Am I opinionated or what? But someone has to SAY these things!!! Peace!
Pam
Am I opinionated or what? But someone has to SAY these things!!! Peace!
Pam
I do not know where this photo came from originally nor who made it but i obtained it from Sarah Grace Wolfram’s facebook page, so i am crediting her. In any event, what it says means the world to me.
I DID NOT CHANGE…IN FACT, MAYBE I NEVER NEEDED TO CHANGE, I JUST WOKE UP…to the fact that the world i had been living in was wrong.
I don’t know what to do. My skin is thinner than gossamer yet people think i am thick-skinned and hide-bound as a hardbound book packed with information and feeling nothing. They have no idea i feel everything from the words people speak to the experiences they have and they describe. I feel it all in and under my skin down to my marrow, i feel, how to explain the knife-edge sensitivity of my life? When Jesse blithely talked about breaking glass and stepping on it, the shard penetrating his foot, MY FOOT felt the glass pierce my arch and plunge straight up through my entire foot until it broke the skin at the top of my foot, and i had to muffle my scream of pain so i did not embarrass myself…it is always this way.
I do not “like” dogs but i feel them too. I feel them! I know where they need to be scratched under their chins and between their ears…always. And why? Because i myself feel it under my chin and between the ears. I love cats, yes. Dogs and cats both understand that i feel them. All animals know that i feel them. But it is too much for me. To feel everything and all that pain. In medical school i could not draw blood from another student because i was too inexpert at it and i felt the pain i was causing him…and despite my hardened exterior, i feel everyone’s pain and sensations, except perhaps their pleasure….i might be able to feel that too, but i distance myself from that because it feels like an intrusion on their privacy. When teddy lays his head on someone’s shoulder, i can feel that pressure on my shoulder. I do not know whether Teddy feels pleasure or relief, that is to say, viscerally, i could feel it, but i must not enter that feeling because it is too private.
I also know what people are thinking. I read people’s minds. They speak what they think to me, and i hear it out loud because they think too loud, but then i get confused between their thoughts and what only i can hear and i respond to what i heard out loud. Then things go haywire, because they say they never said such a thing, and others agree, and i look “crazy” because they did only think them. But in fact, i did hear them think it and they spoke it to me out loud with their thoughts, and my only crime was not knowing the difference and responding out loud. In such cases, they always have the benefit of plausible deniability, and i have nothing…but the truth of knowing what i know, which is that i know what is really going on.
This exquisite sensitivity is both a gift and a curse. Over the years the brutality of hospitals and “treatment” has forced me to try to ignore what i feel or at least pretend to. But things keep happening between me and others that force me to know more than i would ordinarily — if i did not have this gift/curse — want or have to know.
I was always told, “you are just paranoid” …”this is not happening”. And was made to ignore the reality of what i felt was going on around me, rather than speak about it and explore it. But i knew it was true, it was real, it was happening. You see, i feel people too, the way i feel animals, and i understand them, and i knew that they could not bear the fact that i heard their thoughts and knew what they really thought.
i always knew it was not paranoia, just truth they needed to conceal, due to fear and other difficult emotions. So they labeled me paranoid as a way to escape from admitting that i was able in fact to read their minds….
There is more but enough for now.
.
I have been asked, by The Recall Center http://www.recallcenter.com, see also http://www.recallcenter.com/xarelto/side-effects/ to “talk about my medications” so here I am, talking about my “favorite psychotropic drug, NOT..”: Abilify.
Why do I take Abilify?
I take Abilify, well, why do I take Abilify? I was prescribed Abilify because of the diagnosis of schizophrenia many years ago, and I usually take it along with another anti-psychotic drug (Geodon). But frankly the reason that I, I myself, take Abilify for now has nothing to do with psychosis or schizophrenia. I take Abilify simply and only because I have this weird feeling that it helps me write and do art. Ever since I have been taking it, or the two drugs together, I have had no trouble doing art at any time or even writing when I want to. The extra plus is that I can finish longer term projects, ones that I start on one day and have to finish over time. In the past this was a problem, but it seems to not be so difficult for me any more. I do not know for certain whether this is due to the effects of the Abilify/Geodon combination, but it feels like it, since I was never capable of finishing projects so easily and reliably before then. On the other hand, I believe that I can do these things myself now, and that once I get used to living here, in my new state of Vermont, I will choose to sloooowly go off the medications for good.
How do I remember to take my medicine?
In truth, I often forget to take my medications, but for the past thirteen years I had a Visiting Nurse come to remind me. And now that I live in another state, where this service is not available, I have a med tray that is delivered weekly. I hope that I will be able, by seeing this tray openly on display on my table, to remember to take the ones I want. At least for as long as I want to take them.
I have been asked about side effects of this drug, but I would say, 1) all “side effects” of drugs are the effects of the drug, and you cannot tell a person that she is only suffering “side effects” especially if they are serious enough to cause distress. 2) there are very serious and troubling effects possible with Abilify, so my experience is not necessarily typical 3) I used to feel very irritable on Abilify, but no longer 4) usually I add Geodon to help me sleep and calm the anxiety that Abilify can induce
Where do I go for Medical support? I just a few weeks ago moved to Vermont, so I do not yet have a Primary Care Provider, but I do have a psychiatric nurse practitioner who will see me – so far, at any rate – once a month. For medical issues, at this time, I do not know whom I will see, but in Connecticut I used to have an APRN at a doctor’s office. I also was able to get to an Urgent Care center easily, in CT. That is not possible here in rural VT. So in the event of a medical emergency, I do not know exactly what I would do, except call 911 and hope for the best!
Before taking Abilify, or ANY anti-psychotic drug, here are the questions that I think you should ask your doctors: You should ask, first of all, why he or she is prescribing an anti-psychotic medication for you. Does he or she believe you are psychotic? If not, why prescribe such a powerful and possibly devastating drug? And if so, why? Doctors should be willing to answer this openly and honestly and if they will not, then I do not believe that you should listen to their advice, but get a second opinion. You never know who might derive financial gains from prescribing a medication that is not available generically. Also, why is your doctor not being honest with you? I would never feel comfortable in a situation like that…
Ask your doctor what to expect after taking this drug and when to expect the effects, good or bad. What does he or she anticipate you will experience as a benefit and what he or she thinks you might experience on the down side? Ask them to be honest about this and why they feel it is worth the cost/benefit ratio to you.
Abilify is extremely expensive and non-generic until 2015, when a generic form is scheduled to become available. So if you can, I would ask your doctors about why they are prescribing this particular drug and not another. There may be very good reasons for it, such as a low incidence of weight gain, and little sedation, at least at doses below 15mg. Nevertheless, I would want to be certain that there were no financial inducements such as stock holdings in the pharmaceutical company involved etc.
There are ALWAYS risks involved when you take pscho-active medications, or any drug, but anti-psychotic drugs can be especially problematic for some people. Even though Abilify causes fewer problems with massive weight gain, for many people this is not always the case and weight gain as well as Type 2 diabetes, with or without weight increase has been known to occur on Abilify. Over-activation and irritability have been reported frequently, in my experience. And many people I know who have taken Abilify have told me that they have trouble sleeping if they take it at night.
Published research suggests that 30mg of Abilify is no more “effective” than 15mg. From my own experience, I can only say that at 15 mg Abilify is quite activating but at 20-30mg it becomes suddenly sedating and less helpful. This is why so many people refer to Abilify dosing as “Less is more.” They mean in some sense that the lower doses work better than the higher ones, unless the sole goal is sedation, in which case I would say there are better drugs for that purpose and safer ones.
As for drug interactions, I am not aware of any important ones.
Finally, the three main things I wish I knew before taking Abilify are what I wish I’d known before I took ANY anti-psychotic drug many years ago: that if I took what they gave me, and kept taking it, 1) I might be disabled for the rest of my life 2) it might induce chronic/episodic psychosis – i.e. stop the natural process of recovery in its tracks 3) NOT that my brain’s neurochemistry was already “out of balance” but that my brain and its neurochemistry would be changed and destabilized by the drug itself…
That is what I wish I knew before taking Abilify. Before I take any drug from now on, I will find out these things and determine for myself whether the cost/benefit ratio really makes sense.
But on the whole I would say that NO DRUG developed in the last 20 years has been adequately or honestly researched for any pharma company to make a claim about either its efficacy or its safety. NONE. So I would on that basis probably never take a new drug from now on. There is not a drug company out there that I trust to have done ANY new brain research, since it’s all based on junk and garbage theories that arose from “back researching” Thorazine, which was bogus in the first place. So why would I want to take a drug that was developed from research coming out of that cesspit?
I am 62 years old. I am NOT suicidal and I certainly do not want MDs with murder on their brains to euthanize me with their psycho-drugs, or to use me as some guinea pig to determine how much control they can have over people…NO MORE DRUGs, NO MORE DOCTORS, NO MORE HOSPITALS AND HOSPITAL ABUSES.
I may take a couple of drugs today in order to survive the transition from CT to VT, but you must understand that my brain was already damaged from the years of having been given them against my will. So I HAVE AN ALREADY DAMAGED BRAIN, from the medications I’ve already taken.
