Tag Archives: memoir
See my art at Jim Gottstein’s psychrights Everyday Horrors site
Award-Winning Short Story — 1 page — and art
THE DRESS
by Phoebe Sparrow Wagner (formerly Pamela Spiro Wagner)
I will never forget The Dress. Worn only once, with three quarter-length sleeves cuffed in white, and a demure white collar, it had two layers of navy blue crepe skirting, with a dropped waist and a sash. This was the first “dressy” dress I ever picked out all on my own.
The first thing about The Dress was that it was not the pale pink tent that I had worn to my first mixer with Sheffield Academy, which I was convinced scared away my freckled red-haired date, not that I minded much, once I saw him dance. The second thing about The Dress was the look in the eyes of the boy at the Gunnery, where my second mixer was held. This boy was matched with me strictly by height. I don’t know why, but something clicked with us, and the first thing he said to me, to my huge relief, was, “I hate dancing, don’t you? Let’s take a walk.” With that, we linked arms and spent the evening strolling arm in arm around his campus.
To say that nothing happened would seem almost hilarious these days, except that nothing did, besides our shared and passionate discussion of Plato and the books we’d read and other schoolish stuff. By the time the bells rang to call everyone back to the buses, I knew, because after all, I was a teenage girl who had read books, what might happen. I also knew, because I was an avid fan of the advice columnist Ann Landers, that no self-respecting young girl allowed a kiss on her first date. We had been walking arms around each other’s waist all evening; I liked him, it was equally clear that he liked me. It was inevitable what would happen next. But I was a good girl. What to do?
I tried to say good-bye, smiling sadly and keeping the distance that would protect me. My adoring young man nevertheless leaned in to kiss me. Turning my cheek, I rebuffed him. I did not mean to hurt his feelings, but I knew that Ann Landers was watching me and would be happy my virginity was safe. As I climbed onto the bus with a heavy heart, I looked back and waved but my date was nowhere to be seen. I took my seat, feelings mixed about whether the rebuff had truly been a success.
Then someone behind me spoke. “Good for you, Pammy, not kissing the black boy!”
What? I looked at her. My classmate was smiling grimly. “You didn’t kiss that -–“ and she used the terrible word I had never heard anyone say to my face.
In that moment, I knew that if I could have, I would have raced off the bus and grabbed that young man and kissed him full on the lips, and to hell with Ann Landers and her crappy advice.
But it was too late to change anything. Too late to let him know why I had not kissed him, too late to kiss him in spite of my classmates and too late to spite Ann Landers and my proper upbringing. Too late, too late, too late. I never wore that dress again.
—————————-
This short account, all too true, won first place at Vermont’s Counterpoint’s annual writing contest in 2015. You can see it and the other first place winner at
Click to access Counterpoint_Summer_2015.pdf
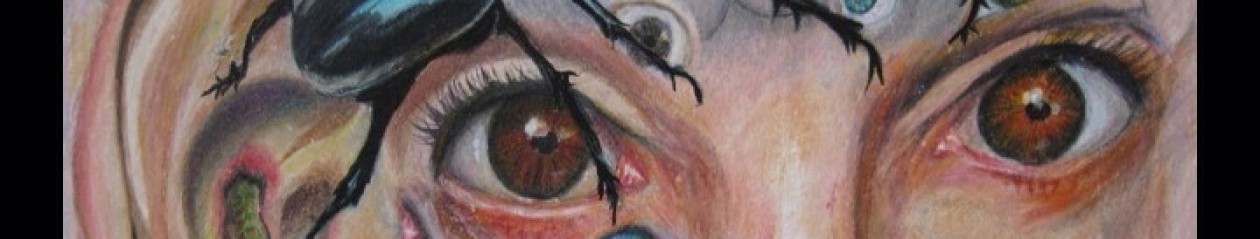
Below is my very first painting done in about 2009 or 2010 when I was first starting to do art. I called it First Love, and now you know why.

Important Video about Psychiatric Torture
“Divided Minds” now an audiobook!
What are/were the most significant barriers to your recovery from “mental illness”?
The biggest barrier to my recovery from what had always been diagnosed as schizophrenia or schizoaffective disorder was, I regret to say, the mental health system and psychiatry itself. Yes, for many decades I had been told I was ill and needed interventions like medications and the hospital for my “brittle psychosis”. I was told even that obvious brutalities, like 5-point restraints and seclusion in locked freezing cold cells, devoid of anything but a slab in the wall and a grate in the floor for drainage, were helpful treatments for my condition and not the torture and punishment that I felt them to be. No one or very few people treated me with kindness or any understanding or with the idea that there was hope for recovery, even though I had a genius level IQ and had shown some significant talents in many areas, and still did even when sick. They seemed bent on only one thing: coercion and control, and to prove that they were able to dominate me, and the other patients. If you dared to question their superiority or their information you would either be dismissed as delusional or worse, treated with more abuse.
Needless to say, I lived up to these expectations for many years, and i did not get better or even come near to recovering. In fact, before I took the drastic step of giving almost all I owned away and leaving my home, the state where I had lived for all my life and moving to another 100 miles away, by myself, knowing no one and nothing about it, I ended up again in the hospital and almost did not make it out. Not only did the guards there attempt to strangle me, but the doctor was convinced that I should be committed to the state’s one public facility that provided long term treatment…from which I might not leave for a long time.
Instead, I managed to play the game this sadistic doctor insisted on, and was finally discharged from a city hospital that had spent weeks doing nothing but torturing me, daily throwing me into their seclusion cell or shackling me in restraints …for no better reason than that I “disturbed the unit milieu”.
But discharged I was, with newly acquired PTSD from my treatment there, and within a week I was two states away, safe for the first time from these ministration that had inflicted on me nothing but damage.
It was here, in this northern state that I finally began to heal, with the help not of the mental health system but of a non-licensed therapist (she has a psychotherapist license from the UK) who taught me Marshall Rosenberg’s non-violent communication or NVC, and is the first person I felt sees me for who I really am, not “just another schizophrenic.” Even though I still take medications, I am slowly tapering off of them and doing well after decades on the massive doses I was told I absolutely could not survive without. Why? Because I’m proof of the fact that you can recover from life-long “mental illness” when given enough unconditional acceptance and understanding. When someone sees you and understands you and does not dismiss you, crazy as you might have been told you are, a lot of the craziness just falls away and you become another human being, no more and no less.
There is no normal, there is no abnormal. We are all just human beings trying to get along in society and often society is sicker than “we are” in its demands that we conform to some impossible standard. Maybe my experiences — hearing voices, thinking things that might be called delusions, etcetera — are not common but they are not outside the realm of human experience either. We should rejoice in our differences as in our similarities and look for common cause between us, not find reasons to fear what is Other in each other. Love really is what it’s all about. Maybe that sounds squishy and sentimental, but have you ever met someone diagnosed with schizophrenia who says they both love themselves and feel that they are adequately loved in the world by others?
Institute of Living, 2013, Torture and Illegal Confinement Part 2

Continued from previous post:
Here’s what SAMHSA the substance abuse and mental health services administration publication has to say on seclusion and trauma:
“Studies suggest that restraints and seclusion can be harmful and is often re-traumatizing for an individual who has suffered previous trauma…
“Further, there is a common misconception that seclusion and restraint are used only when absolutely necessary as crisis response techniques. In fact, seclusion and restraint are most commonly used to address loud, disruptive, noncompliant behavior and generally originate from a power struggle between consumer and staff. The decision to apply seclusion or restraint techniques is often arbitrary, idiosyncratic, and generally avoidable.
“Moreover, some studies indicate that seclusion and restraint use lead to an increase in the behaviors that staff members are attempting to control or eliminate.
I have been traumatized, and not just by hospitals. I was date-raped three times in my twenties and experienced traumatic domestic abuse. The cover sheet on the PAD made very clear that due to these trauma issues, I could not tolerate being secluded or restrained without severe consequences: regression and serious worsening of symptoms. Unfortunately, as soon as the staff saw fit to use physical methods of coercion and control on me, that is to say, punishment, from the first time a staff member grabbed me, all bets were off as to how I would behave. I certainly ceased improving, and my symptoms went downhill. Did they really think they were being kind and compassionate? Violence begets violence….
I tried to get help even when on the unit, at least I tried when I was free to make calls or leave my seclusion, err, forced-voluntary “time-out” two-week-long stay in the so-called side room” last winter. I do not know how many times I called the patient advocate office, but the sole time anyone made contact was when she came to hand me some paperwork – I believe I was actually in 4 point restraints at the time – some papers I could not read about a forced medication hearing they would be holding. I needed her advocacy, but she never responded to my panicked called. I wanted her help, but she never came by to ask me what I needed. She was less than useful, the fact that I had to go through her, and her refusal to respond contributed to my ongoing panic and desperate feelings of aloneness and depression. No wonder Dr. Banerjee tried to force me into ECT (about which my feelings of horror and revulsion were stated clearly in my PAD).
And where did the ECT discussion come from at all? My PAD states that I would refuse ECT under any and every circumstance. My brother would be my conservator if Banerjee had sought to go down that road, and he would never have made any decision to counter my wishes on that subject. If Banerjee really read my PAD, he would have known that. He told me that “Dr Mucha and I have made the decision to force you to have ECT.” I recorded the conversation in my journal immediately after it happened and Dr. Banerjee presented it as a two-man decision only, one that I had no choice in.
Regarding ECT and my so-called “depression,” Sanjay Banerjee MD had stopped my 75mg of the antidepressant Zoloft during the first or second week I was there. “Do you really need that?” he had asked, “You don’t seem depressed to me.” Obedient, and in any event glad to get off any medication at any time, I nodded my head, assenting to the change. At least, I thought, if things go haywire, it will not be due to self-fulfilling prophecy, a doctor looking for symptoms he expects to find and conveniently finding them. And at least he will know the reason.
A week later, instead of reinstating the Zoloft, Banerjee blamed my sudden “depression” on my refusal to take Lamictal, a drug I had not taken in 6-9 months. Now he was applying to force me to have ECT, something I was terrified of, convinced it caused deliberate brain damage.
It was this threat, and the brutality with which the decision was made, that started the downhill course of my IOL stay.
The very next day, all hell broke loose. When I entered the conference room, I pushed some important notes I needed Dr Banerjay and Laurie to read across the table in front of them. They refused, claiming that I threw the papers at them. Instead, Dr Banerjay proceeded to berate me, and told me how he had consulted with other hospitals and providers and had read my records against my instructions and Advance Directive, thus violating my HIPAA rights. Moreover, he threatened me with a behavioral treatment plan that would not permit me to do art or writing unless I “behaved.” I hit the roof, telling him I would sue the hospital and complain to JCAHO, then summarily left, slamming the door, an act that stemmed from feelings of utter impotence, because I couldn’t actually say in words anything more effective.
It could have ended there. I could have been left alone, to cool down and calm myself. But no, Dr. Banerjee had to write for stat meds again, and even though I was on the phone and trying to find someone to talk to, to calm myself, I had to be physically dragged off the chair I sat on, away from the phone and brought to the floor in a physical struggle (because they had attacked first, i.e. physically grabbed me, I defended myself, instinctually). They could have waited for me to finish the call. They could have waited to see if I calmed myself. I was not hurting anyone. I did not threaten anyone or myself with harm. ALL that I had done, in terms of physical threats was yell at the phone and refuse to take a pill. Furthermore, it was done and over with. I had left that area and gone to my room. I had then come back and now sat on the chair by the phone, speaking to my interlocutor on the other end. There was no need to pick a fight or encourage a struggle. A wait-and-see policy could have successfully guided things to a better resolution not only for the situation at hand but for my entire hospital stay. As a famous poem by Dylan Thomas ends: “After the first death, there is other.” Once the IOL staff decided to use restraints, there was no going back. The first time broke everything. So, they used them again, and again, and each time more freely and without justification but for convenience and punishment.
Some final points:
CMS regulations on use of Restraint and Seclusion
Restraint or seclusion may only be imposed to ensure the immediate physical safety of the patient, a staff member, or others and must be discontinued at the earliest possible time.
At no point in my stay was anyone ever in immediate physical danger except me, from the staff who were assaulting me…They may have claimed that I bit and fought and resisted, but this was always in response to their manhandling me first. Always. In fact, my medical records show they had restraints re-evaluated and approved while I was sleeping. They even discharged me from the hospital directly from restraints and seclusion, on a day when the usual attending physician happened to be out of town.
(ii) Seclusion is the involuntary confinement of a patient alone in a room or area from which the patient is physically prevented from leaving. Seclusion may only be used for the management of violent or self- destructive behavior.
This means that IOL’s definition of seclusion as being “kept alone in a room to which the door is locked” is wrong. I protested that I had been secluded all along, for a good two weeks before they instituted formal seclusion. I was not violent or self-destructive, and certainly not imminently dangerous to self or others…Never was anyone in immediate physical danger.) Yet the IOL allowed staff to abuse me and seclude me because I was loud and made people uncomfortable…I was surely not the first person to be so treated and brutalized. It remains traumatizing to this day, and I know it is still happening to patients at the IOL even now, because no one can stop them if they don’t know it is happening. Due to this sort of brutal treatment, my PTSD escalated. I think about what happened there and I can’t stop trembling. I have nightmares every night that literally keep me from sleeping.
“The highest price of all is the price paid by the people who are restrained: their recovery is stalled by a practice that can disempower them, break their spirit, and reignite a sense of helplessness and hopelessness…” from Recovery Innovations
Worst of all, using restraints doesn’t work to make either the patient calmer and safer or the unit a calmer safer environment to work in for staff. In truth, things only go from bad to worse once you restrain an unruly patient…Violence only begets more violence…Moreover, when I was another hospital, I was told by one of their mental health workers that she had wanted to experience the process of being four-pointed so she could identify with patients. She was told no, because as the aide informed me, hospital administrators feared it would be too traumatizing.
