strangle me, or he did not. Either it happened or in some fashion I imagined it. It is that simple, isn’t it? Yes or no, red or green, one or zero. Like a digital configuration, there’s nothing vague about it: either it happened or it didn’t.
There are records. I know what the ones they wrote say, as far as they go. But how to interpret them since so little was written down, and unless my memory is so completely at odds with reality as to have confabulated the entire episode – which by the way, is what they claimed all along – how to explain the discrepancies when so much is not even mentioned. That they whisked my gurney into a seclusion room and assaulted me en masse is my version. In theirs, the room change is noted only in passing, and of the IM medication all that is said is that it was given “NOW”. Nothing else of the incident I recorded in great detail in my journal some days later, and raged about from the first day I was admitted to the day I left. In fact, I’m still outraged, months later.
I wanted to go home, they wanted me to stay. That I was abjectly terrified of being kept there meant to them that I was “paranoid.” I claimed I had no problems and had never been diagnosed with a psychiatric disorder. That was a problem for they had more power than I did as well as my lengthy psychiatric history on their side to prove I must be crazy to make such a claim. Worse, I was loud, demanding, and in my increasing panic, getting angry. They saw my screaming as a threat. Even though I was blind to what was going on, any onlooker could have seen that I could not win and in the end of course I lost mightily.
But let me go back towards the beginning.
It didn’t help that I had arrived at the ED by ambulance and immediately refused to have my “vitals” taken, asserting that I was “fine!” I then accused the nurse of just wanting to get paid for taking them. In short order I was whisked to the so-called “purple pod” where the psych patients were buried for hours until the on-call psychiatrist deigned to come down to see them.
“Here,” someone said, thrusting a hospital johnnie and a pair of pajama pants at me. “Undress and put these on.”
I looked down and saw that I was already wearing pj pants from another hospital. No one ever knew the real nature of what I wore — they simply passed for scrubs — and they were so comfortable that I kept them on day and night. “I’m already wearing pajama pants. I only need to change my shirt,” I said.
“No, you are wearing very nice blue slacks. Now, put on the pajamas, or do you want a couple of strong men to put them on for you?”
“Actually,” I sniped, “they are hospital pajama pants. I pilfered them from –“ and I named the hospital. But I made a show of undoing the snaps so they would see that I was going to comply. The last thing I wanted was anyone touching me or “helping” me undress.
Soon an APRN, came by and I thought, Wow, they are quick here, maybe it isn’t so bad being taken to a big hospital. Maybe I can get discharged from here in no time. Unfortunately, she was there only to do a 15 second “physical exam” that consisted of looking in my mouth and listening to my back with her stethoscope. Period. Pronouncing me cleared for a psychiatric interview, she rushed off to clear someone else. Then I sat on the gurney in my cubicle and waited. And waited.
I remember being cooperative for what felt like a long time. I tried to sleep, and I listened patiently to what was going on around me. I swore that I would simply hold my breath and bide my time until someone saw me, so that, calm, I could present my case and they would see I was safe and sane enough to be sent back home, not admitted or sent to some hospital against my will. But it was taking so long, it was taking hours for someone to see me, and I knew they were doing it to me on purpose. Did they think I, too, was drunk or on drugs just like the others here? I started to complain that I had waited long enough and needed to see someone. I was NOT drunk, did not need to dry out. Where was the doctor? There was nothing wrong with me, I did not need to be here. I wanted to go home!
Things started happening then. Memory fails me however and even the chart, which I just obtained a couple of days ago leaves out way too much. All it says is that I was uncooperative, then irritable, screaming and combative. Meds were “offered”.
I remember this: When I refused to take soul-deadening Haldol by mouth, they descended on me, wheeled my gurney into a solitary room and jumped on me, intending to inject me by brute force. In the struggle, a guard gripped my neck and compressed the arteries, strangling me. I tried to get the nurse’s attention, burbling through forcibly compressed lips that I could not breathe. But her response, attending only to her needles and not even looking at me, was an impatient, “You’re all right!” In a pulse of panic, I jerked away as she started to shove the first needle into my arm.
“Damn!” she cried as a rush of blood spattered us and the needle danced away from my skin. “Hold still!”
I’d hoped to get some respite from strangulation but instead of letting go of me, the guard reasserted his grip on my neck and pressed down harder. I felt the light go black as blood failed to reach my brain. Darkness descended. Sounds grew confused and dim. Suddenly I knew that I could die, that this was how patients had been “accidentally” killed during notorious restraint episodes in Connecticut. I did the only thing I could: I went limp, hoping the nurse would get the injections over with quickly and that the guard would not kill me before she was through.
One, two, and then, astonishingly a third needle punctured my arm. She wiped my deltoid muscle with an alcohol wipe then removed herself from the gurney. “All done,” she said, removing her gloves with a smack and she nodded, indicating the door.
With a cruel leisure, the guard let go of my neck, but he leaned down as he did so and muttered in my right ear: “That’ll teach you a lesson about bringing a JCAHO case against M— Hospital…” Then he and all the others strode out of the room, leaving me alone in what I had already been warned was a soundproof room where you can “scream all you want, but no one will hear you.”