I do not advise anyone with a more or less intact brain to take an anti-psychotic drug, not ever, not if you can avoid it and certainly not for “the rest of your life.” NEVER take any drug on an ongoing, “forever” basis. ALWAYS re-evaluate your need for it.
And that is all I am going to say about Abilify. If you take Abilify for “depression” you have come to the wrong place. Nevertheless, I have written a blog post just for you. Do a search on “Add Abilify” and you should find it. But you won’t like it any more than this one. Sorry about that.
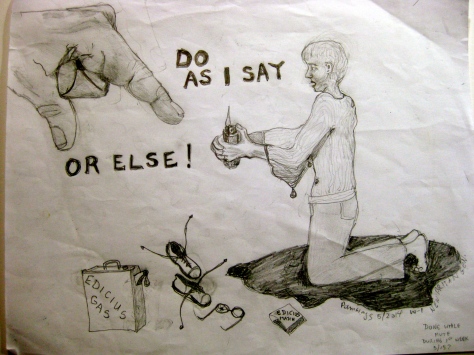
CLICK ON THE PICTURES TO ENLARGE THEM.
There were few rewards for behavior that toed the line at New Britain General Hospital (HOCC). Mostly it was punishment. If I was found with even a stub of a forbidden pencil, I was carried off to the Supermax seclusion cell, stripped naked and left alone.
At that point, being teeth-chatteringly blue with cold, I would swat a nurse in such a way that she would feel assaulted and bring on the goon squad of “I want to hurt someone today” guards to put me in four point restraints.
Why would I induce this? Because then they would at least cover me up afterwards with the mercy of a sheet, for modesty not warmth mind you, and I would beg for a blanket in vain. But at least my body would be protected from head to toe from the blasts of the A/C up full bore, and I could rest after I had had screamed out my lungs and my despair for a lonely twenty minutes or more.
No one cared, no one heard or paid any attention. The doors were double, and the cell was utterly soundproof. NO one ever even knew I was locked in there. When my screaming was too heart-wrenching for the softer ones of the staff down the hall in the room where they had retired to, they simply turned down the monitor and intercom so they didn’t have to listen.
I know, because I heard when the telephone rang, telling the person sitting outside the inner door they could turn it back on now (after I had quieted down). This was brutality of the nth degree. But they always called it treatment for safety, though I mentioned the CMS regs to the security guards one day as they were inflicting their usual pain in order to bring me to the room, and they stopped in their tracks.
“You’re kidding,” one said, “Its true that the only legal reason for seclusion is Imminent Danger to self or others?” (I had been brought there for disturbing the peace…)
I nodded, Look it up. She looked gravely at the others. but proceeded o do what she had been ordered to do anyway. And I proceeded to behave in a wildly immodest and terrified fashion likewise…knowing I would be left alone and freezing for at least two to three hours, no matter how fast I calmed myself.
They didn’t care. it was PROTOCOL…




I understand now why Dr. Michael E. Balkunas, the psychiatrist at New Britain General Hospital (Hospital of Central Connecticut) W-1, general psychiatry, gave up on me. He decided, even after eliciting my brother’s opinion both from a professional and a personal standpoint, and Dr Angela’s equally professional opinion that I do not suffer from Borderline Personality Disorder, to diagnosis me secondarily as exhibiting that disorder.
Oh, he knew I had come in with an acute exacerbation of schizophrenia and that I had PTSD. He knew that I had in my electronic medical record documents stating from other psychiatrists that I do not and never did have any personality disorder, despite in-hospital “behaviors.” But I know why Dr Balkunas diagnosed one. He did it for the same reason the other hospitalist psychiatrists have done it in the past: 1) in order to justify the use of a Behavioral “Treatment” Plan that was tantamount to torture and 2) to excuse his liberal use of seclusion and restraints in instances when they went against all CMS regulatory guidelines. And 3) in order to dismiss me and call my behaviors “manipulative and devious” instead of taking me and what I said seriously.
I also suspect, for all the second shift RN Barbara’s telling me that Michael Balkunas MD is a caring man and “never gives up on a patient” that he DID in fact give up on me. In fact I suspect that he never really tried to deal with or treat me at all, that from the first time he resorted to seclusion and restraints, he knew he had opted to terminate any treatment alliance.
But how did I figure this out? Well, it isn’t as if there ever had been any kind of alliance between us. From the first day after he admitted me from the ER, when he came into my room while I was still mute, he just walked away, saying dismissively, “I won’t talk with you unless you speak.” Immediately I understood that this man was willing to jeopardize everything about me and about my treatment in order to assert his power.
The same thing came into play after I began speaking about a week later. Now the issue was that he would not speak to me, would not deal with me at all but would immediately leave the room if I became angry and spoke with anything resembling a raised voice. (Argh, this was so many shades of Amy Taylor MD at the Institute of Living last year! — and Dr Balkunas tortured me in similar ways with predictable ineffectiveness — but powerful people behave in predictable ways, right? It seems I must have threatened their sense of entitlement. Why else take it out on me? Who am I? I’m a big fat nobody! They could have ignored me or just treated and released me, like anyone else. But instead they did their damnedest to crush me and destroy me. Why? Because in the end, I think I must have triggered some underlying feelings of resentment and impotence in these two psychiatrists and you know you do not threaten to unearth the feelings of a psychiatrist, or at least not with Michael Balkunas MD or with Amy Taylor MD …)
I learned very quickly, but not quickly enough, that everything about the Hospital of Central Connecticut W-1 Unit at New Britain was about coercion and control. Not about trauma-informed, patient-centered care. I don’t know how other patients managed to be discharged from there within a few days, but it would never have been possible for me. Mostly because I was simply too out of control to BE controlled by people who used such methods to undermine any possible calm and stability I might have achieved in those early days. They did NOTHING to help me but take away the very coping methods and objects that might have helped me. They used the carrot-and-stick method liberally, but mostly they used sticks. The very fact that the ED staff had seen fit to seclude me, give me IM meds twice and also to four-point restrain me naked to a bed tells you something about the brutality that reigns supreme there.
You know the very first thing I did was give the ER and the W1 staff a Psychiatric Advanced Directive. It was supposed to help them to help me. But instead they seemed to resent my knowing myself, and wanting them to know how to help me. They reacted badly and worked against it in every way possible, instead helping me. It appeared to anger them that I knew myself, and instead of using it, they did everything in their power to abrogate each and every section of it, right up to the section where it asked them to notify my doctor and my brother when and if they used seclusion and/or restraints despite the warnings.
No one ever called anyone in each instance that they chose to restrain or seclude me, even though I begged them to verbally at the time as well, and this document, which was at the front of my chart all along, stated in no uncertain terms that I wanted both people to be notified.
It was the worst hospitalization I have ever had, and I say that having had many serious and difficult stays. I was not just a difficult patient, I was a pain in the ass, but this was a direct result of the trauma I experienced in the ED and immediately following it on the floor. If I had not been traumatized, on the unit and in the ED, I feel certain that my “behavior,” outrageous, “disgusting,” and out of control as it was, would never have been so damaged. But because everyone saw fit to go against everything advised in the PAD, and do everything they could to re-traumatize me– even after I had a conversation with a nurse about my three experiences with date rape, even after that, she decided to seclude me, involving the forcible removal of me from my room by brute guards who bodily threw me into a cell without any mean s of communication with the world — because of this, they got the regression and degeneration and worsening of symptoms that my PAD predicted would happen. What did they expect? That I would simply thank them?!
I realized, though, the Monday morning of the week he discharged me when he came into my room and asked me how I was doing, that Dr Balkunas, who “never gave up on a patient,” had given up on me. Now, my brother had indicated to him that the “kindness” Dr Balkunas was offering to me by means of involuntary commitment to CVH would be devastating and destructive to the max. I think “Balkie” had had to think about the wisdom of actually sending me there. So he also had to think about whether he actually had any tools at all to “fix me” or cure me as he had promised. Indeed he was no miracle worker and had never held out anything, NOTHING AT ALL, by way or therapy or treatment modalities beside commitment to the state hospital to help me…so without that threat he had nothing to offer me.
The man never once sat down and even talked to me calmly and caringly. I say this because when he sallied forth with his usual opening that Monday morning, How are you? (I had decided finally, with my brother’s encouragement to “play the game.”) I answered with the socially acceptable, “fake” answer, my game plan, not expecting any real psychiatrist worth his salt to accept it, but trying to “play the game” anyway, as I was desperate to be discharged. My answer?
“I’m fine, thank you. How are you?”
Balkunas really didn’t bat an eyelash, the completely social answer was good enough for him, because he had given up trying to help me. Indeed, he had never even tried. So he proceeded, “How are you eating?”
“Fine.”
“How are you sleeping?”
“Fine.”
“Well, if things continue this way and there are no meltdowns I think you can go home on Friday.”
There were indeed meltdowns, even the night before I was discharged I had a meltdown over my supper tray. But Dr B was not on the floor much and didn’t hear of those, and everyone was so sick of me that they didn’t write them up, knowing I was to go home. And I persisted in answering those three magic questions “correctly.” Socially, as I had been taught, against my will, years ago. He never asked me a single other thing, and never talked about anything else at all after that.
The day of discharge came, and the great and caring Dr. Michael Balkunas popped his head into the room. “How are you?”
“I’m fine thank you. How are you?”