Restraints are traumatizing, let’s face it, in order to restrain me the manifold times I have been brutally restrained, putting up no resistance whatsoever, even the most jaded and brutal should have felt a twinge of conscience and questioned why he or she was doing. Unless they had become so inured to cruelty that they no longer considered it degrading and obscene to spread-eagle a naked woman, shackling her legs to the bed posts, so hardened to sadism that they did not consider tying her wrists to the underside of the bed as torture, only a mild form of discipline, meted out in order to teach her the lesson they had decided to teach her…
I hope you manage to read this letter and look at the supporting materials. You could learn a lot. You have more power than I do in this world, and could change things, if you know they are happening and are wrong. I beg you to think about what I have written to you. The IOL is not an isolated case. Brutality happens in nearly every psychiatric ward and hospital in Connecticut, and I believe this is the reason: As long as seclusion and restraints are permitted in any fashion, brutality and abuse will continue and at rates that are higher than where they are eschewed.
The problem is not that there may remain some exceptional cases who, it is claimed, will need to be restrained, but that someone somewhere will start finding such exceptions and boom, we’ll be right back where we started, with abuse and mistreatment of the most vulnerable. I believe the only way to stop the abuse of seclusion and restraints is to simply stop using them, period. Killing in self-defense is a good defense in law, and every decision to use restraints should be evaluated with similar strict thinking. Say No, we don’t go there, first, and then if done, know that it was a violation of the law and harmed the patient above all else, but under some conditions, this is the lesser evil compared to what might have eventuated without their use.
Now hospital workers are allowed to use restraints and seclusion as legitimate forms of “treatment. But when you permit staff to use violence against even one patient, it imbues their culture with an acceptance of violence as a treatment modality rather than something criminal. Restraints help no one. They are always retaliatory. Always discipline and punishment. Oh, in the short run the unit may seem quieter and easier to manage, but in the subsequent days, when the prisoner in restraints re-enters the community more chaos than ever may ensue.
Please help me. Do something about it today.
Institute of Living, Hartford CT, torture and illegal confinement in 2013
Part One

Let me introduce myself. My name is Pamela S. Wagner, and I was for most of my 65 years a resident of Connecticut. I have a long history diagnosed with serious mental illness and have been on disability for many years because of it. Five years ago, I was admitted to the Hartford Hospital’s Institute of Living on a 14-day PEC. I would like to tell you about some of the grotesque brutalities that transpired there and the egregious “treatment” that passes for care in that hospital.
Ever since I was discharged from the Institute of Living in February 2013, to which facility I had been committed as an involuntary patient under an order known as a Physicians Emergency Certificate. I have felt too terrified even to read the partial chart which the Connecticut Office of Protection and Advocacy obtained for me. Indeed, every time I recall what I am able to, or reread the brief nursing notes about what was done to me that winter at the IOL, my heart races unbearably, my body sweats and shakes and I start crying. Even so, because of trauma-induced amnesia, I remember the month I spent there only vaguely and in “snapshot” or flashbulb-like moments” of clarity. It is only now that I have acquired these few records, and learned some of the details of what happened that I’m finally able to put some of the pieces together.
Before I say anything further, I want to say that I believe that I was grievously injured by the “treatment” I received on Donnelly 2 South, and that what the staff did to me was not only unethical and cruel but that it crossed the line into illegality more than once.
I was admitted to Donnelly 2 South, and right from the first I made it clear that I wanted to witness their searching my knapsack. I wanted to know what they confiscated from me. They assured me that, Yes, of course, that is our policy, Don’t worry, Pam, you will have ample opportunity to watch us search your bags… I calmed a bit and followed a nurse to a closed room to do an intake interview. When she released me to the Day Area, I was shown to my room, where I found on my bed, my already searched knapsack and bags. Needless to say, this upset me greatly and I made my feelings known, which did not endear me to anyone. I let the charge nurse know that I felt violated and that she had openly broken a promise and my rights, posted prominently on the hospital wall.
As the Donnelly 2 staff learned, I had arrived prepared with a detailed Psychiatric Advanced Directive and I made it very clear that my online electronic medical record was accessible from any computer. I made the Read-Only access code available to the doctor and nurses. That included documents such as my narcolepsy diagnostic consult and special documentation proving my need for a higher than usual dosage of Ritalin, written by my former sleep specialist (also my psychiatrist from 2000-2009.) Included as well was a letter she wrote to my present psychiatrist, Dr. C, explicitly stating her conviction that I do not, and never did have a personality disorder, borderline or otherwise, a conviction that Dr C also held.
According to Dr. Sanjay Banerjee, the doctor who first took over my care, he read every page of these and all the other documents that I brought with me. That is what he told me. Moreover, when he spoke with Dr. C, my outside psychiatrist, he brushed off my concerns about anyone misperceiving me as having a personality disorder. My brother, P, himself a psychiatrist, brought the same matter to the fore again when in discussion with Laurie Denenberg, LCSW. Again, her response was much the same: “Personality disorders are not a part of the picture here. We intend to honor her PAD. We are glad that she has had the foresight to prepare such a document.”
Nevertheless, Amy Taylor, MD, the doctor who took over my care after Jan 27th decided to summarize my psychiatric history from this stay in words such as these: “long psychiatric history of schizophrenia, paranoid type, PTSD, and personality disorder NOS with borderline traits.” I was treated for four weeks for an active psychotic disorder. No one could know – especially with the significant additional diagnosis of PTSD, whether or not I had any personality disorder, given the two Axis I diagnoses already present. I believe she decided to use this diagnosis as a way to “justify” the brutality that she had ordered to be used to punish me during the hospitalization I write about.
As I said, I was on the Donnelly 2 unit for almost a month. But I was admitted on January 10, 2013, right into to seclusion because of putative “blepharitis.” They called it “infection precautions” but never took a culture of my swollen eyelids to determine if there truly was any infection present. They simply said it had to be blepharitis – as if saying so meant that it was so (but the fact is that blepharitis generally speaking is a benign non-infectious condition, and one that doesn’t produce massive swelling in the entire facial region). There were other factors however that accounted for my swollen face: prime among them the self -inflicted second degree burn on my forehead the size of a half dollar. Knowing this, the fact that my face had swelled to 1½ its size should not have surprised anyone. Blepharitis? The doctor was looking for zebras instead of seeing the common nag right in front of her…
I know I was a difficult patient. I was loud and paranoid and hard for some staff to deal with. That is precisely why I wrote out my Psychiatric Advance Directive the way I did, with explicit and detailed instructions for how best to deal with me when I was upset… When ill, I am frightened, paranoid, and hostile, which makes me easily roused to irritability. I know this, from a distance as it were. But knowing this now does not mean I was in full control of my behavior at the time.
On Feb 5th, I was being held incommunicado in the so-called “side room”, which, when I called it seclusion, the staff insisted it was not so. That afternoon, I simply walked away from it. I had had enough of them saying it was not seclusion, then preventing me bodily from leaving it. So, when I could do so without someone actually wanting to fight me, I walked away.
I proceeded to enter the unit and walk down the hall to the end and looked out the window. I took a deep breath, heard staff behind me, and sauntered back to the proper end of the hall, the “lost end” where they kept anyone from seeing me or knowing what they were doing to me. Once I got there, they descended upon me, some staff I knew, but most I did not. I did not bother to look at who was doing what to me. I simply lay passively on the bed and put my arms where they could do what I knew they would do. Tightly, they shackled my wrists out past my hips so there was no play in the restraints and I could not turn on my side or do anything but lie stiffly on my back. At the same time, others jerked my feet apart and just as tightly shackled my ankles to the lower corners of bed. Then came the coup de grace. They twisted me over onto my side somehow, pulled down my pants, and injected me with three drugs: Haldol 5mg, Ativan 2mg, and Benadryl 50mg. Why, except as punishment I do not know. I had, just a half hour before, been doped up on involuntary Zyprexa 10mg. Then they walked out, leaving someone just outside the door for the usual monitor, and did not release me for 19 hours, despite the fact that I was sleeping much of that time.
Of course, this was punishment. The very fact that they told me it was “not punishment” only “what your behavior brings on every time, Pamela,” proves my point. At first and usually they only said, it was because I “didn’t follow directions” so if they were not punishing me, what were they doing? They most certainly were not following Centers for Medicare and Medicaid regulations for the use of Restraints and Seclusion only in cases where a person is in imminent danger of harming her self or others. Indeed, the best they could do, when I protested, passively, saying just those words, was to respond, “You are not safe” as if that proved somehow that I was in danger or posed any imminent threat to the safety of anyone.
They always restrained me in an X, spread-eagled so tightly I couldn’t move a muscle. They never permitted bathroom breaks or even let my hands free to eat, so several times I had to pee and even defecate in my clothing. I would fall asleep rapidly after those three injections–whether I was restrained while calm or not, it was routine: punishment needles in the buttocks of Haldol 10mg, Ativan (up to 5mg at one time) and Benadryl 50mg—and then they would invent reasons to maintain me in restraints even after I was asleep for hours. When I woke, hardly dangerous to anyone, they would grill me with questions that I was too groggy to answer, and they would use my inability to respond as reason not to release me.
Later in the evening on Jan 5 or 6thth, for the second time that day, they restrained me, this time for throwing half a graham cracker at the wall. Then they left me like that for hours, even after I fell asleep. In point of fact, I could never earn my way to release from restraints by good behavior or quietly, calmly asking for release. Of course not, because I hadn’t done anything to “deserve” them in the first place. They always refused to release me, always, until I cried, “Uncle” when they told me to.
As to those vaunted “shows of force” what does anyone expect? Presented with a cohort of threatening staff personnel I saw only one thing: an impending assault. I know they anticipated my panic; it said as much in my chart. Isn’t that the point of a planned “show of force” – to induce fear and panic? (which when you think about it is grotesque…What sort of person wants to induce fear and more panic in someone who is by definition already terrified?) But why else do it? So why should it be any surprise, when I defended myself as they grabbed me? When they stuffed me into a body bag and were trying to tighten the straps, surely you can understand why anyone would bite the hand of an attacker whose digits came near. It was a matter of life and survival instinct…
But none of it should have happened. My PAD explained in exquisite detail exactly what to do and what I respond to better than fear tactics and force. In fact, it is beyond comprehension, knowing that one of the admission diagnoses I came in with was PTSD, how the director of patient care at the time pre-approved on paper the emergency abrogation of my PAD and a “just in case they are needed” use of restraints and seclusion. Why didn’t he counsel the person asking for this advance “right to restrain” to do instead all in his power not to restrain me and to work with the PAD instead?
TO BE CONTINUED… SEE NEXT ENTRY.
What Really Happened On W-1 in New Britain Hospital’s Psychiatric Unit in 2014…
I remember names…some of them. For instance, the short, chubby, blond nurse, who was worried about her weight and who was so instrumental in torturing me? Her name was Debra. And the head nurse who seemed so oblivious to the fact that her policies were indeed torture, even though she admitted that she expected the guards to inflict pain on patients when “escorting” them to seclusion in order to “subdue them faster” as she put it to me, openly. Her name was Barbara, and even though I was horrified by things she told me, I believe that she was innocently deluded and believed in her job, did not mean to be mean, not the way Debra seemed to, and honestly wanted the best for her patients. But let me start at some beginning which is to say, anywhere at all, and give you an idea of what I am talking about.

I have written in multiple places and on many occasions about what happened to me at New Britain Hospital (aka Hospital of Central Connecticut on Grand Street in New Britain) and I do not want to go into the whole thing here. All you need to do is search on the subject of Michael E Balkunas at this blog and you will get most of the gory details. That said, much that happened has never been told not even here. For instance, that Debra was the nurse who in a sadistic impulse and in an apparent fit of frustration, decided to have the security guards strip me naked when she was secluding me for some unknown (and always unnecessary) reason yet again…as they did nearly daily at W-1 in New Britain Hospital in May 2014….that it was Debra who was directly responsible for this I have never stated. But I remember her name clearly, and her face….And the fact that after she did this the second or third time she went on leave for several days, and when she came back told me she had almost quit her job.
I was momentarily cheered because I thought perhaps she had had some serious regrets about what she’d done to me. I asked her, Was it because of me? I thought she would tell me yes. She looked at me, and nodded, then said, “Because you are such a challenging patient.” Huh? I looked at her, and saw no remorse, no regrets only residual anger and scorn…and a certain unrepentant rancor that I had “made her do what she did.” Clearly she felt that I was to blame for her behavior, that I was to blame in general and that it was all justified.

But to get back to what happened. After she had me stripped naked by four male guards, after I loudly and vociferously protested being left alone in that freezing seclusion cell for I never knew how long, I began mildly hitting my head on the wall in protest. They threatened to four-point me and then they came barreling back in and threw me onto a restraint bed. The thing is, I knew, completely naked, I could not take the cold in that seclusion cell. But if they restrained me they would HAVE to cover me with something, and at the very least I would not freeze to death in that frigid cell for an indefinite number of hours…But when they came for me, they grabbed me and angrily threw me onto a gurney, even though I put up no resistance, spread-eagled my legs, deliberately exposing my private parts, and shackled them to the corners of the gurney with my arms pinioned above my head until I shrieked in pain even as they laughed. Then they held me down, gratuitously I might add, since I was already restrained, compressing my neck and chest, in order to give me the usual three-injection cocktail of punishment drugs — Haldol, Ativan and Benadryl — forcibly slammed into my buttocks. All of this done to me while I was naked and immobilized in four point restraints. Then fearing that they would leave me alone there, freezing cold, I screamed for them to cover me. With a look of disgust, someone threw a draw sheet over me, but no more.