In other circumstances, I would have screamed, soundproof or not, as the door was left open. But nothing was ordinary anymore. A guard – thuggish bully, no doubt a reject from the police academy — paid to protect people, had just partially strangled me in revenge for – what? What had I done to him? My case against that other hospital should have meant nothing to him. But what was clear to me, trying to get a breath and calm myself, was that I was not only not protected in the this ED, I was in mortal danger. I could not scream or rage in outrage, I could not even complain or demand to see a patient advocate. My life was imperiled. Still panting, trembling, in shock, I lay in the semi-dark of that single room and prayed — not to any god, mind you, but simply for my life, prayed to get out of that ED alive. I promised myself that I would not say or do anything “wrong,” would comply with everything they asked from then on in order to survive the night. But it was a long night ahead of me and I had no idea whether or not the guard would come back and finish the job. I was so terrified my teeth chattered. I felt a hollow coldness inside me of unutterable fear. And there was nothing I could do but lie there and hope he did not return.
__________________________________
I did not name the hospitals in the piece above, though I usually do, and I refrained from doing so because I do not know whether what I am going to write now is indeed true or not. But if it is not, then I do not want certain people being alerted to this blog post and reading it and taunting me with “Yehaw, we got away with it!” Read on, and you will see what I am talking about further on.
So as I said, I am in possession of my chart, the entire thing, 60 pp for a mere four day stay in the hospital about which I speak, including an approximately 10 hour stay in the ED. In it, there is absolutely no evidence that anyone ever took me or what I had to say seriously at any time. Everything I said was dismissed as paranoid and delusional, grandiose, disorganized or confabulating. (BTW Confabulate does not mean lying, it means to unintentionally “fabricate imaginary experiences as compensation for loss of memory.” But whatever they thought I was confabulating I have not the faintest idea. Or memory. Alas, the chart says nothing of what I spoke about.)
What has completely upset the applecart is my own statement, written in my journal and elsewhere: “Why on earth would that guard care whether or not JCAHO was involved in that other hospital?” On that thought rests everything, because of course, he had to have cared mightily to have wanted to strangle me for it. Or did he? Did he care, and in fact did he try to strangle me, and did he even say those words in my ear? I am serious.
You have to understand something: Once, years ago, I heard, or hallucinated, hospital nurses announce over the public address system in nearly the same words how they were going to “teach me a lesson” about — whatever it was I had done…and I knew I had heard it, knew I was hearing it at the time, except for the fact that I was on the phone with my sister at that time. I held out the phone in the air so she could hear it too, but she told me she heard nothing, assured me that I was hallucinating. What I described was not only unlikely but so beyond the realm of the likely that she was certain it could never have happened. “Its just your voices, Pammy,” she said, “you have to trust me, you are hallucinating.”
So remembering this, it gives me pause. For why would that guard care about JCAHO and that other hospital in the first or even the last place? What could it possibly mean to him? Security guards are usually hired from outside agencies so his over-involved concern with another hospital’s accreditation suddenly seems to me absurd. And if he did not care, why would he have tried to strangle me? Oh, maybe he did hold me down too hard, and I felt that, yes. But if I could speak, then I know I could breathe, so I was not actually being strangled either.
Perhaps I was simply frightened? And could it be that in fact he never said anything at all? That I “imagined” those words, hallucinated them, and then continued to believe that I heard him say them and that he wanted to kill me, all the time since then? Could it possibly be that some of what the hospital personnel said was true — NOT all of it, but some part of it. That I was in fact hallucinating and delusional? It doesn’t make their behavior right. It doesn’t justify throwing me into seclusion and injecting me with IM meds when I was not a danger to myself or others. It doesn’t even make admitting me to the hospital the proper thing to do in the first place. But, but, but…if I have heard people say things, visible people say things that they simply have not said, when they have not said anything at all, and I know this has been the case, then it is, I admit, just possible that what happened at the ED this summer might be another instance of the same…It pains me to think this. It frightens me to think that I could have been so mistaken for so long.
But what’s more, I worry that I am wrong to believe I might be wrong! That the guard DID say what I think he said, did intend to strangle me, and that I am giving him what he wanted: I am letting him drive me into believing I was/am crazy!
I do not know what to think. And I may never know for certain what happened. Not about this. However, one fact that I can corroborate in the record I am painfully aware I “knew” for months: I was given 3 IM drugs during that episode. Yet you only have to read my chart to see that I was given only 2: Geodon and Ativan. The third drug, Haldol, was canceled immediately after it was ordered. The records clearly state that only the Geodon and Ativan were ever administered. This is so striking an error of memory that it too makes me think again about trusting what I was certain I heard in that terrifying room where they held me down and injected me.
I don’t know what to do with this…I don’t know how to handle it or deal with it. It doesn’t feel good, or give me any sense of relief. I dunno how I feel. Just shocked, I guess. And perturbed, because I don’t know what else I have experienced that never “really” happened.
Natchaug Hospital and Trauma-related artwork (plus…)