“Okay, I will write your discharge papers now.”
The very minute he said that and turned to leave, I put my sunglasses back on, as I saw that taking them off a week prior had served its purpose and it mattered not whether I wore them from that point on or not. I still wear them today, to protect people from my evil…
Dr. Michael Balkunas may talk a great game about helping people but he has very few tools to do so and really it is all pretence. He has medications, which are by and large bogus (though he has been educated by Big Pharma for so long he fails to understand this), and he had commitment proceedings to the state hospital, unless he happens upon a millionaire family willing to spend on their family member. I was not one of those, nor worth it. CVH – for those who are not in the know, CVH—Connecticut Valley Hospital is the last state hospital and the only long term facility for adults on Medicaid in Connecticut – being sent there would have killed me and he and my brother both knew it.
The difference was that my bother was decent enough to care while Balkunas honestly thought it would be good for me to lose my life there. And that was his treatment? Bullshit. He was a bad doctor and despite the cant, he gave up on me to boot. Well, thank god he did.
But you know, I do not forgive his accepting my social “I am fine thank you. How are you” so easily. That was insulting. He was sick of me, and considered me willfully manipulative and devious, otherwise he would not have diagnosed me with the damning BPD diagnosis, which in his hospital means just that you are a PIA, no less and no more. But he might have at least pretended to be a psychiatrist and not just a social buddy. How are you? Fine thank you, How are you? What sort of answer is that? ON the other hand, if he had asked me, what could I have said? We both know I had to get out of there and there was nowhere to go but home. He was not interested in finding out how I was, in talking to me. Not from the first. All he wanted was to medicate me. Which he did. So fuck me. How are you, I am fine thank you how are you? And it wouldn’t have made a rat’s ass worth of difference if I had not been okay, which I wasn’t, so long as I said I was fine, thank you, how are you’
Like I said, it was a game. That was the name of it, Play the Game…
So fuck Michael Balkunas. He is worthless to me, and his add-on personality disorder diagnosis means less than a fig to me. He knew I had schizophrenia and PTSD. He knew the hospital was abusing me. He knows nothing about me, never spent more than 3 minutes with me on any given day. He knows nothing. And I don’t give a flying femtogram about HOCC (the former New Britain General Hospital) except insofar as they ought to ask me back to educate them and improve the situation vis a vis their abusive use of seclusion and restraints, not trauma-informed patient-centered care at all. However since even supposedly trained Nurse Manager Jessica came around to not objecting, and approving their use, I can see that it might be hopeless to do so. Willing though I would be.
Barbara, RN on the second shift. You alone were a lifesaver and a light in a dark tunnel. I wrote in the scraps of paper I called a journal of your kindnesses again and again, and I forgive your being blind to the cruelty of seclusion and restraints, because you have lived with that culture too long, You just need to be re-educated. But you saved my life. Had you not been on duty that weekend before I was discharged, I might not have calmed enough to say to Dr. Balkunas the socially acceptable “I-am-fine-thank-you-how-are- you” mantra that was the magic ticket out of there.
I know no one on W-1 remembers me with anything but relief that I am gone and a great deal of disgust and anger. Ditto for me. I still wake screaming from nightmares about the place and a great deal of anger that I don’t want to let go of. I want to hold onto it long enough to fix the situation of W1, before I forgive anyone. Then we will see.
But for now I am off to Vermont for six weeks to stay with relatives. I hope to heal. I hope I can heal…
Take care of yourself Barbara. You would do well to find a kinder and better place to work and train. I thank YOU for everything. I mean it when I say you saved my life and sanity.
Blessings on you alone, Barbara, the rest of you can FYandGTH.
Miss Wagner
I know this audio file may be difficult to understand, but this is what happens when the voices go haywire…I can’t speak. And I cannot even tell you what triggered it, but something did. I tried to go to a Voice Hearers workshop on Tuesday about Taboo and Dangerous voices, but i could scarcely enter the building. I had to “get permission” just to open the door, and when I did, I could not stay…Just could not stay. Forget it. I’m worthless.

Yes I actually managed to paint this picture — in gouache, not oils, true, but I did it, I picked up paints and brushes and from start to finish made a complete painting. This is a big step for me. True, I did the running shoes picture a bit earlier but that was really just a sketch. I have been drawing for so long, and so scared of painting that it feels really BIG that I did this, good or bad a picture though it might be. Sooooo, what’ja think? (By the way, it is a self-portrait – not flattering but hey…)
I THOUGHT THIS WAS INCREDIBLY WELL WRITTEN AND IMPORTANT INFORMATION. SEE CREDITS AT THE BOTTOM. Posted on January 12, 2014 by annecwoodlen THINGS YOUR DOCTOR SHOULD TELL YOU ABOUT ANTIDEPRESSANTS September 12, 2012 By Paul W. Andrews, Lyndsey Gott & J. Anderson Thomson, Jr. Antidepressant medication is the most commonly prescribed treatment for people with depression. They are also commonly prescribed for other conditions, including bipolar depression, post-traumatic stress disorder, obsessive-compulsive disorder, chronic pain syndromes, substance abuse and anxiety and eating disorders. According to a 2011 report released by the US Centers for Disease Control and Prevention, about one out of every ten people (11%) over the age of 12 in the US is on antidepressant medications. Between 2005 and 2008, antidepressants were the third most common type of prescription drug taken by people of all ages, and they were the most frequently used medication by people between the ages of 18 and 44. In other words, millions of people are prescribed antidepressants and are affected by them each year. The conventional wisdom is that antidepressant medications are effective and safe. However, the scientific literature shows that the conventional wisdom is flawed. While all prescription medications have side effects, antidepressant medications appear to do more harm than good as treatments for depression. We reviewed this evidence in a recent article published in the journal Frontiers in Psychology (freely available here). The widespread use of antidepressants is a serious public health problem, and it raises a number of ethical and legal issues for prescribers (physicians, nurse practitioners). Here, we summarize some of the most important points that prescribers should ethically tell their patients before they prescribe antidepressant medications. We also discuss the ways that prescribers could be held legally liable for prescribing antidepressants. Finally, we implore practitioners to update the informed consent procedure for antidepressant medication to reflect current research and exercise greater caution in the prescription of antidepressants.
Most antidepressants are designed to alter mechanisms regulating serotonin, an evolutionarily ancient biochemical found throughout the brain and the rest of the body. In the brain, serotonin acts as a neurotransmitter—a chemical that controls the firing of neurons (brain cells that regulate how we think, feel, and behave). However, serotonin evolved to regulate many other important processes, including neuronal growth and death, digestion, muscle movement, development, blood clotting, and reproductive function. Antidepressants are most commonly taken orally in pill form. After they enter the bloodstream, they travel throughout the body. Most antidepressants, such as the selective serotonin reuptake inhibitors (SSRIs), are intended to bind to a molecule in the brain called the serotonin transporter that regulates levels of serotonin. When they bind to the transporter, they prevent neurons from reabsorbing serotonin, which causes a buildup of serotonin outside of neurons. In other words, antidepressants alter the balance of serotonin in the brain, increasing the concentration outside of neurons. With long-term antidepressant use, the brain pushes back against these drugs and eventually restores the balance of serotonin outside of the neuron with a number of compensatory changes. It is important to realize that the serotonin transporter is not only found in the brain—it is also found at all the major sites in the body where serotonin is produced and transported, including the gut and blood cells called platelets. Since antidepressants travel throughout the body and bind to the serotonin transporter wherever it is found, they can interfere with the important, diverse processes regulated by serotonin throughout the body. While physicians and their patients are typically only interested in the effects of antidepressants on mood, the harmful effects on other processes in the body (digestion, sexual function, abnormal bleeding, etc.) are perfectly expectable when you consider how these drugs work.
Many people who have suffered from depression report a substantial symptom-reducing benefit while taking antidepressants. The problem is that symptoms are also substantially reduced when people are given a placebo—a sugar pill that lacks the chemical properties of antidepressant medications. In fact, most of the improvement that takes place during antidepressant treatment (approximately 80%) also takes place with a placebo. Of course, antidepressants are slightly more effective than placebo in reducing symptoms, but this difference is relatively small, which is what we mean when we say that antidepressants have a “modest” ability to reduce depressive symptoms. The pushback of the brain increases over months of antidepressant treatment, and depressive symptoms commonly return (frequently resulting in full blown relapse). Often this compels practitioners to increase the dose or switch the patient to a more powerful drug. Prescribers fail to appreciate that the return of symptoms often occurs because the brain is pushing back against the effect of antidepressants. 3. The risk of relapse is increased after antidepressant medication has been discontinued Another effect of the brain pushing back against antidepressants is that the pushback can cause a relapse when you stop taking the drug. This pushback effect is analogous to the action of a spring. Imagine a spring with one end attached to a wall. An antidepressant suppresses the symptoms of depression in a way that is similar to compressing the spring with your hand. When you stop taking the drug (like taking your hand off the spring from its compressed position), there is a surge in the symptoms of depression (like the overshoot of the spring before it returns to its resting position). The three month risk of relapse for people who took a placebo is about 21%. But the three month risk of relapse after you stop taking an SSRI is 43%—twice the risk. For stronger antidepressants, the three month risk is even higher.