The charge nurse came in for my “face to face” interview to see that all was “proper” and she visibly and audibly shivered, but refused me a warm blanket, or any at all, due to “safety concerns.” Then she left with the rest of them and turned off the intercom, so “we won’t have to listen to her scream.” They closed the door behind them, leaving me all alone behind a metal cell door that did not even have an observation window in it.
I screamed from the base of my lungs as deeply and as loudly as I could for as long as I could last. No one took mercy on me or brought me water or a blanket or spoke to me the entire time. Only when, exhausted, I finally lapsed did they relent and ask, from outside the door, “can we turn the intercom back on? She is quiet now…” And apparently got assent for that… Because eventually I heard someone flip a switch but nothing more.
After I was released, the next day, I told the unit director, Dr Michael E Balkunas what they had done to me, and he must have recognized the egregious nature of it because his response is telling. Instead of dismissing it as not so terrible, he said: “They would NEVER do such a thing as that in my hospital. You are a liar!” So he saw how awful it had been, what they had done to me, he just refused to acknowledge it had happened, and that he did not in fact what his staff were up to. But I was never in fact the liar he believed me to be. His stock answer to everything he did not want to see or believe was routinely that I was lying, but this was not true, and he was so sickeningly dismissive of the truth that I did not wait to listen to more this time. I was so wiped off the map by his response that I got up and walked out of the interview room and did not bother with him from then on…I KNEW I was never a liar, and that in actuality it was the STAFF who lied all the time, but telling Balkunas that would have done no good. He wanted to believe what he wanted to believe and nothing i said got through to him from day one…So I thought, so why bother ? WHY BOTHER. Balkunas wanted to murder my body and my spirit, and I could not let him succeed. He could imprison my body in his hospital, but i was damned if i would let him get my spirit. FUCK HIM!
But Dr Balkunas, Michael, you did not in point of fact know what went on at W-1 ever, nor at the ER, when you were there. Abuse was rampant because you encouraged it to be…and you never cared much what they did to achieve “order” so long as it was “quiet” when you were around. So you gave tacit assent to the tortures that they inflicted, and you likewise tacitly approved the very behaviors that you told me would “never happen on your watch”…Yeah? Well, I feel certain that if they behaved as they did towards me, they had done it before me, and did so to others after I left as well…and they continue to inflict these things on patients to this day.
I will leave it there. Your unit staff and you too, Balkie, are Out of control, and deserve, as my Obama post notes, to be CLOSED down for good.
The other day I made this little polymer clay figure to illustrate what Debra did to me.

It blew me away and I could not sleep all night the night I made her….Until Wendy and I decided to heal her, and perhaps heal me, from the experience, First, talking to the figure in the little bed calmly and with compassion, we covered her with a thick cotton blanket. That brought me some relief as I no longer felt chilled. Then we took off the restraints, which despite being made of polymer clay actually slipped right off, and we brought her arms down to her sides so she could sleep in comfort. By the time we were through I felt immensely better.
Neither of us could even imagine treating another human being as Balkunas had had me treated on numerous occasions by routine.
Do You Work in In-Patient Psychiatry? This is For YOU…
All art copyright of Pamela Spiro Wagner
Short Story with “Structural Tension” and more!
Dear Readers, here I am again, some scant four months after getting out of the Vermont state hospital unit in Rutland, Vermont, after two years of nearly nonstop institutionalizations, and i am dedicated to the proposition that i will never again see the inside of another mental health facility in this state, or any other state for that matter. Nor will i allow myself to be lied to again by a practitioner of mental health care, a subject i consider almost completely bogus, both the diagnosis of so-called mental disorders and their almost universally dangerous “treatments.”
In this spirit of rejecting the mental health system, rejecting even the non-system, except insofar as I need assistance in getting out of it, and rejecting *any* and all mental illness diagnosis, i decided to take a course in creativity for five days in Newfane, Vermont, just to try my hand at something outside the usual realm of “recovery-” and or madness-oriented activities.
While this ended up being, frankly, a bust — for reasons i will explain, i can report that i really liked the people i met there, some of whom came from as far away as the UK. As for the course itself, I feel that a requirement of valor means that i leave this at “the less said, the better.” I admit, however, that the teacher, a certain Robert Fritz of self-proclaimed international renown, seems to have been taking out his private pique on me ever since the course ended, for leaving the class early, on a few days, and for not praising him lavishly, or even, god knows, “enough.”
So be it, so be it. If he is so small as to exact such petty revenges, i myself need not stoop to his level.
Alas, the course ended up depleting me deeply and the sole worthwhile lesson it left me with concerned “structural tension.” This, Fritz repeated literally ad infinitum, or at least ad nauseam, all day long for five days, 8 hours a day. Sadly, the one time we did worthwhile hands-on practice, when he *first* outlined this notion and gave us a narrative structure — take point A and reverse it to point B (with a character, crisis and certain developing plot points) around which to easily design a monologue — Fritz then gave us an hour to write a piece in the voice of a single person, and was rewarded when every single person in the class wrote what i thought was a professionally competent piece, this was never to be repeated.
How much more he could have taught us and built on that, had he used the example of what we had learned and done and our confidence to “grow on and go on…” but instead he opted only for more of the same old same old, which was just going over the same ground again and again, with analyzing music video after music video but doing it FOR us, not even having us participate in any meaningful way. Readers, it truly appeared that class participation in any real sense was simply too threatening for this teacher, who was not one of those who felt he could learn anything from his students, no matter their age and life experiences…
No more recriminations on my part. I could not have known this would happen, especially since we were provided no clues, no syllabus, no handout that gave any hint as to Robert’s plans…I went in every day, every single day, and to every session with (dimming but) renewed hope that things would change, right to the last session of the last day…To my dismay and disappointment and growing exhaustion, it never did.
At least i enjoyed the monologue- writing exercise. The following was mine, which is fiction, though it was based on someone i know pretty well (and he knows who he is! )
_____________________________________
I, Winton Wooster the third, had sex for 30 years with one man and one man only, Arturo, whom I’d met in Culinary Arts school and absolutely despised. It took me another three years and five other men, one woman, and an Electrolux, before I came to realize that it was Arturo to whom I was attracted and loved with all my heart and soul and body. “Over The Rainbow” sung by Izzy Kamakawiwo’ole was our song.
Some people think gay men can’t be monogamous. That is so not true, so not true. I might have been promiscuous before Arturo, but A.A, that is After Arturo, I never looked away, that is until…well, how do I explain this?
It all started with cars. And collections. Collections of cars. And collections of everything else under the sun. I had the car collection, and I had the other collections. I had Kewpie dolls and Christ statuettes and I had spoons and books of spoonerisms, and I had jackknives and jack-in-the-boxes, I had bowls and bowling ball collections. If there was something to be collected, I collected it and more. I collected art and books, and books of art and china and vintage Chinese clothing and if you think there was no space left in my three-story house, that is saying nothing. I rented space in several other houses, my clients’ houses, which I cleaned each week, and those were soon filled with my collections as well. As for the cars? I had seventeen cars and that was only after culling them down from a high of thirty-seven.
As for Arturo? He had one. One car, and no collections. Only an affection for zinnias, which he called the gay flower and he grew tons of them, for me. His car was named Ada, and she was a 1987 Toyota Tercel. I always said I didn’t think they still made the Tercel that year, but he showed me the papers and proved that they had. Ada was pale yellow, a custom color, and still had the original fabric on her seats and the same original everything, just a tad creaky and fading. I joked with Arturo that we too were creaky and fading. Now, to tell a gay man of 55 that he is beginning to fade and creak is dicey at best, but we were not just old lovers, we were practically brothers, so the degree of his taking offense surprised me. But then he retorted that I shouldn’t talk, since I needed Viagra more often than not and that was only when I managed to get interested enough to take it.
Oooh, that got me where it hurt. But he wasn’t wrong. The thing is, I had once had enormous sex drive along with everything else but along the way, things seem to have just dissipated. I don’t know why exactly. But it was that remark that crystallized an amorphous dissatisfaction into the huge lump of cruel coal it was: Arturo was the source of my problems and my discontent. If I hadn’t been supporting him, if he didn’t live in my house, I would have more space for my things, and furthermore I would find someone I could, frankly, feel something for and well, get it up for. Period.
The end of our partnership came one night during a quarrel about my car collection, which was occupying several other garages as well as parking spaces in town. Several times a year during snow storms we had to play a desperate game of move the cars – in order to stay ahead of the tow trucks and the tickets to get them out of wherever they might be impounded. Arturo was sick of this, and frankly so was I and I wanted, I proposed, and I had actually had the plans secretly approved by the town zoning board, to build a giant garage in the back yard, a “garage-mahal” that would house my entire car collection on site. The problem was that in order to finance it, I wanted Arturo to pay rent, to help out, that is, with my second mortgage.
Arturo was hurt and he said so in no uncertain terms. He had lived with me and paid me in so many other ways, he told me, how could I do this to him? He cooked, he cleaned and he shopped and he did everything in the house to have made it a home for us and now I expected him to pay rent like a mere tenant? Firmly and obdurately I stood my ground and said, yes.
With tears in his eyes, for which I admit I felt a small pang, but not as big a pang as I ought to have, he turned around, climbed the stairs to our bedroom and packed a suitcase. Then I heard him tread the stairs downward, open the front door, and close it with a thud.
I was such a cad I did not even ask him where he was going or see him off. I felt a relief just to be rid of him. I can’t even say why. It was only the next morning that I discovered, in the small car shed I was planning within the week to tear down and replace with my garage-mahal, Arturo’s pale yellow Toyota Tercel, which he had left behind, for reasons I did not know and could not divine. After he didn’t pick it up for a month, I decided that he likely could not afford the payments or the gas, now that I was not paying for everything. Nevertheless, I could not bring myself to get rid of it, so I paid the insurance and made sure the registration was up to date and kept it on the first floor of the new enormous garage that was soon built on the back of my property.
I did not hear from Arturo at all after that. I learned from friends that he was renting a small first floor apartment on the outskirts of town, in exchange for taking care of the owners’ property. He was rumored to have neither phone nor email. I did not try to contact him but got absorbed instead in my own busy-ness.
In the garage-mahal there was room for all of my vehicles, all the ones in driving condition, including the Bentley for which I had paid only $22,000.00 but kept in mint condition. I had some cars on lifts and others were withdrawn down into specially constructed rooms underground. Only my special fire engine red Mustang and Arturo’s Tercel were in the front bay, readily available for driving.
I spent many of my leisure hours polishing and cleaning the cars, as the house had gone to seed, ever since Arturo was not there to pick up after me or sort the collected items. Also, it was – to be honest — lonely. I was able to have sex after Viagra, yes, but then only to have the Electrolux as my partner — what was the point? I gave up sex altogether. But that made me feel even worse. I tried the gay dances and party scene, and once even an “orgy” that a friend urged me to go to. But all of that just made the loneliness worse.
One night in the summer, sitting in a deck chair, under the bright LED lighting in the garage-mahal, I thought I heard someone’s radio playing a yard away. I got up to listen and heard our favorite song, “Over the Rainbow” performed by Izzy. I stole down the street, and listened to the radio on a porch nearby, and found myself standing in a clump of tall bright-petalled flowers as if by coincidence. No coincidence, I thought, there are no coincidences. I am a total cad, but I can’t let this be. I have left the love of my life and I need him back.
I ran back to the garage-mahal and jumped into the red Mustang, but the starter just made a coughing sound, as if it had just then given up the ghost. “Damn!” I yelled, then I realized that Arturo’s Tercel was still insured and ought to be drivable. Ought to be. Hell, yes, why not?
It was. As if it knew just where it was going the Tercel seemed to drive me all by itself to a small pink stucco house on the edge of town, a house surrounded by trees and with planters filled to the brim with zinnias. To this day I don’t know how it was that Arturo happened to be there, or why he did not seem surprised or even taken aback that I’d come. But without questioning anything, he just smiled warmly, opened the door and opened his arms.
So You Thought Your Genes or Drugs Cause Drug Addiction? Read This and Think Again
FROM THE HUFFINGTON POST:
The Likely Cause of Addiction Has Been Discovered, and It Is Not What You Think
By Johann Hari
It is now one hundred years since drugs were first banned — and all through this long century of waging war on drugs, we have been told a story about addiction by our teachers and by our governments. This story is so deeply ingrained in our minds that we take it for granted. It seems obvious. It seems manifestly true. Until I set off three and a half years ago on a 30,000-mile journey for my new book, Chasing The Scream: The First And Last Days of the War on Drugs, to figure out what is really driving the drug war, I believed it too. But what I learned on the road is that almost everything we have been told about addiction is wrong — and there is a very different story waiting for us, if only we are ready to hear it.
If we truly absorb this new story, we will have to change a lot more than the drug war. We will have to change ourselves.
I learned it from an extraordinary mixture of people I met on my travels. From the surviving friends of Billie Holiday, who helped me to learn how the founder of the war on drugs stalked and helped to kill her. From a Jewish doctor who was smuggled out of the Budapest ghetto as a baby, only to unlock the secrets of addiction as a grown man. From a transsexual crack dealer in Brooklyn who was conceived when his mother, a crack-addict, was raped by his father, an NYPD officer. From a man who was kept at the bottom of a well for two years by a torturing dictatorship, only to emerge to be elected President of Uruguay and to begin the last days of the war on drugs.
I had a quite personal reason to set out for these answers. One of my earliest memories as a kid is trying to wake up one of my relatives, and not being able to. Ever since then, I have been turning over the essential mystery of addiction in my mind — what causes some people to become fixated on a drug or a behavior until they can’t stop? How do we help those people to come back to us? As I got older, another of my close relatives developed a cocaine addiction, and I fell into a relationship with a heroin addict. I guess addiction felt like home to me.
If you had asked me what causes drug addiction at the start, I would have looked at you as if you were an idiot, and said: “Drugs. Duh.” It’s not difficult to grasp. I thought I had seen it in my own life. We can all explain it. Imagine if you and I and the next twenty people to pass us on the street take a really potent drug for twenty days. There are strong chemical hooks in these drugs, so if we stopped on day twenty-one, our bodies would need the chemical. We would have a ferocious craving. We would be addicted. That’s what addiction means.
One of the ways this theory was first established is through rat experiments — ones that were injected into the American psyche in the 1980s, in a famous advert by the Partnership for a Drug-Free America. You may remember it. The experiment is simple. Put a rat in a cage, alone, with two water bottles. One is just water. The other is water laced with heroin or cocaine. Almost every time you run this experiment, the rat will become obsessed with the drugged water, and keep coming back for more and more, until it kills itself.
The advert explains: “Only one drug is so addictive, nine out of ten laboratory rats will use it. And use it. And use it. Until dead. It’s called cocaine. And it can do the same thing to you.”
But in the 1970s, a professor of Psychology in Vancouver called Bruce Alexandernoticed something odd about this experiment. The rat is put in the cage all alone. It has nothing to do but take the drugs. What would happen, he wondered, if we tried this differently? So Professor Alexander built Rat Park. It is a lush cage where the rats would have colored balls and the best rat-food and tunnels to scamper down and plenty of friends: everything a rat about town could want. What, Alexander wanted to know, will happen then?
In Rat Park, all the rats obviously tried both water bottles, because they didn’t know what was in them. But what happened next was startling.
The rats with good lives didn’t like the drugged water. They mostly shunned it, consuming less than a quarter of the drugs the isolated rats used. None of them died. While all the rats who were alone and unhappy became heavy users, none of the rats who had a happy environment did.
At first, I thought this was merely a quirk of rats, until I discovered that there was — at the same time as the Rat Park experiment — a helpful human equivalent taking place. It was called the Vietnam War. Time magazine reported using heroin was “as common as chewing gum” among U.S. soldiers, and there is solid evidence to back this up: some 20 percent of U.S. soldiers had become addicted to heroin there, according to a study published in the Archives of General Psychiatry. Many people were understandably terrified; they believed a huge number of addicts were about to head home when the war ended.
But in fact some 95 percent of the addicted soldiers — according to the same study — simply stopped. Very few had rehab. They shifted from a terrifying cage back to a pleasant one, so didn’t want the drug any more.
Professor Alexander argues this discovery is a profound challenge both to the right-wing view that addiction is a moral failing caused by too much hedonistic partying, and the liberal view that addiction is a disease taking place in a chemically hijacked brain. In fact, he argues, addiction is an adaptation. It’s not you. It’s your cage.
After the first phase of Rat Park, Professor Alexander then took this test further. He reran the early experiments, where the rats were left alone, and became compulsive users of the drug. He let them use for fifty-seven days — if anything can hook you, it’s that. Then he took them out of isolation, and placed them in Rat Park. He wanted to know, if you fall into that state of addiction, is your brain hijacked, so you can’t recover? Do the drugs take you over? What happened is — again — striking. The rats seemed to have a few twitches of withdrawal, but they soon stopped their heavy use, and went back to having a normal life. The good cage saved them. (The full references to all the studies I am discussing are in the book.)
When I first learned about this, I was puzzled. How can this be? This new theory is such a radical assault on what we have been told that it felt like it could not be true. But the more scientists I interviewed, and the more I looked at their studies, the more I discovered things that don’t seem to make sense — unless you take account of this new approach.
Here’s one example of an experiment that is happening all around you, and may well happen to you one day. If you get run over today and you break your hip, you will probably be given diamorphine, the medical name for heroin. In the hospital around you, there will be plenty of people also given heroin for long periods, for pain relief. The heroin you will get from the doctor will have a much higher purity and potency than the heroin being used by street-addicts, who have to buy from criminals who adulterate it. So if the old theory of addiction is right — it’s the drugs that cause it; they make your body need them — then it’s obvious what should happen. Loads of people should leave the hospital and try to score smack on the streets to meet their habit.
But here’s the strange thing: It virtually never happens. As the Canadian doctor Gabor Mate was the first to explain to me, medical users just stop, despite months of use. The same drug, used for the same length of time, turns street-users into desperate addicts and leaves medical patients unaffected.
If you still believe — as I used to — that addiction is caused by chemical hooks, this makes no sense. But if you believe Bruce Alexander’s theory, the picture falls into place. The street-addict is like the rats in the first cage, isolated, alone, with only one source of solace to turn to. The medical patient is like the rats in the second cage. She is going home to a life where she is surrounded by the people she loves. The drug is the same, but the environment is different.
This gives us an insight that goes much deeper than the need to understand addicts. Professor Peter Cohen argues that human beings have a deep need to bond and form connections. It’s how we get our satisfaction. If we can’t connect with each other, we will connect with anything we can find — the whirr of a roulette wheel or the prick of a syringe. He says we should stop talking about ‘addiction’ altogether, and instead call it ‘bonding.’ A heroin addict has bonded with heroin because she couldn’t bond as fully with anything else.
So the opposite of addiction is not sobriety. It is human connection.
When I learned all this, I found it slowly persuading me, but I still couldn’t shake off a nagging doubt. Are these scientists saying chemical hooks make no difference? It was explained to me — you can become addicted to gambling, and nobody thinks you inject a pack of cards into your veins. You can have all the addiction, and none of the chemical hooks. I went to a Gamblers’ Anonymous meeting in Las Vegas (with the permission of everyone present, who knew I was there to observe) and they were as plainly addicted as the cocaine and heroin addicts I have known in my life. Yet there are no chemical hooks on a craps table.
But still, surely, I asked, there is some role for the chemicals? It turns out there is an experiment which gives us the answer to this in quite precise terms, which I learned about in Richard DeGrandpre’s book The Cult of Pharmacology.
Everyone agrees cigarette smoking is one of the most addictive processes around. The chemical hooks in tobacco come from a drug inside it called nicotine. So when nicotine patches were developed in the early 1990s, there was a huge surge of optimism — cigarette smokers could get all of their chemical hooks, without the other filthy (and deadly) effects of cigarette smoking. They would be freed.
But the Office of the Surgeon General has found that just 17.7 percent of cigarette smokers are able to stop using nicotine patches. That’s not nothing. If the chemicals drive 17.7 percent of addiction, as this shows, that’s still millions of lives ruined globally. But what it reveals again is that the story we have been taught about The Cause of Addiction lying with chemical hooks is, in fact, real, but only a minor part of a much bigger picture.
This has huge implications for the one-hundred-year-old war on drugs. This massive war — which, as I saw, kills people from the malls of Mexico to the streets of Liverpool — is based on the claim that we need to physically eradicate a whole array of chemicals because they hijack people’s brains and cause addiction. But if drugs aren’t the driver of addiction — if, in fact, it is disconnection that drives addiction — then this makes no sense.
Ironically, the war on drugs actually increases all those larger drivers of addiction. For example, I went to a prison in Arizona — ‘Tent City’ — where inmates are detained in tiny stone isolation cages (‘The Hole’) for weeks and weeks on end to punish them for drug use. It is as close to a human recreation of the cages that guaranteed deadly addiction in rats as I can imagine. And when those prisoners get out, they will be unemployable because of their criminal record — guaranteeing they with be cut off even more. I watched this playing out in the human stories I met across the world.
There is an alternative. You can build a system that is designed to help drug addicts to reconnect with the world — and so leave behind their addictions.
This isn’t theoretical. It is happening. I have seen it. Nearly fifteen years ago, Portugal had one of the worst drug problems in Europe, with 1 percent of the population addicted to heroin. They had tried a drug war, and the problem just kept getting worse. So they decided to do something radically different. They resolved to decriminalize all drugs, and transfer all the money they used to spend on arresting and jailing drug addicts, and spend it instead on reconnecting them — to their own feelings, and to the wider society. The most crucial step is to get them secure housing, and subsidized jobs so they have a purpose in life, and something to get out of bed for. I watched as they are helped, in warm and welcoming clinics, to learn how to reconnect with their feelings, after years of trauma and stunning them into silence with drugs.
One example I learned about was a group of addicts who were given a loan to set up a removals firm. Suddenly, they were a group, all bonded to each other, and to the society, and responsible for each other’s care.
The results of all this are now in. An independent study by the British Journal of Criminology found that since total decriminalization, addiction has fallen, and injecting drug use is down by 50 percent. I’ll repeat that: injecting drug use is down by 50 percent. Decriminalization has been such a manifest success that very few people in Portugal want to go back to the old system. The main campaigner against the decriminalization back in 2000 was Joao Figueira, the country’s top drug cop. He offered all the dire warnings that we would expect from the Daily Mail or Fox News. But when we sat together in Lisbon, he told me that everything he predicted had not come to pass — and he now hopes the whole world will follow Portugal’s example.
This isn’t only relevant to the addicts I love. It is relevant to all of us, because it forces us to think differently about ourselves. Human beings are bonding animals. We need to connect and love. The wisest sentence of the twentieth century was E.M. Forster’s — “only connect.” But we have created an environment and a culture that cut us off from connection, or offer only the parody of it offered by the Internet. The rise of addiction is a symptom of a deeper sickness in the way we live — constantly directing our gaze towards the next shiny object we should buy, rather than the human beings all around us.
The writer George Monbiot has called this “the age of loneliness.” We have created human societies where it is easier for people to become cut off from all human connections than ever before. Bruce Alexander — the creator of Rat Park — told me that for too long, we have talked exclusively about individual recovery from addiction. We need now to talk about social recovery — how we all recover, together, from the sickness of isolation that is sinking on us like a thick fog.
But this new evidence isn’t just a challenge to us politically. It doesn’t just force us to change our minds. It forces us to change our hearts.
Loving an addict is really hard. When I looked at the addicts I love, it was always tempting to follow the tough love advice doled out by reality shows like Intervention — tell the addict to shape up, or cut them off. Their message is that an addict who won’t stop should be shunned. It’s the logic of the drug war, imported into our private lives. But in fact, I learned, that will only deepen their addiction — and you may lose them altogether. I came home determined to tie the addicts in my life closer to me than ever — to let them know I love them unconditionally, whether they stop, or whether they can’t.
When I returned from my long journey, I looked at my ex-boyfriend, in withdrawal, trembling on my spare bed, and I thought about him differently. For a century now, we have been singing war songs about addicts. It occurred to me as I wiped his brow, we should have been singing love songs to them all along.
The full story of Johann Hari’s journey — told through the stories of the people he met — can be read in Chasing The Scream: The First and Last Days of the War on Drugs, published by Bloomsbury. The book has been praised by everyone from Elton John to Glenn Greenwald to Naomi Klein. You can buy it at all good bookstores and read more at www.chasingthescream.com.
Johann Hari will be talking about his book at 7pm at Politics and Prose in Washington DC on the 29th of January, at lunchtime at the 92nd Street Y in New York City on the 30th January, and in the evening at Red Emma’s in Baltimore on the 4th February.
The full references and sources for all the information cited in this article can be found in the book’s extensive end-notes.
If you would like more updates on the book and this issue, you can like the Facebook page: https://www.facebook.com/chasingthescream
Poem about Radical Forgiveness

TO FORGIVE IS…
To begin and there is so much to forgive
for one, your parents, one and two,
out of whose dim haphazard coupling
you sprang forth roaring, indignantly alive.
For this, whatever else followed,
innocent and guilty, forgive them.
If it is day, forgive the sun its white radiance
blinding the eye;
forgive also the moon for dragging the tides,
for her secrets, her half heart of darkness;
whatever the season, forgive it its various assaults
— floods, gales, storms of ice —
and forgive its changing; for its vanishing act,
stealing what you love and what you hate,
indifferent, forgive time;
and likewise forgive its fickle consort, memory
which fades the photographs of all you can’t remember;
forgive forgetting, which is chaste and kinder
than you know; forgive your age and the age you were when happiness was afire in your blood
and joy sang hymns in the trees;
forgive, too, those trees, which have died;
and forgive death for taking them, inexorable as God; then forgive God His terrible grandeur, His unspeakable Name
forgive, too, the poor devil for a celestial falll no worse than your own.
When you have forgiven whatever is of earth, of sky, of water, whatever is named, whatever remains nameless
forgive, finally, your own sorry self, clothed in temporary flesh,
the breath and blood of you already dying.
Dying, forgiven, now you begin.
by Pamela Spiro Wagner in “We Mad Climb Shaky Ladders” (Cavakerry Press 2009) also featured in “Divided Minds: twin sisters and their Journey through schizophrenia.”