Antidepressants can kill neurons (see our article for a review). Many medical practitioners will be surprised by this fact because it is widely believed in the medical community that antidepressants promote the growth of new neurons. However, this belief is based on flawed evidence—a point that we address in detail in our article. One way antidepressants could kill neurons is by causing structural damage of the sort often found in Parkinson’s disease. This neurological damage might explain why some people taking antidepressant medication can develop Parkinsonian symptoms and tardive dyskinesia, which is characterized by involuntary and repetitive body movements. Many prescribers mistakenly think these syndromes only occur in patients taking antipsychotic medications.
Recent research indicates that antidepressants may increase the risk of cancer outside of the brain, such as breast cancer. However, the neuron-killing properties of antidepressants may make them potentially useful as treatments for brain cancers, and current research is testing this possibility.
Since neurons are required for proper brain functioning, the neuron-killing effects of antidepressants can be expected to have negative effects on cognition. In rodents, experiments have found that prolonged antidepressant use impairs the ability to learn a variety of tasks. Similar problems may exist in humans. Numerous studies have found that antidepressants impair driving performance, and they may increase the risk of car accidents. Recent research on older women also indicates that prolonged antidepressant use is associated with a 70% increase in the risk of mild cognitive impairment and an increase in the risk of probable dementia. 7.Antidepressants are associated with impaired gastrointestinal functioning The action of antidepressants results in elevated levels of serotonin in the intestinal lining, which is associated with irritable bowel syndrome. Indeed, antidepressants have been found to cause the same symptoms as irritable bowel syndrome—pain, diarrhea, constipation, indigestion, bloating and headache. In a recent study, 14-23% of people taking antidepressants suffered these side effects. 8. Antidepressants cause sexual dysfunction and have adverse effects on sperm quality. Depression commonly causes problems in sexual functioning. However, many antidepressants make the problem worse, impairing sexual desire, arousal, and orgasm. The most widely studied and commonly prescribed antidepressants—Celexa, Effexor, Paxil, Prozac, and Zoloft—have been found to increase the risk of sexual dysfunction by six times or more. Evidence from case studies suggests that antidepressants may also interfere with attachment and romantic love. Some antidepressants have been found to negatively impact sperm structure, volume, and mobility. 9. Antidepressant use is associated with developmental problems Antidepressant medication is frequently prescribed to pregnant and lactating mothers. Since SSRIs can pass through the placental barrier and maternal milk, they can affect fetal and neonatal development. Generally, if SSRIs are taken during pregnancy, there is an increased risk of preterm delivery and low birth weight. Exposure during the first trimester can increase the risk of congenital defects and developing an autism spectrum disorder, such as Asperger’s Syndrome. Third trimester SSRI exposure is associated with an increased risk of persistent pulmonary hypertension in the newborn (10% mortality rate) and medication withdrawal symptoms such as crying, irritability, and convulsions. Prenatal exposure to SSRIs is also associated with an increased risk of respiratory distress, which is the leading cause of death of premature infants. 11\\10. Antidepressant use is associated with an increased risk of abnormal bleeding and stroke Serotonin is crucial to platelet function and promotes blood clotting, which is important when one has a bleeding injury. Patients taking SSRIs and other antidepressants are more likely to have abnormal bleeding problems (for a review see our article). They are more likely to have a hemorrhagic stroke (caused by a ruptured blood vessel in the brain) and be hospitalized for an upper gastrointestinal bleed. The bleeding risks are likely to increase when SSRIs are taken with other medications that reduce clotting, such as aspirin, ibuprofen, or Coumadin . 11. Antidepressants are associated with an increased risk of death in older people. Depression itself is associated with an increased risk of death in older people—primarily due to cardiovascular problems. However, antidepressants make the problem worse. Five recent studies have shown that antidepressant use is associated with an increased risk of death in older people (50 years and older), over and above the risk associated with depression. Four of the studies were published in reputable medical journals—The British Journal of Psychiatry, Archives of Internal Medicine, Plos One, and the British Medical Journal—by different research groups. The fifth study was presented this year at the American Thoracic Society conference in San Francisco. In these studies, the estimated risk of death was substantial. For instance, in the Women’s Health Initiative study, antidepressant drugs were estimated to cause about five deaths out of a 1000 people over a year’s time. This is the same study that previously identified the dangers of hormonal replacement therapy for postmenopausal women. In the study published in the British Medical Journal, antidepressants were estimated to cause 10 to 44 deaths out of a 1000 people over a year, depending on the type of antidepressant. In comparison, the painkiller Vioxx was taken off the market in the face of evidence that it caused 7 cardiac events out of 1000 people over a year. Since cardiac events are not necessarily fatal, the number of deaths estimated to be caused by antidepressants is arguably of much greater concern. An important caveat is that these studies were not placebo-controlled experiments in which depressed participants were randomly assigned to placebo or antidepressant treatment. For this reason, one potential problem is that perhaps the people who were taking antidepressants were more likely to die because they had more severe depression. However, the paper published in the British Medical Journal was able to rule out that possibility because they controlled for the pre-medication level of depressive symptoms. In other words, even among people who had similar levels of depression without medication, the subsequent use of antidepressant medications was associated with a higher risk of death. These studies were limited to older men and women. But many people start taking antidepressants in adolescence or young adulthood. Moreover, since the risk of a relapse is often increased when one attempts to go off an antidepressant (see point 3 above), people may remain on medication for years or decades. Unfortunately, we have no idea how the cumulative impact of taking antidepressants for such a long time affects the expected lifespan. In principle, long-term antidepressant use could shave off years of life. It is commonly argued that antidepressants are needed to prevent depressed patients from committing suicide. Yet there is a well-known controversy over whether antidepressants promote suicidal behavior. Consequently, it is not possible to reach any firm conclusions about how antidepressants affect the risk of suicidal behavior. However, most deaths attributed to antidepressants are not suicides. In other words, antidepressants appear to increase the risk of death regardless of their effects on suicidal behavior. We suggest that antidepressants increase the risk of death by degrading the overall functioning of the body. This is suggested by the fact that antidepressants have adverse effects on every major process in the body regulated by serotonin. 12. Antidepressants have many negative effects on older people Most of the research on the adverse health effects of antidepressants has been conducted on older patients. Consequently, our conclusions are strongest for this age group. In addition to cognitive decline, stroke and death, antidepressant use in older people is associated with an increased risk of falling and bone fracture. Older people taking SSRIs are also at an increased risk of developing hyponatremia (low sodium in the blood plasma). This condition is characterized by nausea, headache, lethargy, muscle cramps and disorientation. In severe cases, hyponatremia can cause seizures, coma, respiratory arrest and death. The fact that most research has been conducted on older people does not mean that antidepressants do not have harmful effects on the young. As previously discussed, antidepressants can have harmful effects on development. Moreover, many people start taking these drugs when they are young and remain on them for years or decades. In principle, the negative effects of these drugs could be substantial over such long periods of time. Altogether, the evidence leads us to conclude that antidepressants generally do more harm than good as treatments for depression. On the benefit side, the drugs have a limited ability to reduce symptoms. On the cost side, there is a significant and unappreciated list of negative health effects because these drugs affect all the processes regulated by serotonin throughout the body. While the negative effects are unintended by the physician and the patient, they are perfectly expectable once you understand how these drugs work. Taken together, the evidence suggests that these drugs degrade the overall functioning of the body. It is difficult to argue that a drug that increases the risk of death is generally helping people. There may be conditions other than depression where antidepressants are generally beneficial (e.g., as treatments for brain tumors and facilitating recovery after a stroke), but further research in these areas is needed (see our article). Ethical and Legal Issues Physicians and other medical practitioners have an ethical obligation to avoid causing greater harm to their patients. The Latin phrase primum non nocere (“first, do no harm”) that all medical students are taught means that it may be better to do nothing than to risk causing a greater harm to a patient. Although all prescription medications have adverse side effects that can cause harm, practitioners have an ethical obligation to not prescribe medications that do more harm than good. The evidence we have reviewed suggests practitioners should exercise much greater caution in the prescription of antidepressants and to reconsider their use as a first line of treatment for depression. Additionally, we suggest that physicians and other medical practitioners should consider their potential legal liability. Legal liability for prescribing antidepressants Medical practitioners can be sued for prescribing antidepressant medications if doing so violates their state’s standard of care laws. In most states, the standard of care is what a “reasonably prudent” practitioner in the same or similar field would do. The standard of practice is not defined by what the majority of physicians do because it is possible for an entire field to be negligent. Since studies on the health risks associated with antidepressant use (e.g., stroke, death) have been published in well-respected medical journals, medical practitioners could possibly be vulnerable to malpractice lawsuits. For instance, it seems likely that a reasonably prudent physician should be aware of the medical literature and avoid prescribing medications that could increase the risk of stroke and death. Prescribers can also be held liable for not discussing information about medical risks so that patients can give informed consent for medical treatments and procedures. Prescribers have a duty to discuss the benefits and risks of any recommended treatment. Consequently, medical practitioners should discuss with their patients that antidepressant medication is only modestly more effective than placebo and could increase the risk of neurological damage, attentional impairments, gastrointestinal problems, sexual difficulties, abnormal bleeding, cognitive impairment, dementia, stroke, death, and the risk of relapse after discontinuation. Antidepressants must cause harm to create liability A medical malpractice lawsuit can only succeed if the antidepressant caused harm to the patient. It is important to realize that the antidepressant does not need to be the only cause of the harm—it only needs to contribute to or exacerbate the harm. As we have argued, antidepressants play a causal role in many adverse health outcomes because they disrupt serotonin, which regulates so many important processes throughout the body. This may make it particularly difficult for a medical practitioner to defend against a medical malpractice suit from a patient who experiences any of a number of adverse health effects while taking an antidepressant. For instance, if a patient has a stroke while taking an antidepressant, the evidence that antidepressants increase the risk of stroke suggests that the antidepressant may have contributed to the patient’s stroke, even if it was not the only cause. Conclusion The evidence now indicates that antidepressants are less effective and more toxic than commonly believed. From ethical, health, and legal perspectives, it seems prudent for individual practitioners and professional medical organizations to revise informed consent guidelines and reconsider the status of antidepressants in standards of care for many diagnoses and as the front line treatment for depression. With older people, for instance, the current data suggest informed consent must include a discussion of the increased risk of hemorrhagic stroke and even early death. We suspect that if prescribers realized they were placing themselves at legal risk for failing to discuss the adverse health effects of antidepressants with their patients, not only would they be more likely to discuss such information, they would be less likely to recommend these drugs in the first place. Paul W. Andrews is an assistant professor in the Department of Psychology, Neuroscience & Behaviour at McMaster University in Canada. He has a PhD in Biology from the University of New Mexico and a law degree from the University of Illinois at Urbana-Champaign. His work on the evolution of depression with J. Anderson Thomson, Jr. has been featured in the New York Times Sunday Magazine and Scientific American Mind. Taken with respect and gratitude. directly from ANNECWOODLEN’s Blog BEHIND THE LOCKED DOORS OF INPATIENTS PSYCHIATRY. http://behindthelockeddoors.wordpress.com/2014/01/12/you-and-your-antidepressant-2/
April 16, 2014
Dear Harold Schwartz, Director of the Institute of Living at Hartford Hospital
I believe that I was profoundly harmed by the treatment I received in 2013 on Donnelly 2 South at the Institute of Living at Hartford Hospital, and that what the staff did to me was not only unethical and cruel but that it crossed the line into illegality from the very first. Psychiatric patient abuse is a pattern in Connecticut hospitals, but it was most egregious at the Institute of Living because the staff told me that they knew what they were doing was wrong but that they would get away with it anyway.