YOU AND YOUR ANTIDEPRESSANT — From Anne C Woodlen’s Blog
I THOUGHT THIS WAS INCREDIBLY WELL WRITTEN AND IMPORTANT INFORMATION. SEE CREDITS AT THE BOTTOM. Posted on January 12, 2014 by annecwoodlen THINGS YOUR DOCTOR SHOULD TELL YOU ABOUT ANTIDEPRESSANTS September 12, 2012 By Paul W. Andrews, Lyndsey Gott & J. Anderson Thomson, Jr. Antidepressant medication is the most commonly prescribed treatment for people with depression. They are also commonly prescribed for other conditions, including bipolar depression, post-traumatic stress disorder, obsessive-compulsive disorder, chronic pain syndromes, substance abuse and anxiety and eating disorders. According to a 2011 report released by the US Centers for Disease Control and Prevention, about one out of every ten people (11%) over the age of 12 in the US is on antidepressant medications. Between 2005 and 2008, antidepressants were the third most common type of prescription drug taken by people of all ages, and they were the most frequently used medication by people between the ages of 18 and 44. In other words, millions of people are prescribed antidepressants and are affected by them each year. The conventional wisdom is that antidepressant medications are effective and safe. However, the scientific literature shows that the conventional wisdom is flawed. While all prescription medications have side effects, antidepressant medications appear to do more harm than good as treatments for depression. We reviewed this evidence in a recent article published in the journal Frontiers in Psychology (freely available here). The widespread use of antidepressants is a serious public health problem, and it raises a number of ethical and legal issues for prescribers (physicians, nurse practitioners). Here, we summarize some of the most important points that prescribers should ethically tell their patients before they prescribe antidepressant medications. We also discuss the ways that prescribers could be held legally liable for prescribing antidepressants. Finally, we implore practitioners to update the informed consent procedure for antidepressant medication to reflect current research and exercise greater caution in the prescription of antidepressants.
- How antidepressant medication works
Most antidepressants are designed to alter mechanisms regulating serotonin, an evolutionarily ancient biochemical found throughout the brain and the rest of the body. In the brain, serotonin acts as a neurotransmitter—a chemical that controls the firing of neurons (brain cells that regulate how we think, feel, and behave). However, serotonin evolved to regulate many other important processes, including neuronal growth and death, digestion, muscle movement, development, blood clotting, and reproductive function. Antidepressants are most commonly taken orally in pill form. After they enter the bloodstream, they travel throughout the body. Most antidepressants, such as the selective serotonin reuptake inhibitors (SSRIs), are intended to bind to a molecule in the brain called the serotonin transporter that regulates levels of serotonin. When they bind to the transporter, they prevent neurons from reabsorbing serotonin, which causes a buildup of serotonin outside of neurons. In other words, antidepressants alter the balance of serotonin in the brain, increasing the concentration outside of neurons. With long-term antidepressant use, the brain pushes back against these drugs and eventually restores the balance of serotonin outside of the neuron with a number of compensatory changes. It is important to realize that the serotonin transporter is not only found in the brain—it is also found at all the major sites in the body where serotonin is produced and transported, including the gut and blood cells called platelets. Since antidepressants travel throughout the body and bind to the serotonin transporter wherever it is found, they can interfere with the important, diverse processes regulated by serotonin throughout the body. While physicians and their patients are typically only interested in the effects of antidepressants on mood, the harmful effects on other processes in the body (digestion, sexual function, abnormal bleeding, etc.) are perfectly expectable when you consider how these drugs work.
- Antidepressants are only moderately effective during treatment and relapse is common Since the brain pushes back against the effects of antidepressants, the ability of these drugs to reduce depressive symptoms is limited (see our article for a review). While there is some debate over precisely how much antidepressants reduce depressive symptoms in the first six to eight weeks of treatment, the consistent finding is that the effect is quite modest.
Many people who have suffered from depression report a substantial symptom-reducing benefit while taking antidepressants. The problem is that symptoms are also substantially reduced when people are given a placebo—a sugar pill that lacks the chemical properties of antidepressant medications. In fact, most of the improvement that takes place during antidepressant treatment (approximately 80%) also takes place with a placebo. Of course, antidepressants are slightly more effective than placebo in reducing symptoms, but this difference is relatively small, which is what we mean when we say that antidepressants have a “modest” ability to reduce depressive symptoms. The pushback of the brain increases over months of antidepressant treatment, and depressive symptoms commonly return (frequently resulting in full blown relapse). Often this compels practitioners to increase the dose or switch the patient to a more powerful drug. Prescribers fail to appreciate that the return of symptoms often occurs because the brain is pushing back against the effect of antidepressants. 3. The risk of relapse is increased after antidepressant medication has been discontinued Another effect of the brain pushing back against antidepressants is that the pushback can cause a relapse when you stop taking the drug. This pushback effect is analogous to the action of a spring. Imagine a spring with one end attached to a wall. An antidepressant suppresses the symptoms of depression in a way that is similar to compressing the spring with your hand. When you stop taking the drug (like taking your hand off the spring from its compressed position), there is a surge in the symptoms of depression (like the overshoot of the spring before it returns to its resting position). The three month risk of relapse for people who took a placebo is about 21%. But the three month risk of relapse after you stop taking an SSRI is 43%—twice the risk. For stronger antidepressants, the three month risk is even higher.
- Antidepressants have been found to cause neuronal damage and death in rodents, and they can cause involuntary, repetitive movements in humans.
Antidepressants can kill neurons (see our article for a review). Many medical practitioners will be surprised by this fact because it is widely believed in the medical community that antidepressants promote the growth of new neurons. However, this belief is based on flawed evidence—a point that we address in detail in our article. One way antidepressants could kill neurons is by causing structural damage of the sort often found in Parkinson’s disease. This neurological damage might explain why some people taking antidepressant medication can develop Parkinsonian symptoms and tardive dyskinesia, which is characterized by involuntary and repetitive body movements. Many prescribers mistakenly think these syndromes only occur in patients taking antipsychotic medications.
- Antidepressants may increase the risks of breast cancer, but may protect against brain cancers .
Recent research indicates that antidepressants may increase the risk of cancer outside of the brain, such as breast cancer. However, the neuron-killing properties of antidepressants may make them potentially useful as treatments for brain cancers, and current research is testing this possibility.
- Antidepressants may cause cognitive decline.
Since neurons are required for proper brain functioning, the neuron-killing effects of antidepressants can be expected to have negative effects on cognition. In rodents, experiments have found that prolonged antidepressant use impairs the ability to learn a variety of tasks. Similar problems may exist in humans. Numerous studies have found that antidepressants impair driving performance, and they may increase the risk of car accidents. Recent research on older women also indicates that prolonged antidepressant use is associated with a 70% increase in the risk of mild cognitive impairment and an increase in the risk of probable dementia. 7.Antidepressants are associated with impaired gastrointestinal functioning The action of antidepressants results in elevated levels of serotonin in the intestinal lining, which is associated with irritable bowel syndrome. Indeed, antidepressants have been found to cause the same symptoms as irritable bowel syndrome—pain, diarrhea, constipation, indigestion, bloating and headache. In a recent study, 14-23% of people taking antidepressants suffered these side effects. 8. Antidepressants cause sexual dysfunction and have adverse effects on sperm quality. Depression commonly causes problems in sexual functioning. However, many antidepressants make the problem worse, impairing sexual desire, arousal, and orgasm. The most widely studied and commonly prescribed antidepressants—Celexa, Effexor, Paxil, Prozac, and Zoloft—have been found to increase the risk of sexual dysfunction by six times or more. Evidence from case studies suggests that antidepressants may also interfere with attachment and romantic love. Some antidepressants have been found to negatively impact sperm structure, volume, and mobility. 9. Antidepressant use is associated with developmental problems Antidepressant medication is frequently prescribed to pregnant and lactating mothers. Since SSRIs can pass through the placental barrier and maternal milk, they can affect fetal and neonatal development. Generally, if SSRIs are taken during pregnancy, there is an increased risk of preterm delivery and low birth weight. Exposure during the first trimester can increase the risk of congenital defects and developing an autism spectrum disorder, such as Asperger’s Syndrome. Third trimester SSRI exposure is associated with an increased risk of persistent pulmonary hypertension in the newborn (10% mortality rate) and medication withdrawal symptoms such as crying, irritability, and convulsions. Prenatal exposure to SSRIs is also associated with an increased risk of respiratory distress, which is the leading cause of death of premature infants. 11\\10. Antidepressant use is associated with an increased risk of abnormal bleeding and stroke Serotonin is crucial to platelet function and promotes blood clotting, which is important when one has a bleeding injury. Patients taking SSRIs and other antidepressants are more likely to have abnormal bleeding problems (for a review see our article). They are more likely to have a hemorrhagic stroke (caused by a ruptured blood vessel in the brain) and be hospitalized for an upper gastrointestinal bleed. The bleeding risks are likely to increase when SSRIs are taken with other medications that reduce clotting, such as aspirin, ibuprofen, or Coumadin . 11. Antidepressants are associated with an increased risk of death in older people. Depression itself is associated with an increased risk of death in older people—primarily due to cardiovascular problems. However, antidepressants make the problem worse. Five recent studies have shown that antidepressant use is associated with an increased risk of death in older people (50 years and older), over and above the risk associated with depression. Four of the studies were published in reputable medical journals—The British Journal of Psychiatry, Archives of Internal Medicine, Plos One, and the British Medical Journal—by different research groups. The fifth study was presented this year at the American Thoracic Society conference in San Francisco. In these studies, the estimated risk of death was substantial. For instance, in the Women’s Health Initiative study, antidepressant drugs were estimated to cause about five deaths out of a 1000 people over a year’s time. This is the same study that previously identified the dangers of hormonal replacement therapy for postmenopausal women. In the study published in the British Medical Journal, antidepressants were estimated to cause 10 to 44 deaths out of a 1000 people over a year, depending on the type of antidepressant. In comparison, the painkiller Vioxx was taken off the market in the face of evidence that it caused 7 cardiac events out of 1000 people over a year. Since cardiac events are not necessarily fatal, the number of deaths estimated to be caused by antidepressants is arguably of much greater concern. An important caveat is that these studies were not placebo-controlled experiments in which depressed participants were randomly assigned to placebo or antidepressant treatment. For this reason, one potential problem is that perhaps the people who were taking antidepressants were more likely to die because they had more severe depression. However, the paper published in the British Medical Journal was able to rule out that possibility because they controlled for the pre-medication level of depressive symptoms. In other words, even among people who had similar levels of depression without medication, the subsequent use of antidepressant medications was associated with a higher risk of death. These studies were limited to older men and women. But many people start taking antidepressants in adolescence or young adulthood. Moreover, since the risk of a relapse is often increased when one attempts to go off an antidepressant (see point 3 above), people may remain on medication for years or decades. Unfortunately, we have no idea how the cumulative impact of taking antidepressants for such a long time affects the expected lifespan. In principle, long-term antidepressant use could shave off years of life. It is commonly argued that antidepressants are needed to prevent depressed patients from committing suicide. Yet there is a well-known controversy over whether antidepressants promote suicidal behavior. Consequently, it is not possible to reach any firm conclusions about how antidepressants affect the risk of suicidal behavior. However, most deaths attributed to antidepressants are not suicides. In other words, antidepressants appear to increase the risk of death regardless of their effects on suicidal behavior. We suggest that antidepressants increase the risk of death by degrading the overall functioning of the body. This is suggested by the fact that antidepressants have adverse effects on every major process in the body regulated by serotonin. 12. Antidepressants have many negative effects on older people Most of the research on the adverse health effects of antidepressants has been conducted on older patients. Consequently, our conclusions are strongest for this age group. In addition to cognitive decline, stroke and death, antidepressant use in older people is associated with an increased risk of falling and bone fracture. Older people taking SSRIs are also at an increased risk of developing hyponatremia (low sodium in the blood plasma). This condition is characterized by nausea, headache, lethargy, muscle cramps and disorientation. In severe cases, hyponatremia can cause seizures, coma, respiratory arrest and death. The fact that most research has been conducted on older people does not mean that antidepressants do not have harmful effects on the young. As previously discussed, antidepressants can have harmful effects on development. Moreover, many people start taking these drugs when they are young and remain on them for years or decades. In principle, the negative effects of these drugs could be substantial over such long periods of time. Altogether, the evidence leads us to conclude that antidepressants generally do more harm than good as treatments for depression. On the benefit side, the drugs have a limited ability to reduce symptoms. On the cost side, there is a significant and unappreciated list of negative health effects because these drugs affect all the processes regulated by serotonin throughout the body. While the negative effects are unintended by the physician and the patient, they are perfectly expectable once you understand how these drugs work. Taken together, the evidence suggests that these drugs degrade the overall functioning of the body. It is difficult to argue that a drug that increases the risk of death is generally helping people. There may be conditions other than depression where antidepressants are generally beneficial (e.g., as treatments for brain tumors and facilitating recovery after a stroke), but further research in these areas is needed (see our article). Ethical and Legal Issues Physicians and other medical practitioners have an ethical obligation to avoid causing greater harm to their patients. The Latin phrase primum non nocere (“first, do no harm”) that all medical students are taught means that it may be better to do nothing than to risk causing a greater harm to a patient. Although all prescription medications have adverse side effects that can cause harm, practitioners have an ethical obligation to not prescribe medications that do more harm than good. The evidence we have reviewed suggests practitioners should exercise much greater caution in the prescription of antidepressants and to reconsider their use as a first line of treatment for depression. Additionally, we suggest that physicians and other medical practitioners should consider their potential legal liability. Legal liability for prescribing antidepressants Medical practitioners can be sued for prescribing antidepressant medications if doing so violates their state’s standard of care laws. In most states, the standard of care is what a “reasonably prudent” practitioner in the same or similar field would do. The standard of practice is not defined by what the majority of physicians do because it is possible for an entire field to be negligent. Since studies on the health risks associated with antidepressant use (e.g., stroke, death) have been published in well-respected medical journals, medical practitioners could possibly be vulnerable to malpractice lawsuits. For instance, it seems likely that a reasonably prudent physician should be aware of the medical literature and avoid prescribing medications that could increase the risk of stroke and death. Prescribers can also be held liable for not discussing information about medical risks so that patients can give informed consent for medical treatments and procedures. Prescribers have a duty to discuss the benefits and risks of any recommended treatment. Consequently, medical practitioners should discuss with their patients that antidepressant medication is only modestly more effective than placebo and could increase the risk of neurological damage, attentional impairments, gastrointestinal problems, sexual difficulties, abnormal bleeding, cognitive impairment, dementia, stroke, death, and the risk of relapse after discontinuation. Antidepressants must cause harm to create liability A medical malpractice lawsuit can only succeed if the antidepressant caused harm to the patient. It is important to realize that the antidepressant does not need to be the only cause of the harm—it only needs to contribute to or exacerbate the harm. As we have argued, antidepressants play a causal role in many adverse health outcomes because they disrupt serotonin, which regulates so many important processes throughout the body. This may make it particularly difficult for a medical practitioner to defend against a medical malpractice suit from a patient who experiences any of a number of adverse health effects while taking an antidepressant. For instance, if a patient has a stroke while taking an antidepressant, the evidence that antidepressants increase the risk of stroke suggests that the antidepressant may have contributed to the patient’s stroke, even if it was not the only cause. Conclusion The evidence now indicates that antidepressants are less effective and more toxic than commonly believed. From ethical, health, and legal perspectives, it seems prudent for individual practitioners and professional medical organizations to revise informed consent guidelines and reconsider the status of antidepressants in standards of care for many diagnoses and as the front line treatment for depression. With older people, for instance, the current data suggest informed consent must include a discussion of the increased risk of hemorrhagic stroke and even early death. We suspect that if prescribers realized they were placing themselves at legal risk for failing to discuss the adverse health effects of antidepressants with their patients, not only would they be more likely to discuss such information, they would be less likely to recommend these drugs in the first place. Paul W. Andrews is an assistant professor in the Department of Psychology, Neuroscience & Behaviour at McMaster University in Canada. He has a PhD in Biology from the University of New Mexico and a law degree from the University of Illinois at Urbana-Champaign. His work on the evolution of depression with J. Anderson Thomson, Jr. has been featured in the New York Times Sunday Magazine and Scientific American Mind. Taken with respect and gratitude. directly from ANNECWOODLEN’s Blog BEHIND THE LOCKED DOORS OF INPATIENTS PSYCHIATRY. http://behindthelockeddoors.wordpress.com/2014/01/12/you-and-your-antidepressant-2/
About Sacrifice and a Poem : Making Things Holy
MOSAIC
Mosaic: a word that means from the muses, from Moses and a work of art created from broken fragments of pottery, stone or glass.Even the first time, surrender was not hard,
though the grownups and mothers
with their drinks and swizzle sticks
undoubtedly thought it so when you volunteered
your only present that 10th Christmas
to a younger child who wouldn’t understand
being giftless at the tail end of a line to Santa,
nor your inherent sin in being born.
Such generosity should have stayed
between your concept-of-God and you,
but grownup admiration (you could not hope
to make your act unpublic) sullied the soap
of any generosity’s power to cleanse you.
Other atonements followed, only one
almost perfect, being perfectly anonymous
spoiled by an accomplice’s later telling.
Perfection? You never made that grade,
your terrible love for God demanding all life
from your life. No one told you, “Live a lot,”
not in words that made it matter, though
they doubtless counseled, “Live a little.”
You were always in school to be perfect,
never knowing that life is a classroom
where one learns to love flaws
by throwing bad pots, to shatter
them with careful hammer,
assembling beauty from broken things.
I do not believe I posted this poem here before. I may have but I doubt it as I was going to publish it in a print journal. Instead, I never sent it out. So instead I choose to “sacrifice” it here. (meaning: If i publish it online here I cannot do so in a print journal…so this is for you, folks!)
I am going to tell you about the child I was when I was very small, as small as I can remember. The first thing I remember about myself as a self, was…well, what do I remember? This is hard. For one thing, while I am down to only 5mg of Abilify, I still take 160mg of Geodon, but more important I still take 200mg of Topamax, an anticonvulsant that has known adverse effects on memory and cognition. Whether it actually interferes with what I can recall from childhood or not, I could not say…Perhaps ECT did that, 16 plus 5 sessions of ECT could have done a number on my brain, especially as I had active neurological Lyme disease at the time. The Lyme-literate neurologist advised strongly against ECT, but the hospital psychiatrist forced me, at least through the last 8, after I refused to go back, by getting a court order and drugging me on so much Thorazine I had no will.
Ah, but “They,” the faceless They of Authority, They say that ECT affects only short-term memory. Well, then, I guess just being 60 years old and having gone through trauma after trauma in the present decade alone surely could have wiped out memories from a half century ago and before. Whatever is the case, I must now scour my brain to recall what I thought I could recall easily.
Marjorie M, an old friend of my father’s, related a significant story recently — about me at age 6. Given our bedroom when she stayed with our family to recuperate from surgery, while my twin sister and I camped out somewhere else in the house, Marjorie was relaxing in my twin bed, alone, when she was surprised by my little face in the doorway. “Hi, Mrs M,” she tells me I said. “Why, hello, Pammy. How are you?” I looked at her with concern. “Are you all right, Mrs M? Are you lonely? Do you need anything?” (or something to that effect..) I am astonished that even at age 6 I knew I needed to “do this,” although I think that my mother, who disliked Marjorie intensely, was probably ignoring her and I suspect knew it even then. But Marjorie says she fell in love with me at that moment. She certainly never forgot the incident. Bless her heart…
I forgot it, likely I never knew or understood its impact. Given that I was six, I had already made the decision the year before, when Martha was born and I was five years old, that since I would never have the older sister of my own dreams, I would instead have to be the older sister I dreamed about for Martha. I made myself the promise to Martha, the day she was brought home from the hospital, that I would do everything in my power to be in Martha’s older sister the OS I would have wanted.
In all our childhood photos, until the year I turned 14 and stopped permitting photos to be taken, you see two things: I am almost always featured next to Martha, with my arms around her or somehow touching her, protective of her, and my twin sister is with the dog or otherwise occupied. Always. You might not be able to tell which twin is which from our facial features, but you can tell us apart from that. One of us is with Martha, and you know I am that twin for certain.
It is the greatest loss to me, the worst thing, the — I can only say this: I am not a quitter, but I was unable to complete that most important of assignments because of what happened to me in high school, whatever you want to call it. I either became ill, or troubled or had too many problems…whatever it was, I simply could not function well enough to do all that I promised myself (and Martha) I would do for her. I could not BE the person I needed to be, the functioning adequate teenager, in a good enough way to be a good enough older sister to her.
For instance, just take the older sister/younger sister Q and A that ought to have taken place but never did after I was 14. My own menstual periods took me by brutal surprise. In addition, I never did learn “the facts of life” (ie sex) as we called it in those days, not for real, not so I understood them, until after college. I vaguely knew the “birds and the bees” but not really, not so I understood the fundamental mechanics of sex at a time when most teens were experimenting with relationships for real. (Not me… I went to an all-girls high school and even though it was not necessarily true for the other students, for me, sex was never on my mind, I never understood the urge or the drive, not then and frankly not ever…) Given those facts, you can see that the OS/YS tête-a-têtes about sex and dating etc just were not going to happen. I didn’t know enough, one, and two, even if I had, I was unprepared to talk about anything so intimate with anyone.
As it turned out, though, Martha had plenty of friends and soon clearly found people to talk to when I could not. Thank heavens, because if the roles had been reversed, she could have taught me plenty! Only they could not be reversed, because I was the OS and she was the YS and things had to stay that way… I think to this day, though she doesn’t say it in so many words, she misses, if not resents, losing the OS, the me she once had…She misses surely the OS promise she knew I made to her from the outset.
Oh, Martha knows it wasn’t my fault. Life is life and shit happens. But she misses me, the Pam that never quite panned out because of everything that “happened” after I turned 14, 15, 16 and then it went on and on and on…She reminded me recently that even before I was taking any medication I told her that life was a minute by minute, hour by hour, day by day struggle just to survive…and I was only 24 or 26 or…This horrified her. To this day she can scarcely bare to recall my telling her. Or of seeing me catatonic in the State Hospital. She left crying and I think could not bear to visit again for years…
We create our reality, people tell me. Our thoughts are very powerful…If so, I created from a very young age, a very harsh reality, one where in cahoots with a punitive God, I had learned over the years I had to be selfless to the point of self-obliteration, as well as nearly mute. But not so mute as to be noticeable…because if you were noticed then you were not completely self-less. (I told you it was a harsh world…) I had to speak just enough so as to NOT be noticed, but never about me or my concerns. ONLY about others…and then listen to their problems ONLY. I had to be a pair of ears pinioned to the wall. Wear drab no-color colors, unnoticeable. Fade into the woodwork, but only in a way that was unremarkable…As soon as someone noticed that I was fading, it was evil! and I had to add just enough color to fade into the crowd anonymously yet again, self-lessly.
No wonder my handwriting almost disappeared into invisibility. (I would have willed my fingerprints away if I had been able to!) Can you imagine my mortification, and the self-mortification I had to practice when bank tellers noticed the minuscularity of my signature and made me sign checks a second time? They NOTICED my attempts to disappear, and in doing so, made me appear loud and big…which was bad. So the voices took it out on me, making demands that had to be answered and hidden in turn.
Why am I writing about these things? Because despite the pain it has caused me, I still believe in self-denial. I believe in self-lessly doing things for others, and in NOT being the center of our own universes ALL the time. I think a good bit of doing for and thinking about others in THEIR universes is good for the soul, so long as they do not abuse you. And I do not believe that others need to know everything good that we do. I do not think we need to broadcast every good deed on Facebook or to our friends so they know what good people we are! So what if it remains anonymous, or between God and you? Maybe even God doesn’t need to know it if you do something for someone else…and that someone else doesn’t need to know who did it either.
Live with the anonymity. You can do it. You can be self-less once in a while and not die. Your self is strong enough tolerate not telling the world everything you do for others…Trust me. You do not need kudos, confirmations or smiles for everything you do. You just need to know that someone else is better off because you did something or gave away something you could have used, but decided to give it to someone else instead. You sacrificed something. Not that you gave it away because you could not use it but because someone else needed it more than you did.
Try it, a little sacrificing especially in the United States is a good thing to learn. But make it real, don’t do it falsely. Giving up time or giving away something you don’t use or have any need for is no sacrifice. Sacrifice: from the Latin, sacer, “holy” plus facio, facere, “to make.” Something is only a sacrifice, something is only made holy, if it is a real loss and a real gift at the same time.
Today’s Art Journal Pages:West Farms Mall: You are Here…PLUS



Despite the MALFUNCTION picture above, there was nothing at all wrong with my ipad…I simply didnt understand the three finger tap function. But once i did, all was well. And the geniuses at the Genius bar were blessed again. I left to do the drawing of the West Farms Mall, rather than waste the 25 minute drive it had taken me to get over there.
That said, I need to add that I did one thing this weekend that Martha, my youngest sister picked up on immediately and knew at once was the wrong call, so to speak. She is an emotional genius of the highest order, and I dunno how, but somehow wrote me a text message that gave me permission to solve the problem…
To make the story clear, let me explain that it has LONG been part of my ethic that if I treasure something, especially a THING, I make a practice indeed a habit of giving it away. This is in part so I do not get attached to things, and so that I am not ” allowed to have any particular beloved items” that I need too much or covet too much. A form and practice of self-denial that runs very deep and started when I was remarkably young. I won’t go longer into this practice now except to add that as I wrote in my art journal on one page, one summer a few years ago, I took my very first vacation that was not a “hospital vacation” but was instead a planned stay at a Arts and craft camp called Snow Farm up in Florence, Massachusetts, where I signed up for a metal jewelry course. I already knew how to do the basics, but what this course promised was to teach sawing and riveting and soldering of metals, something I could not do at home.
Martha, who is five years younger than I, lives very close to Snow Farm, and without her support I never would have survived my weeklong stay. Partly because it turned out that I was much too paranoid to eat in the dining room, so she supplied me with enough food to make do with “canned” that is to say mostly fresh and decent food in my single room in the sleeping quarters. Late at night I would creep down to the emptied dining room and make myself a large PB sandwich to supplement these as well, from the supplies that were left out at all hours. But except for the one time the APRN who was then the manager of Snow Farm actually came and got me for supper and the other time that Martha also went with me to eat, I made do alone…
An equal hardship, one I am less able to explain, is that during the entire weeklong course, no one in the class of mostly women, more or less my age, spoke to me. They were a chatty bunch and talked a lot among themselves, but not a person said a thing to me, except I think one woman, towards the end of the week, offered the use of her tools or something, which became the occasion of a final breakthrough. But for the most part it was a lonely awful time.If it hadn’t been for the teacher herself, Abigail, who spent time with me (she knew my background from my application). I’d have withered from sheer isolation, both self- and other-imposed.
The final hardship was that I was very thin at the time, and using a metal saw required that one hold it against the chest wall while tightening any replacement saw bands and at other times as well. For some reason, I kept breaking my saws, which were delicate enough that if you twisted it while sawing a copper sheet, it could snap in a second. But holding the saw in a vise against my chest wall was simply impossible: It caused me exquisite physical pain, and I could not withstand the pain long enough to replace a single blade. So I had to give up learning to saw, and thus never learned to rivet either. Anything that involved the saw was simply beyond me. Either nobody observed the problem, or all decided that it was not worth coming to my aid. In any event, I was left with no alternative but to do the only thing I was able to finally do: to solder silver rings.