That I know I was a difficult patient never justified staff behavior towards me. I was loud and upset and hard for them to deal with, yes. That is precisely why my Psychiatric Advance Directive (PAD) was written out the way it was, and why I made my medical and psychiatric history online so available. When ill, I am frightened and paranoid, which makes me easily roused to irritability and hostility. I know this, from a distance as it were. But knowing this now does not mean I was in control of my emotions. I am by nature neither temperamental nor prone to temper eruptions or throwing things. In addition, I am extremely modest, hardly one to disrobe or urinate in public. My friends and family have at times variously labeled me “stoic” and “peacemaker,” which should tell you a lot. But that I disrobed and urinated on the floor on Donnelly 2 South both horrifies me and concerns me because these behaviors point to something going on distinct from my psychosis: they point to my having been subject to abuse and trauma at the hospital itself.
Let me make it very clear that if I have behaved in such ways before it was only in response to similar extreme circumstances – as when i was subjected over and over to restraints and seclusion in a horrific and sadistic fashion at Manchester Hospital in 2009 and similarly at Middlesex Hospital in 2010. It is too bad that when Sanjay Banerjee MD and Amy Taylor MD took it upon themselves to violate my HIPAA privacy rights and investigate my previous admissions, without my permission (which I expressly refused to grant) they failed to make the connection between the abuse, and my subsequent behaviors…It turns out all they drew as a conclusion was that if those hospitals could use restraints and seclusion ad libitum, so could they. It didn’t seem to matter to Dr Taylor in particular that in 2009 and 2010 measures such as seclusion and restraints not only didn’t work, they made things worse. Not surprisingly, when Dr Taylor followed these examples I regressed completely, just as my PAD predicted.
I was admitted to Donnelly 2 South, and I came in with a very detailed Psychiatric Advanced Directive as I said. I made it very clear that my online electronic medical record was also available. It included documents such as my narcolepsy diagnostic consult and special documentation assessing my need for a higher than usual dosage of Ritalin, written by my former sleep specialist, Mary B O’Malley, MD PHD who was also my psychiatrist from 2000-2009. Included as well was a letter she wrote to my present psychiatrist, Dr Angela Cappiello, explicitly stating her conviction that I do not have a personality disorder, NOS, borderline traits, or otherwise.
According to Dr. Sanjay Banerjee he read every page of these documents. That is what he told me. He even praised me, saying he wished every patient would come so prepared. Moreover, when he spoke with Dr. Cappiello, he brushed off my concerns about anyone misperceiving me as having a personality disorder. My brother, Philip Spiro, MD, himself a psychiatrist, brought up the same matter when in discussion with Laurie Denenberg, LCSW, but her response was much the same: “Personality disorders are not a part of the picture here. We intend to honor her PAD. We are glad that she has had the foresight to prepare such a document.”
If this was so, then how did it come to pass that Amy Taylor, MD wrote on my history and discharge summary that I have a “long history of Borderline personality disorder” and herself diagnosed “Personality disorder NOS with borderline traits”? I was being treated for four weeks for an active psychotic disorder Axis 1. In any event, she could have no way of knowing whether or not I had a personality disorder, given an active an Axis I diagnosis.
On or around February 4, 2013, I walked in frustration away from the quiet room where I had been held captive for nearly three weeks, strolled down the hall, looked out the window and slowly retraced my steps back to the quiet room, which I had been expressly told was NOT a seclusion room (the definition at Hartford Hospital’s Institute of Living of a seclusion room is a “room to which the door is locked.”) But when I arrived I was confronted by a cohort of staff who proceeded to 4-point restrain me to the bed, even though I was quiet and put up no resistance. Not wanting to give them any reason or justification, I passively lay down on the bed and placed my own limbs out for the restraint cuffs, saying, (I quote my journal entry made later that evening): “For shame. You ought to be ashamed of yourselves. I am not and never was a danger to myself or others.” Their response was “ You refuse to follow directions so we do not know what you will do. This is not punishment, Pamela, this is what your behavior brings on every time.”
From that point on, the threshold for restraints was extremely low. They always restrained me, spread-eagled, so tightly I couldn’t move a muscle. They never permitted bathroom breaks or even used a bedpan, instead they made me defecate in my clothing. They never even let my hands free to eat. I would fall asleep rapidly after three routine punishment needles in the buttocks: Haldol, Ativan and Benadryl—whether I just had my regular meds or not, and they would invent reasons to maintain me in restraints even after I had been asleep for hours. When I woke, groggy and hardly dangerous to anyone, they would grill me with questions that I could not answer. They would then use my inability to respond as reason not to let me out, even when I asked, as the chart recorded, in a “soft sedated voice” for release. They would re-inject me, to put me back to sleep instead.
In the evening on Jan 5th, for the second time that day, they brutally restrained me for throwing half a graham cracker at the wall. Then, as usual, they left me like that for six hours, even after I fell asleep. But in point of fact, though, I could never earn my way to release from restraints by good behavior or quietly, calmly asking for release. I had never done anything to earn my way into them in the first place. I was never violent until they threatened me. They refused to release me until I literally cried, “Uncle” when they told me to.
As to those vaunted “shows of force” what did they expect? Presented with a cohort of threatening staff personnel I saw one thing: an impending assault. I know they anticipated my panic; they said as much in my chart. Isn’t that the point of a planned “show of force” – to induce fear and panic? Why else do it? So why should it be any surprise, when I defended myself when they forcibly, physically grabbed me? When they stuffed me into a body bag and were trying to tighten the straps, surely you can understand why anyone would bite the hand of an attacker whose digits came near the face. I had done nothing but refuse to enter the body bag willingly. I simply was passive. I did not fight or resist until they grabbed my body and assaulted me.
But none of it should have happened. My Advanced Directive explained in exquisite detail exactly what to do and what I respond to better than fear tactics and force. In fact, It is beyond me, knowing that one of the admission diagnoses I came in with was PTSD, how anyone could possibly approve in advance, permission to use restraints and seclusion “just in case they are needed”. Why not counsel the person asking for this advance “right to restrain” to do all in his power not to restrain me and to work with the PAD instead?
Here’s what SAMHSA the substance abuse and mental health services administration publication has to say on seclusion and trauma:
“Studies suggest that restraints and seclusion can be harmful and is often re-traumatizing for an individual who has suffered previous trauma…
“Further, there is a common misconception that seclusion and restraint are used only when absolutely necessary as crisis response techniques. In fact, seclusion and restraint are most commonly used to address loud, disruptive, noncompliant behavior and generally originate from a power struggle between consumer and staff. The decision to apply seclusion or restraint techniques is often arbitrary, idiosyncratic, and generally avoidable.
“Moreover, some studies indicate that seclusion and restraint use leads to an increase in the behaviors that staff members are attempting to control or eliminate.