Yes, when it turned out that I could with ease hammer silver half-round sterling into a ring shape and solder it together into a permanent ring, and no one placed a limit on how many I made (since we paid for silver materials as we went along) I simply made silver rings for the rest of the week. Then the one woman who was semi-friendly with me gave me a few sterling silver pre-made bezel cups that would hold a 3 mm cabochon, were I to obtain them. And the teacher showed me how to solder the bezel cup onto a couple of my rings finally as well, (I could never learn to make my own bezel cups because that involved sawing…)
I left Snow Farm with about ten rings, two of which had soldered-on bezel cups. Some were big enough for men, the others were varying women’s sizes, but all were 100% sterling silver. None were anything mind you but amateurish, but that mattered little to me or anyone I gave one to. No one knew the difference, and if I did, it ceased to matter. I ordered little cabochons of grade A lapis lazuli, the lovely blue stone that is so famous, and managed to secure two of them into the two rings with bezel cups on them in a fairly decent if untutored manner (no adhesive used, that much I was proud of).
But of course, one of these lapis lazuli rings was in due course given away to a friend who was on and off not a friend. and who verbally abused me in such fashion that it was from her that I learned the awful language and names that I called the nurses and aides at Natchaug and Yale. (I hate the fact that I even have the c__nt word in my working vocabulary. I never did before this friend who is no friend of mine used it on me…But once heard as an name-calling term of verbal abuse, it became “valid,” it became part of my language…much as I wish it had never. And now I confess that when enraged at the people at the hospital, but ONLY then, I call them c––nts and variants on the terms rather freely, because I know what a terribly word it is and what effect it will have on them. (Chip my brother roared with laughter when I told him I called the single nurse restrained me for walking away from the quiet room at the IOL a “snarky little c––nt” and praised me for being able to laugh too. but in truth I wish I did not even have the word in my working vocabulary at all. I would prefer a lack of insults to use on people to being able to hurt anyone with this word…)
Now this “friend” is out of my life and I have the single ring left,..my single remaining treasure from that troublesome perfect vacation.
But what happened at the end of that vacation? Well, the last night, we were told to make something for the camp auction and so I brought earring making equipment and starting making a slew of those, and that, plus the fact that I’d brought over a copy of DIVIDED MINDS, finally just to introduce myself (I think the woman who had given me the bezel cups had asked me a question and elicited the fact that I had written two books…wanted to see them). Well, this was what finally broke the ice. And it did it in a major way. People were really interested, and curious. And they now asked me questions and seemed less scared to talk with me, as if the book’s subject matter somehow explained “everything.” I dunno…Maybe it did and maybe it didn’t. But the last day there , with the auction and the final dinner went fine. and I would say that I “love Snow Farm” despite everything.
Which is why I treasure that one remaining lapis lazuli ring. It means that I actually made something from a situation that could have been unmitigated disaster. I made lemonade from lemons, and I survived a vacation all on my own. SO when I managed to practically beg Martha, my compassionate genius of a younger sister to take this ring from my finger…she was dubious to begin with. For one thing, she has her own two important rings. One is her own gift to herself for surviving Breast Cancer…and it is her most important ring. But I practically made her take my ring from me. I think I have done this to her before…And she didn’t want to take it then either….She KNOWS things, this wonderful sister of mine, and either it is in part that she has these other rings of her own, or that she has inklings about my propensity to give my treasures away to others (I love) she is not and has not been a willing taker of my ring on either occasion.
What a good egg, This night I received an email from her saying she wanted to “trade it back to me” or at least have each of us wear it so she wasn’t taking it from me…But she knew, she knew. I dunno how, but something told her that it was not just ANY ring I made. God knows I have made her things, and she had accepted them. So she isn’t just refusing to take anything I made. no. I made the papier mache hummingbird JUST FOR MARTHA after all. And in point of fact she knew that I didnt want to part with Christobelle or the Using Klimt collages, but felt okay about taking them as long as she paid me the full price that I was asking…. (Actually I feel like shit, not just giving the collages to her! But that is another story.)
But the ring, oh the ring is so different. HOW DID SHE KNOW that the ring was different? It is not that my offer was false. I wanted her to have my treasure. I did. I loved giving it to her. It is just that I also know that I missed the ring, and wanted also to have it too. And in that sense alone I regretted my impulsivity. And the need to impoverish myself and deprive myself just because i had to. WHY? WHy am I not allowed to keep my ring, symbol of so much? Would it kill me to keep it? Would it be such a terrible mortal sin to allow me to keep my ONE treasure? It isn’t that precious, after all. The solder seam is visible on the bottom not under the bezel and it is a pretty shoddy piece of handmade jewelry. Not worth a nickle to anyone, in reality. Even the lapis cost me all of a dollar or two. So why does it cost me so much emotionally to keep it??????
Martha gets it, though. She really did and does. She KNOWS. She knows the real value of the ring is not the monetary value, but what it means to me. And that is why she is uncomfortable keeping it. The ring aint worth shit, not qua ring. It is only worth something as memory and as symbol and then only to me…and to Martha by extension and because of her depth of understanding.
Martha, if you read this, i hope I understood you correctly. You certainly got me on the dime. Thank you from the depths of even my impoverished dried up little heart for understanding. You deserve a ring far better than any crappy lapis ring I could ever make…You are a sister beyond dreams. Thank you…I really love you more than I can say.
Schizophrenia Video: UVA and DIVIDED MINDS
This video was made during our “book tour” of 2005-6 after DIVIDED MINDS: Twin Sisters and Their Journey through Schizophrenia was published. I had not seen it for several years when my good friend, the poet Mizzy Hanley, located it by chance on YouTube. I am surprised, frankly by how eloquent my speech is, though I cringe, today, at some of the things I said. How differently my talks today are! In any event, much of it still holds true, though now I would couch things in somewhat different language, and might not so readily give the voice of certainty to such statements as “I suffer from schizophrenia.” Nevertheless, the comments underneath are certainly encouraging, and if it helps anyone for us to have said what we did then good.
Donna’s Story and More Art
This picture is Tim’s sister in law, Dawn, whom I drew at Christmas, in 2012. It took me about an hour. The elephant below is remarkable only in that it is my first painting, in oils, that I have ever done. And for that matter, almost literally the first time I have painted anything, except for a few portraits. I usually draw, in pencil or oil pastel. I have painted some acrylic portraits, in the past, but none recently, as I told myself I’d better learn to draw a few years back “before I go any further with painting.” I never ever did anything with oils at all. So if I achieved any success with the elephant it was completely by chance. I find oils very difficult. I do not know how to work with them, nor how to manipulate a brush or the colors, or how to do anything at all with paint. So this is an interesting journey, and transition, if transition it be. I do not know what will happen. Whether I will switch to oils completely, or simply use them desultorily…We will see. I am now working on another elephant painting, just for practice. Both of them started with the use of oil pigment sticks, which enable a sort-of drawing technique, very bluntly, and ended forcing me to paint, using either my fingers or real brushes. So it seems I am being led willy nilly to the brush and paint pot!
This last picture started as a doodle that I did of another patient at the Institute this winter, but I liked it so much (and the patient hated it!) that I finished it by changing her to make her unrecognizable. I would have given it to her otherwise, but she didn’t want it, so I said nothing more. But I gave it to my friend Bill, who loved it. In the mean time, I figured I would finish it as I wanted to and did. I love it myself, and would gladly have kept it, had no one else expressed interest in it. But once I knew Bill loved it, well, I knew I wanted him to have it. And it meant I took extra care finishing it when I did. I never really knew much about this patient’s story, nor about anyone else there. Nor did they learn much about me. I do not believe they ever knew what the staff was doing to me that last ten days, when they kept putting me into four point restraints. That was the point: I was in seclusion so no one had any idea I even existed by that time. No wonder I ended by screaming non stop and blood curdlingly that last night when they restrained me the second time for no reason. Everyone who had known of me had left by then. All the patients were new, and no one even knew I was there. I was aware of it, and I knew that if I didn’t scream, they would simply four point me for another 8-10 hours and get away with it…Well, enough of that. This patient did not mind my drawing her, for the few hours that I was allowed to be in the general population. In fact, I think she was flattered that I wanted to. Unfortunately, she was not pleased by the results of my efforts when she saw the drawing…and made her feelings clear when she saw the drawing.
___________________________
One of my loyal blog readers, Donna, wrote a long comment the other day, and I asked if I could post it on the blog proper, as I felt it was important for her story to be heard. She said Yes, and so I am reprinting it here.
“I have many personal arguments against taking antipsychotics. First of all, I endured schizophrenia since I was about 10 yrs old without anyone knowing anything about it. Without being diagnosed, that is. Yes, I had been thought of as weird and even retarded by my peers, mostly because of social anxiety and being an extreme introvert that were a result of or in addition to the schizophrenia. But my sanity hung on the fact that I was creative and could physically exercise to the point of exhaustion. I think that exercise (running) was the most potent antipsychotic I have ever experienced, probably due to the release of endorphins and the subjugation of ongoing anxiety for a few hours. The hallucinations never really bothered me because I couldn’t remember being without them. Nevertheless, once doctors knew of the hallucinations, that became their excuse for medicating the hell out of me. And subsequently robbing me of my creativity and the ability to exercise. You can see where this is going.
For one thing there was exercise equipment in the hospitals I began to frequent (after starting on antipsychotics, of course.) but I could not use it without a doctor’s prescription, which was never forthcoming. I guess they didn’t put much stock in exercise. It can’t be patented and marketed and sold as a pharmaceutical. Once I began taking Zyprexa, the option was moot anyway, because I gained so much weight there was no possible way to run anymore.
Although I had schizophrenia, as I said, for many years before diagnosis and treatment, I was always able to read voraciously, retain what I had read, and use that as grist for the mill of creativity. Once I started taking mood stabilizers (which, btw, never stabilized my mood) like Lithium, Depakote, and Tegretol, I began to REALLY suffer mentally. Yes, I could tolerate hallucinations, but what I found intolerable was the side effect of being unable to be intellectually stimulated. I was laid low. I could no longer read and understand the combination of words. I couldn’t sit through a movie because I could no longer process the sensory input — what I saw and heard became separate entities rather than combining seamlessly into a meaningful whole. It was a frightening, assaultive experience. Even music ceased to be soothing. All I wanted to do, and practically all I DID do was to lie in bed just trying to think one clear thought. It couldn’t be done.
After the antidepressant and mood stabilizer failure, ECT was tried. Again, that only made things worse. Then came antipsychotics. The first one I took, Trilafon, was a nightmare. Kind of like what you said, Pam — I then had an inability to tell dreams from reality. The scary kind of hallucinations started, like seeing a gargoyle when I looked in the mirror. And the parade of multiple antipsychotics drifted ineffectually past the window of my consciousness. Finally, when I was given Zyprexa, I “awakened.” Would I have needed awakening if I had never started taking these medications in the first place? I had my doubts. But on Zyprexa, I could read again. I could tolerate movies. I could write creatively. But the weight gain that started with Lithium began to really pile on with Zyrpexa. My weight doubled within a few months. I had always been extremely weight and diet-conscious. With Zyprexa came mind-numbing sedation and a tremendous 24×7 appetite. So I was eating and sleeping, but I was also reading and writing.
Talk about the horns of a dilemma — I could take the medication and regain my ability to think and create but be a slave to the fork, spoon and pillow, or I could stop taking medication and keep my appetite and weight within normal limits and be insane. What I’m wondering now is whether any of this would have been a problem if I had never taken the medications to begin with. I became much more insane after being medicated and stopping the medication. To my way of thinking, medication had stopped the positive symptoms but had made me especially prone to relapse every time I tried to ease back on it. And the hallucinations had never been much of a problem — not nearly the problem of weight gain and intellectual poverty. Zyprexa did at least give me back a portion of my mind. Medication giveth and medication taketh away; blessed be thy name pharmaceuticals.
SInce then, I have tried just about ever atypical on the market, with the exception of Invega, hoping to find the “right” medicaiton. They were all promising at first, but each with an array of intolerable side effects. Anxiety. Hypoglygcemia. Hypothyroidism. Akathisia. Pruritis. Mania. Severe insomnia. And for a long time, I could return (somewhat relieved) to Zyprexa and what had become my standard of recovery — stabilization and the ability to think and sleep again.
Now, however, I refuse to take the previous 40mg of Zyprexa. My psychiatrist seems to believe the higher the dose, the more effective the medication. I have weaned myself down to 2.5mg which is enough to keep me out of the hospital but apparently not enough to keep my appetite so revved up. It does not allow me to lose all this weight, no, but at least I am no longer gaining. I am writing again. And reading. The problem is, this dose of Zyprexa does not solve the problems of anxiety and insomnia, which are pure torture. So I take the minimum dose for several days, then double that for a couple of nights in order to sleep, then back again. I used to just stop taking the Zyprexa completely because the weight gain frustrated me so much. The stigma of mental illness is bad enough without the stigma of obesity. Schizophrenia is bad enough without metabolic syndrome or diabetes.
The real kicker, to me, is that yes I was having problems before I ever started on the psychiatric medication rollercoaster. I had some psychosis, depression, hypomania. I heard voices once in a while. I had a roster of impossible people renting space in my head. But I lived a close-to-normal existence from all outward appearances. I could hold down a stressful job. I managed to keep a marriage together. I was winning regional poetry contests in my spare time. I had my own home. But it was not until I began taking all of these medications that it all went to hell. And now, from what I’ve read and what I have experienced, my body can no longer tolerate being without the medications. Life is worse off of them now than on them. I have to take Zyprexa or go back to the hospital. I have to take it or I may end up living on the streets. I have to take it or risk killing myself. My doctor says oh, but the medication has SAVED you from these horrors. But am I where I am today — on SSDI, unable to work, a slave to my fat-bound body — because of antipsychotics and antidepressants? Or am I able to be independent, sane, and creative again because of them. Or both? Somehow, something doesn’t seem right.
At Yale Psychiatric Hospital: Respect, Dignity and Kindness
Large picture I did at Yale Psychiatric Hospital, the second one.
The pictures below are actually only 2.5 by 3.5 inches and are artist trading cards. I drew many of them, especially when I did not feel like working on my larger drawings at the hospital.
In mid-February, after a week out of the hospital (and you can read about my hospitalization by scrolling down to the previous post, but, in brief, this had been at Hartford Hospital’s Institute of Living, during which I was kept in seclusion for the larger part of a four week stay and put multiple times, sometimes twice a day for many hours in 4-point restraints. Why? Why? Although I ONCE threw a chair, they told me it was for “not following directions.” To add insult to injury, every incident in which they restrained me was accompanied by three injections in the buttocks of Haldol, Ativan and Benadryl, despite my policy of passive, completely non-violent non-resistance.)
In any event, in mid-February, after I had spent just a week at home, I became acutely psychotic again, and in consultation with the only doctor I trust, a friend drove me to Yale New Haven Hospital’s emergency department. There, after a very long and arduous wait — alas, I cannot say much that is good about Yale’s ED. It felt like the psych/alcohol patients – and there were no discriminations made between the drunks and anyone else — were lined up on their beds in the hallway like buses at a terminal for what felt like “miles.” In fact at one point there was probably a line 15 gurneys long snaking around the corner until I could not see the end.
I was there for two and a half days, maybe longer, I do not recall. In fact, I remember nothing about my ED stay after I was finally “admitted” to the actual psych portion of the ED, as opposed to the hallway. I believe I was finally given medications, but also that I was no longer permitted access to my artist crayons, which meant that I only wanted to sleep and likely did until I was admitted to the Yale Psychiatric Hospital, a street or two away.
To say that my experience at YPH was an order of magnitude better than it had been at the IOL or even at Natchaug Hospital is truly not to give YPH enough credit. I scarcely want to mention the other two hospitals in the same sentence, that is how different Yale is and I say that even though I once considered Natchaug my “gold standard.” No longer, no longer. I think Natchaug was decent once, but only because of the civilizing and humanizing effects that the director of nursing, Sharon Hinton, APRN, had on the hospital. Once she left, the whole place went to pot, as evidenced by my experience during the last two stays, which went progressively from bad to terrible without her there…literally without her protection I was brutalized by a dehumanizing medical staff that had been left to do whatever it wanted to on its own, to hell with the consequences to the patients.
Be that as it may, and we know that the Institute was never humane, Yale took me completely by surprise. I was hard to surprise, and hard to convince that they were for real in their gentleness and kindness, let alone in their determination to treat me and everyone there with respect and dignity. I was certain that they would prove me right, that SOMEONE would be put into restraints, that someone would be violent enough to push their buttons and get 4-pointed. But it never happened, not in the entire three weeks I was there. Not even when a patient threw a punch or a push. Not even when a patient screamed bloody murder or used foul language. Nothing that earned me or anyone else seclusion or restraints elsewhere even came close to pushing the staff’s anger buttons at Yale. Instead, they persisted in using persuasion and gentleness and kindness…and if anyone lost it, if anyone became angry and could not keep it together, so far as I could tell, that staff member took themselves away from the situation to cool down, and did not take it out on the patient.
The most amazing things happened. No one forced me to do anything. Not even to take medication. I agreed to take it, after some discussion with the doctor and social worker…but when I evinced some doubt about the side effects, instead of pooh-poohing them as the doctor had at the Institute, Dr Milstein agreed with me, saying that the Zyprexa definitely increased appetite, and that it was not imaginary or something that was in my control, the way Dr Banerjee did at IOL. Instead, he and the other team members not only agreed to help me control what I ate, but went out of their way – I believe they actually went “Stop and Shopping” – to provide me with my own private supply of raw vegetable snacks in the staff refrigerator to eat at any time of the day…just so I wouldn’t have to be tempted by the hospital snacks of Doritos etc.
Dr Milstein asked me not to worry about what they did or did not do “extra” for me, and I tried not to. But when two large bottles of brand name Diet Coke kept appearing for me every day, and when the resident was sent to buy me batteries for my personal pencil sharpener (with a grinder not a blade), just so I could continue to do my artwork and not rely on the staff to sharpen my pencils in the back, well, I knew 1) they were truly watching out for me and treating me with TLC, or what certainly felt like extraordinary care, and 2) they were in fact spending “extra” money, if not indeed their own money just to supply these special needs…All of which – or NONE of which would have mattered at any other hospital or to any other staff. If I had no pencil sharpener, who would care? If I had to eat hospital food, who gave a damn? Dr Banerjee basically said it was MY fault and only my fault if I gained weight on Zyprexa, that none of his other patients, the good ones, ever did. But at Yale, all these matters were important to me, and so they were important to Dr Milstein to to Chris Simpson the social worker and to the other team members. Not just as a matter of words, but to be taken care of so I could both take the Zyprexa and do art.
Just as important, Dr Milstein took at least a half hour every single day, and I think sometimes it was more than that, simply to talk with me and listen to what I had to say. Even if it was only to rant about how badly I had been treated at the IOL. He repeatedly told me that he just wanted me to learn to trust again, to believe that not everyone was against me or would hurt me…And if I did not learn that precisely, I did eventually come to believe that the staff at Yale were trustworthy and kind and meant what they said about their NO restraints and NO seclusion policy, for everyone. I may had still had frissons whenever someone screamed or threw a fit, panicking, believing that 4-point restraints were finally going to be resorted to. PTSD is not that easily overcome after all. But I grew more trusting, and by the time of discharge, I was able to thank them all for everything, to know that they had gone out of their way for me, and not feel too guilty.
I did a fair amount of art while I was at Yale Psychiatric Hospital. I will post more in the coming days.
Art created at the Torture Chamber called the Institute of Living at Hartford Hospital
I was a prisoner at Hartford Hospital’s Institute of Living’s Donnelly 2 South from January 10th until February 7th, 2013, the day before the east coast blizzard, and I only “escaped” because the torturing doctor went on a four day vacation and the substitute decided that I was not actually psychotic any longer and did not need seclusion or restraints after all…and opted to let me go the very day I was freed from both.
Good thing too, because it was a Thursday and all travel stopped the very next day and for several days after that. The picture above is one that Shedana, RN liked very much. She said it captured her “physique” and while the flooring is imaginary, the unit was structured much as it is pictured. At least while I had a bed on the unit, with my door facing the med room and another bedroom opposite. Shedana was a “good egg” but of course it didn’t help when they decided to attack me in force and secluded me for two weeks and worse…But more on that later.
The first doctor I had merely convinced me to take, semi-voluntarily, a fairly stiff dose of Zyprexa. which I tried to do with regularity. I soon found, however, that far from being the miracle drug it had once been, mixed with Abilify and Geodon it induced a state of apathy and boredom. As if the Intake and Feeding drug, the drug on which I used to feel enthusiasm to learn and read, Zyprexa, simply mixed very badly with the Output drugs of Geodon and Abilify, such that I neither could read and learn, nor do art or write. In any event, this abysmal lethargy pushed me out of desperation to paint this, in oil pastels.
After that, I simply started refusing to take the Zyprexa, and refusing a lot of other things…A great deal of abuse happened. But I did this picture before all my art supplies were confiscated for no reason other than punishment (you cannot damage yourself or others with soft oil pastels)
Before I tell you some of what happened, without naming names, lest a legal case be made against them, as there might possibly be a chance to do, let me show you most of the rest of the art I did there, though one of them is unfinished and may never end up being finished, since it was hospital art and may stay that way.
This one is an oil pastel, me with a dung beetle pushing a ball of shit around on my cheek…Says enough just that, doesn’t it.
This one can be turned any which way to see all sorts of things buried in the picture. It was the one I started first and never did get to finish. What I can point you towards is the central object at the very bottom, which you can trace up to the blue figure and see what is happening. It should tell you something…The hand on the upper left is pointing at this process. Also, the exploding biohazard ball is part of it all, representing me, the all-polluting biohazard…But you have to look at the picture carefully. There is a Boat To Nowhere, and there are a couple of turtles, why, I don’t know…yadda yadda.
Finally, the very last time I had access to any art supplies, and I do not recall whether it was my last morning or some other time, I painted this one with oil pastels. I believe it speaks for itself.
What happened was that they were routinely, literally routinely restraining me “for not following directions” as they would quite openly state. Four-point restraints, in a tight no movement position, for many many hours at a time, with absolutely no indication of how, just how, I might “earn” my freedom. Of course they wouldn’t tell me what I could do to “be good” because I hadn’t done anything to ‘deserve” restraints to begin with as they knew perfectly well. For example,. and this was typical, but it was one of the few opportunities I managed to document because they ha removed all my writing materials, illegally, but I forgot that I had a right to a crayon and paper until Feb 6th. That afternoon, I simply walked away from my seclusion room. I had had enough of them saying it was “merely a side room” not a seclusion room, then preventing me bodily from leaving it. So when I could do so without someone actually wanting to fight me, I walked away, and proceeded to enter the unit and walk down the hall to the end and look out the window, I took a deep breath, heard THEM behind me, and sauntered back to the proper end of the hall, the “lost end” where they kept anyone from seeing me or knowing what they were doing to me. Once I got there, they descended on me, the horde of the goon squad, some staff I knew, but most I did not. I did not bother to look at who was doing what to me. I simply lay passively on the bed, and put my arms out so they could do what I knew they would do. Tightly, they shackled my wrists out past my hips so there was no play in the restraints and I could not turn on my side or do anything but lie stiffly on my back. At the same time, others jerked my feet apart and just as tightly shackled my ankles to the lower corners of bed. Then came the coup de grace. They pinioned me on my side somehow, pulled down my pants, and injected me with three drugs: Haldol 5mg, Ativan 2mg, and Benadryl 50mg. Why, except as punishment I do not know. because I had, just a half hour before, been doped up on involuntary Zyprexa 10mg.
But of course it was punishment. The very fact that they told me it was “not punishment” but “what your behavior brings on every time, Pamela” only proves my point. At first and usually they only said, it was because I “didn’t follow directions” so if they were not punishing me, what were they doing? They most certainly were not following Centers for Medicare and Medicaid regulations for the use of Restraints and Seclusion only in cases where a person is in imminent danger or harming self or others! Indeed, the best they could do, when I protested, passively, saying just those words, was to respond, “You are not safe” as if that proved somehow that I was in danger or posed any imminent threat to the safety of anyone.
No, I did not. I didn’t threaten or harm anyone. I merely walked the length of the hall and looked out the window and then went back to my solitary confinement. But it was enough to trigger their retaliation, and that started at 1pm. I was not released, not even to use the bathroom or eat supper, no never even was a single hand freed to permit me to eat supper — until 7pm.
THEN, at 8:30pm, I became upset and frustrated because — well, I do not know now why, but I “threw a half a graham cracker at the wall” as I recorded later. And the goon squad descended on this dangerous patient again, not only with the strait jacket of four point restraints, but with the same 3 drug IM-in-the-ass cocktail.
This time, however, passive as I was as they trussed me up — and I said only, “For shame, for shame. You ought to be ashamed of yourselves, doing this to me…” — passive as I was, allowing them to seize my limbs and tightly shackle me yet again in truth I dared not resist, as that would only have justified their violence, and i already had my share of bruises. Bur I had come to my limit of the abuse i would silently tolerate. They could restrain and seclude me but they had up till now only silenced me in restraints because iu wanted to earn my way free quickly. THis time I didn’t give a damn. It was nearly nine o clock and no one knew what they had done to me. Everyone was getting their bedtime meds and going to bed without any understanding of what was going on. I was a stranger to most people on the unit, who had no idea I even existed. THAT was a situation that had to change. NOW.
After they trooped out of the room, stationing a 1:1 sitter at the door as usual, I stopped my merely silent and passive resistance and started to scream. I wanted to be heard. I wanted to scare people. I wanted them to wonder, Who is that person,. and what in god’s name are they doing to her? Are they torturing her? And I wanted them to ask questions of the staff that the staff could not answer. I screamed and I screams in desolation and despair, feeling like my life was at an end. The plan they had set up for me was impossible for me to live up to. In nearly 10 days I had not even earned my way to a pencil and my journal. Only to restraints and more restraints. I saw no way out of the hospital. So I screamed, long blood-curdling, heart-wrenching screams that I assume did the job of scaring all, as eventually they closed my door, much to the disgruntlement of the sitter who was forced to come inside with me and was no longer free to socialize. But not for a while. I kept on screaming until my voice gave out and I felt asleep.
The next day the substitute doctor freed me, I dunno why or how, but she did. and I thank my lucky stars as the staff doctor was a sadist and never would have. I have a lot more to say, but for now I am hoping to hear from a sympathetic lawyer who will take on my case for some reason for some purpose…Unlikely to happen. despite my bruised body and joints that are so out of whack I cannot sit indian fashion or cross my legs. Why won’t they help me or respond? I didn’t die, so they won’t earn a lot of money from my case, nobody gives a damn about mental patient abuse…
You really know when you are a third class citizen when you only MIGHT be worth more to them dead than alive.