I have been traumatized, and not just by hospitals. I was date-raped three times in my twenties and experienced traumatic domestic abuse by a long-term roommate. The cover sheet on the PAD made very clear that due to these trauma issues, I could not tolerate being secluded or restrained without serious consequences: regression and serious worsening of symptoms. Unfortunately, as soon as the staff saw fit to use physical methods of coercion and control on me from the first time a staff member grabbed me and pushed me with his lower torso, I ceased improving, and my symptoms went downhill. Did they really think they were being kind and compassionate?
Staff violence begets violence….
I tried to get help even when on the unit, at least I tried when I was free to, to make calls or leave my seclusion… that is to say, forced three -week-long stay in the quiet room last winter. I made many calls to the hospital’s patient advocate office, but the sole time anyone made contact was when the advocate came to hand me some paperwork – I believe I was actually in 4-point restraints at the time — papers I could not read about the forced medication hearing. I needed her advocacy, but she never responded to my panicked calls in any way that was helpful to me. I wanted her help, but she never came by to ask me what I needed. She was less than useful, the fact that I had to go through her, essentially a hospital employee, and her refusal to respond, contributed to my ongoing panic and desperate feelings of aloneness and depression. No wonder Dr. Sanjay Banerjee attempted to force ECT on me, without any prior discussion of it with me whatsoever.
And where did the ECT discussion come from? My PAD states in no uncertain terms that I will refuse ECT under any and every circumstance. My brother would be my conservator if Banerjee had sought to go down that road, and he would never have made any decision to counter my wishes on that subject. If Banerjee really read my PAD, he would have known that. I have already had FORCED ECT and it traumatized me terribly. Also it failed to work.
Banerjee had stopped my 75mg of the antidepressant Zoloft during the first or second week I was there. “Do you really need that?” he had asked, “You don’t seem depressed to me.” Obedient, and in any event glad to get off any medication at any time, I shook my head, assenting to the change. A week later, instead of reinstating the Zoloft, Banerjee blamed my sudden “depression” on my refusal of the anti-seizure medication, Lamictal, a drug I had not taken in 6 months. Now he was applying to force me to take ECT, something I was terrified of, and to have calculated brain damageIt was this threat, and the brutality with which the decision was handed down, that started the downhill course of my IOL stay.
The very next weekday, all hell broke loose. When I entered the conference room, I pushed some important notes across the table that I wanted Dr Banerjee and Laurie Dennenberg to read. They refused, claiming that I threw the papers at them. Instead, Dr Banerjee proceeded to berate me, and told me how he had consulted with other hospitals and providers and had read my records against my instructions and Advance Directive, thus violating my HIPAA rights. Moreover, he threatened me with a behavioral treatment plan that would not permit me to do art or writing unless I “behaved.”
I hit the roof, telling him I would sue the hospital and complain to JCAHO, then summarily left, slamming the door, an act that stemmed from feelings of utter impotence, because I couldn’t actually say in words anything more effective.
It could have ended there. I could have been left alone, to cool down and calm myself. But, no, Dr Banerjee had to write for stat meds again, and even though I was on the phone and trying to find someone to talk to, to calm myself, I had to be physically dragged off the chair I sat on, away from the phone and brought to the floor in a physical struggle (because they had attacked first, i.e. physically grabbed me, I defended myself, instinctually). They could have waited for me to finish the call. They could have waited to see if I calmed myself. I was not hurting anyone or even threatening anyone or myself with harm. All that I had done, in terms of physical threats, was to throw a lightweight chair at the wall. And that, it was clear to everyone, was intended not as a threat to anyone. Furthermore, it was done and over with. I had left that area and gone to my room. I had then come back and now sat on the chair by the phone, speaking to my interlocutor on the other end. There was no need to pick a fight or encourage a struggle. A wait-and-see policy could have successfully guided the situation to a better resolution not only for the situation at hand but for the entire hospital stay. As the poem by Dylan Thomas goes: “After the first death, there is other.” Once they decided to use four—point restraints, there was no going back. The first time broke everything, So they used them again, and again, and more and more freely and without justification but for convenience and punishment.
Back to Feb 5 or 6, after sleeping for six hours, I was taken out of restraints conveniently just in time for a visit from Dr. Angela Cappiello, my outside psychiatrist. Observed by my 1:1 monitor, I only dared whisper and dared not tell the doctor the full extent of the abuse that had been happening. Nevertheless, she took one look at Amy Taylor MD’s behavioral treatment plan posted on my wall, and told me that it would be impossible for anyone, even someone who was well, to follow it properly. She was so worried about me, and about my ability to complete the treatment plan’s requirements, even for the required “24 hours,” that she intervened. The next day, the single day that Dr. Taylor planned to be out of town, Dr. Cappiello asked Dr. Mehendru to evaluate me for discharge, telling her that she feared a power struggle had been set up that I could never win.
When Dr. Mehendru came to see me, at first I was angry, as the chart indicates, thinking she was just another Taylor flunky, preparing to use more restraints and seclusion, But when she asked if I would like to go home, I took one look at her, saw sincerity in her eyes, and burst into a smile, ready to say yes to anything. Miraculously “cured,” I left the IOL that very same day, less than 12 hours after being released from 4-point restraints and not 4 hours out of seclusion.
However, I was not well. Within two weeks time, I was back in the hospital, this time admitted to Yale New Haven Psychiatric Hospital, via their emergency room. Over the next 3 weeks I experienced an entirely different kind of care. At Yale I did not find a staff ready to fight or try to seclude or restrain me.
I was still the same person with the same problems, loud and angry at times, even “violent” to property in my frustration, and still psychotic, yet they never responded with a show of force. Why would they? At Yale it would be absolutely anathema to deliberately frighten a patient. What would be the purpose in that, they would think. They also never pushed me into a seclusion room or strapped me down in punitive 4-point restraints, or any of the other ill-advised responses that my PAD explains are the worst things to do to anyone who is struggling, scared and paranoid. In point of fact, Yale Psychiatric Hospital’s Washington Square unit does not have a seclusion room. They also have a “restraints-free” policy, so they didn’t use those at all either.
The Institute of Living on the other hand with its “We only use restraints and seclusion if we have to” policy, restrained me countless times, and for many more hours than was even legal. When I woke up that last morning, the room opposite me was occupied by yet another person in 4-point restraints! That is because once you allow staff to use restraints a little, it only takes a little to use them a lot. And once you sanction the use of restraints and seclusion at all, it is only time before someone abuses them and abuse becomes the norm.
I would like your response to this letter, I have sent it to many people within the state government and outside of it, But you may have the first response. Also you may be interested in the youtube video of my artwork which can be found at this site:
Prior to when you allowed the staff to body bag and restrain me, when I had done nothing wrong but leave the non seclusion quiet room, and you refused to come to my assistance, you had asked to see my artwork. Instead you left me to be tortured. Well, here is some of the art you might have seen had you rescued me from my abusers.:
Sincerely
Pamela Spiro Wagner
The final one you never saw in featured in the post below this one.
This picture is Tim’s sister in law, Dawn, whom I drew at Christmas, in 2012. It took me about an hour. The elephant below is remarkable only in that it is my first painting, in oils, that I have ever done. And for that matter, almost literally the first time I have painted anything, except for a few portraits. I usually draw, in pencil or oil pastel. I have painted some acrylic portraits, in the past, but none recently, as I told myself I’d better learn to draw a few years back “before I go any further with painting.” I never ever did anything with oils at all. So if I achieved any success with the elephant it was completely by chance. I find oils very difficult. I do not know how to work with them, nor how to manipulate a brush or the colors, or how to do anything at all with paint. So this is an interesting journey, and transition, if transition it be. I do not know what will happen. Whether I will switch to oils completely, or simply use them desultorily…We will see. I am now working on another elephant painting, just for practice. Both of them started with the use of oil pigment sticks, which enable a sort-of drawing technique, very bluntly, and ended forcing me to paint, using either my fingers or real brushes. So it seems I am being led willy nilly to the brush and paint pot!
This last picture started as a doodle that I did of another patient at the Institute this winter, but I liked it so much (and the patient hated it!) that I finished it by changing her to make her unrecognizable. I would have given it to her otherwise, but she didn’t want it, so I said nothing more. But I gave it to my friend Bill, who loved it. In the mean time, I figured I would finish it as I wanted to and did. I love it myself, and would gladly have kept it, had no one else expressed interest in it. But once I knew Bill loved it, well, I knew I wanted him to have it. And it meant I took extra care finishing it when I did. I never really knew much about this patient’s story, nor about anyone else there. Nor did they learn much about me. I do not believe they ever knew what the staff was doing to me that last ten days, when they kept putting me into four point restraints. That was the point: I was in seclusion so no one had any idea I even existed by that time. No wonder I ended by screaming non stop and blood curdlingly that last night when they restrained me the second time for no reason. Everyone who had known of me had left by then. All the patients were new, and no one even knew I was there. I was aware of it, and I knew that if I didn’t scream, they would simply four point me for another 8-10 hours and get away with it…Well, enough of that. This patient did not mind my drawing her, for the few hours that I was allowed to be in the general population. In fact, I think she was flattered that I wanted to. Unfortunately, she was not pleased by the results of my efforts when she saw the drawing…and made her feelings clear when she saw the drawing.
___________________________
One of my loyal blog readers, Donna, wrote a long comment the other day, and I asked if I could post it on the blog proper, as I felt it was important for her story to be heard. She said Yes, and so I am reprinting it here.
“I have many personal arguments against taking antipsychotics. First of all, I endured schizophrenia since I was about 10 yrs old without anyone knowing anything about it. Without being diagnosed, that is. Yes, I had been thought of as weird and even retarded by my peers, mostly because of social anxiety and being an extreme introvert that were a result of or in addition to the schizophrenia. But my sanity hung on the fact that I was creative and could physically exercise to the point of exhaustion. I think that exercise (running) was the most potent antipsychotic I have ever experienced, probably due to the release of endorphins and the subjugation of ongoing anxiety for a few hours. The hallucinations never really bothered me because I couldn’t remember being without them. Nevertheless, once doctors knew of the hallucinations, that became their excuse for medicating the hell out of me. And subsequently robbing me of my creativity and the ability to exercise. You can see where this is going.
For one thing there was exercise equipment in the hospitals I began to frequent (after starting on antipsychotics, of course.) but I could not use it without a doctor’s prescription, which was never forthcoming. I guess they didn’t put much stock in exercise. It can’t be patented and marketed and sold as a pharmaceutical. Once I began taking Zyprexa, the option was moot anyway, because I gained so much weight there was no possible way to run anymore.
Although I had schizophrenia, as I said, for many years before diagnosis and treatment, I was always able to read voraciously, retain what I had read, and use that as grist for the mill of creativity. Once I started taking mood stabilizers (which, btw, never stabilized my mood) like Lithium, Depakote, and Tegretol, I began to REALLY suffer mentally. Yes, I could tolerate hallucinations, but what I found intolerable was the side effect of being unable to be intellectually stimulated. I was laid low. I could no longer read and understand the combination of words. I couldn’t sit through a movie because I could no longer process the sensory input — what I saw and heard became separate entities rather than combining seamlessly into a meaningful whole. It was a frightening, assaultive experience. Even music ceased to be soothing. All I wanted to do, and practically all I DID do was to lie in bed just trying to think one clear thought. It couldn’t be done.
After the antidepressant and mood stabilizer failure, ECT was tried. Again, that only made things worse. Then came antipsychotics. The first one I took, Trilafon, was a nightmare. Kind of like what you said, Pam — I then had an inability to tell dreams from reality. The scary kind of hallucinations started, like seeing a gargoyle when I looked in the mirror. And the parade of multiple antipsychotics drifted ineffectually past the window of my consciousness. Finally, when I was given Zyprexa, I “awakened.” Would I have needed awakening if I had never started taking these medications in the first place? I had my doubts. But on Zyprexa, I could read again. I could tolerate movies. I could write creatively. But the weight gain that started with Lithium began to really pile on with Zyrpexa. My weight doubled within a few months. I had always been extremely weight and diet-conscious. With Zyprexa came mind-numbing sedation and a tremendous 24×7 appetite. So I was eating and sleeping, but I was also reading and writing.
Talk about the horns of a dilemma — I could take the medication and regain my ability to think and create but be a slave to the fork, spoon and pillow, or I could stop taking medication and keep my appetite and weight within normal limits and be insane. What I’m wondering now is whether any of this would have been a problem if I had never taken the medications to begin with. I became much more insane after being medicated and stopping the medication. To my way of thinking, medication had stopped the positive symptoms but had made me especially prone to relapse every time I tried to ease back on it. And the hallucinations had never been much of a problem — not nearly the problem of weight gain and intellectual poverty. Zyprexa did at least give me back a portion of my mind. Medication giveth and medication taketh away; blessed be thy name pharmaceuticals.
SInce then, I have tried just about ever atypical on the market, with the exception of Invega, hoping to find the “right” medicaiton. They were all promising at first, but each with an array of intolerable side effects. Anxiety. Hypoglygcemia. Hypothyroidism. Akathisia. Pruritis. Mania. Severe insomnia. And for a long time, I could return (somewhat relieved) to Zyprexa and what had become my standard of recovery — stabilization and the ability to think and sleep again.
Now, however, I refuse to take the previous 40mg of Zyprexa. My psychiatrist seems to believe the higher the dose, the more effective the medication. I have weaned myself down to 2.5mg which is enough to keep me out of the hospital but apparently not enough to keep my appetite so revved up. It does not allow me to lose all this weight, no, but at least I am no longer gaining. I am writing again. And reading. The problem is, this dose of Zyprexa does not solve the problems of anxiety and insomnia, which are pure torture. So I take the minimum dose for several days, then double that for a couple of nights in order to sleep, then back again. I used to just stop taking the Zyprexa completely because the weight gain frustrated me so much. The stigma of mental illness is bad enough without the stigma of obesity. Schizophrenia is bad enough without metabolic syndrome or diabetes.
The real kicker, to me, is that yes I was having problems before I ever started on the psychiatric medication rollercoaster. I had some psychosis, depression, hypomania. I heard voices once in a while. I had a roster of impossible people renting space in my head. But I lived a close-to-normal existence from all outward appearances. I could hold down a stressful job. I managed to keep a marriage together. I was winning regional poetry contests in my spare time. I had my own home. But it was not until I began taking all of these medications that it all went to hell. And now, from what I’ve read and what I have experienced, my body can no longer tolerate being without the medications. Life is worse off of them now than on them. I have to take Zyprexa or go back to the hospital. I have to take it or I may end up living on the streets. I have to take it or risk killing myself. My doctor says oh, but the medication has SAVED you from these horrors. But am I where I am today — on SSDI, unable to work, a slave to my fat-bound body — because of antipsychotics and antidepressants? Or am I able to be independent, sane, and creative again because of them. Or both? Somehow, something doesn’t seem right.
This was the third picture I did at Yale. During the three weeks I was there, I often had a difficult time when I heard another patient yelling or getting angry. At one point, a young woman (younger than I at any rate) did a fair amount of screaming and complaining. And I heard a lot of noise that I thought portended or suggested violence was happening. I became very scared, terrified in fact, not because I thought I would be hurt, or that she would somehow hurt me. I am never ever afraid of other patients. My only fear at any time, aside from fear of the staff behavior towards me, is fear that another patient will be hurt or traumatized by staff use of seclusion or restraints or other violence on them.
Christine Simpson, the LCSW assigned to me on my team, recognized that I was panicking, and at least three times that day sought me out and just sat with me, talking to reassure me both that I was fine and that the other woman was fine, whatever was going on. She even came back before she went home to check on me and make sure I was okay before leaving, well after 5pm. I don’t think I ever thanked her enough for her support in the other posts, so I hope this does so. She was wonderful and I think she went out of her way to make sure I was not only “just okay” but that everything was as good as it could possibly be.
I am so profoundly grateful and remain astonished, both, that YNHPH has a philosophy of patient-centered care, of dignity and respect for the person, and also practices it so well that it doesn’t need to preach anything to the patient at all. You know, I believe the Washington Square 2 unit “advertises” itself online using the words Dignity and Respect, but I did not know this before I wrote my first blog post about yale or went there. I simply understood it from the way they treated me and everyone else. It was also perfectly obvious to everyone who visited me there.
I have donated picture #2, the one with the red bird of fear (“oiseau de peur”), to Yale Psychiatric Hospital, because of Chris Simpson and Dr Milstein and everyone else on the team and all the aides and counselors on the unit who work so well together. A huge thank you, to all of you.
Let me state this plainly so there is no misunderstanding: I am tired of people thinking there is something wrong with me just because I do not have a husband or boyfriend/lover or even a girlfriend/lover or a love-interest of any kind. I am not interested in sex and have never been interested in sex for whatever reason. This does not distress me and it never would have in the past, had others not insisted that it ought to. I have finally come to the conclusion that being asexual — definition: having no interest in a sexual relationship with another person — is okay.
I am not unhappy. I get a lot done and I am likely more satisfied by my life as an asexual than someone who is sexual and without a partner. I am never lonely. And I have tons of friends. (At least 16 friends — all of whom I adore — came to my 60th birthday party!)
It has taken me, via a tortuous up and down path, a long time to come to this position. And there may well be those who shake this foundation yet, as other people’s opinions, alas, still manage to have a strong effect on me. I have never told openly the story I am now going to relate, but I think it is time. It should be an eye-opener and a warning to those who believe they have the right, even the duty to “help” a young person discover “her true identity…”
As some of you know, a very long time ago, I was a student in a medical school in Connecticut. The two years I attended med school were extraordinarily difficult ones for me and I admit now that even as I matriculated, I “knew” at an almost conscious level that I would never get through. I didn’t honestly want to be a physician. Not really. Oh, yeah, I thought I could be a good psychiatrist. I knew that I understood people and mental illness enough to empathize and help others. But the notion that I could successfully get through four years of med school and four years of residency in order to achieve that goal was something I also knew would be impossible, even as I nominally attempted to undertake it. I had no choice. It was what you did in my family. And there was no question in my mind that I could work at a “regular 8-hour a day job.” I simply didn’t have the stamina either interpersonally or physically. I didn’t know why, I just didn’t. (I also didn’t understand that I had narcolepsy, so I construed my constant drowsiness as “boredom” for everything.)
So there I was in med school, without the ability to make friends or any interest in relationships, especially having just broken up with Bruce, the one boyfriend I had had and with whom I had sex (because he pushed it). I hated it…which was why I broke it off. I know I was noticed. I felt noticed. Possibly because I made little effort to be friendly, possibly because my narcolepsy made me noticeable. I don’t know. It is not that I was or am a striking person at 5′ 3″ and 105 lbs…hardly! Perhaps it was my mere aloneness that struck people. I dunno.
Things were hard to start with, but then the voices started up telling me to hurt myself and I acted on their commands, frequently. I had horrific nightmares nightly. And I could not stay awake in class or to study no matter what I did. People had all sorts of advice and jokes for me but no understanding. They gave me No-Doz and Vivarin for my birthday, which precipitated a caffeine-toxic all-night-up of horror. They took photos of “Rip van Winkle” sleeping on the med school lobby couch and published it in our newsletter. No one knew what was really going on, at home, at night, in my bedroom when the voices took over.
I had a run-in with the student health doctor, Dr E, to whom I had gone about possible Reynaux (sp?) Syndrome. When she saw certain scars on my body she became concerned and spoke with the psychiatrist I was seeing at the time. Dr S, who was a cold man who seemed to dislike me from the start, was angry at our next appointment for “parading” my wounds and warned me against ever doing so again.
I went back to Dr E and told her what Dr S had said. She seemed perturbed and gave me the name of a therapist that she said she often referred “troubled students” to. I might consider seeing Tamara instead of Dr S. The other students liked her a lot, Dr E said. What were their problems? I asked. Dr E shook her head and responded, Not so very different from yours.
I sit nervously in the waiting room, hoping that Tamara will be so late she won’t have time to see me today after all. I feel sick to my stomach and wonder why I’ve come. Five minutes late, ten minutes late. I am just about to leave when a very pregnant woman opens the door to the office and welcomes me in. I do not look at her face but whisk myself inside, trying not to guess how many more weeks she has.
Before she asks me anything, Tamara says, “Now, I see girls who like girls and boys who like boys. You’re okay with that?”
What is she talking about? I don’t understand. Girls who like girls? I like girls, I like boys. Why shouldn’t I be okay with it? So I say, yes. And assume that even so, she sees people whose issues are very different…
I didn’t ask her. I simply assumed that she had other interests. And went on from there. But it was critical, because I did not get that she was conducting therapy as if I had agreed that I was a lesbian, and yet I had made no such admission. I did not even understand what she was getting at. Why was she so coy? Why didn’t she just come out and ask me whether or not I was gay and then tell me that she only treated lesbians and gays with issues around their sexuality?
As it turned out, she had no idea that I was not in fact assenting to her coy proposition that I “liked girls.” On the contrary, if she had asked me point blank, I would likely have said, “Me? No way. I am not even interested in boys. I couldn’t care less about sex. I like, but don’t love, boys and girls…so to speak.” But the operant word, clearly, was not “like” at all, but love, as in “making love.”
Actually, in point of fact, I would not have been able to respond at all, if I remember my former self accurately. I was nearly mute much of the time, esp in therapy, and when I did speak it was often very cryptically and with difficulty making myself clear. This may account for the misunderstanding that so horrified me in what follows.
It was a crazy-making psychotherapy for about 6 months. I had no idea what notion she was operating under, because I didn’t know what kind of therapy she “did.” Likewise, if she knew the least thing about me, it was completely mis-colored by her mis-understanding of me as a lesbian. So when one afternoon she “told” me that she empathized with me, because I had had a sexual relationship with my previous psychiatrist…I hit the roof.
“WHAT? What the F— are you talking about?!” I nearly leapt out of my chair.
“It’s okay Pam, I understand,” she soothed me.
“It is NOT okay! I never said anything of the sort! This is YOUR filthy mind! I’m out of here. Go to hell!” And with that I got up and walked out. I realized then that she was nuts. Somehow she had gotten the entirely wrong idea, but I didn’t understand how. It made no sense to me. Where on earth had she fashioned that notion? I certainly had never said any such thing…
Then her statement “I treat girls who like girls…” came back to me. And I understood more. Dr E surely knew Tamara’ orientation, her clinical expertise, so Dr E must have believed that I needed to talk about conflicts about my “homosexuality,” about coming to terms with being a lesbian, unbeknownst to me. So she had set it up that I see Tamara, believing that she knew me better than I knew myself. But what right had she to do that? And how would she know whether or not I was a lesbian? Just because I was a conspicuous loner? How dare she? She knew nothing about me! What she had done was a violation of me as bad as any man who wanted to have sex just to prove he was Mr Right!
I spent a lot of time after that utterly paranoid that I might be gay, feeling that I must be gay, certain that I was gay…I even came to the point that I accepted it eagerly. But it was never true. It was just another identity forced on me by others who would not let me be. Who would not accept that I simply have never had interest in sex or sexuality beyond a pervasive non-sexuality. My libido, my psychic energy, is invested in other things, in art, in science and in life, but not in erotic interests. And you know what? Being non-sexual or asexual doesn’t make me an amoeba or less than human.
At least 1% of humanity is asexual, has always been asexual, permanently. That’s a LOT of people. We may not be the norm, but there are enough of us out there to rate your acknowledgement and the respect you would pay to any other human being. That’s all we ask, that’s all I ask. And for you not to try to change me just because you do not like it or understand my way of being. Thank you.
(For anyone who was reading the other post when it disappeared, sorry! There was a problem!!!!)
What is real? Is anything true and factual? Or are we all just deluded and mad as hatters? This is a serious question.
What I recall and what was written down in my chart about a certain four days in July 2012 are so different it is difficult to figure out whether my experience was fact in any sense of the word or, as “they”claimed, simply paranoid and delusional. Of course there is some truth in paranoia and delusion, since even a paranoid’s beliefs are based in feelings that arise honestly and from a foundation, I firmly believe, in true things sensed but unacknowledged. Feelings always have their own veracity. But whatever the philosophers may say about the fiction of facts, still there is, there must be, something more to the consensual world of what happens than mere perception.
I mean, either that security guard in the Emergency Department last July deliberately attempted to strangle me, or he did not. Either it happened or in some fashion I imagined it. It is that simple, isn’t it? Yes or no, red or green, one or zero. Like a digital configuration, there’s nothing vague about it: either it happened or it didn’t.
There are records. I know what the ones they wrote say, as far as they go. But how to interpret them since so little was written down, and unless my memory is so completely at odds with reality as to have confabulated the entire episode – which by the way, is what they claimed all along – how to explain the discrepancies when so much is not even mentioned. That they whisked my gurney into a seclusion room and assaulted me en masse is my version. In theirs, the room change is noted only in passing, and of the IM medication all that is said is that it was given “NOW”. Nothing else of the incident I recorded in great detail in my journal some days later, and raged about from the first day I was admitted to the day I left. In fact, I’m still outraged, months later.
I wanted to go home, they wanted me to stay. That I was abjectly terrified of being kept there meant to them that I was “paranoid.” I claimed I had no problems and had never been diagnosed with a psychiatric disorder. That was a problem for they had more power than I did as well as my lengthy psychiatric history on their side to prove I must be crazy to make such a claim. Worse, I was loud, demanding, and in my increasing panic, getting angry. They saw my screaming as a threat. Even though I was blind to what was going on, any onlooker could have seen that I could not win and in the end of course I lost mightily.
But let me go back towards the beginning.
It didn’t help that I had arrived at the ED by ambulance and immediately refused to have my “vitals” taken, asserting that I was “fine!” I then accused the nurse of just wanting to get paid for taking them. In short order I was whisked to the so-called “purple pod” where the psych patients were buried for hours until the on-call psychiatrist deigned to come down to see them.
“Here,” someone said, thrusting a hospital johnnie and a pair of pajama pants at me. “Undress and put these on.”
I looked down and saw that I was already wearing pj pants from another hospital. No one ever knew the real nature of what I wore — they simply passed for scrubs — and they were so comfortable that I kept them on day and night. “I’m already wearing pajama pants. I only need to change my shirt,” I said.
“No, you are wearing very nice blue slacks. Now, put on the pajamas, or do you want a couple of strong men to put them on for you?”
“Actually,” I sniped, “they are hospital pajama pants. I pilfered them from –“ and I named the hospital. But I made a show of undoing the snaps so they would see that I was going to comply. The last thing I wanted was anyone touching me or “helping” me undress.
Soon an APRN, came by and I thought, Wow, they are quick here, maybe it isn’t so bad being taken to a big hospital. Maybe I can get discharged from here in no time. Unfortunately, she was there only to do a 15 second “physical exam” that consisted of looking in my mouth and listening to my back with her stethoscope. Period. Pronouncing me cleared for a psychiatric interview, she rushed off to clear someone else. Then I sat on the gurney in my cubicle and waited. And waited.
I remember being cooperative for what felt like a long time. I tried to sleep, and I listened patiently to what was going on around me. I swore that I would simply hold my breath and bide my time until someone saw me, so that, calm, I could present my case and they would see I was safe and sane enough to be sent back home, not admitted or sent to some hospital against my will. But it was taking so long, it was taking hours for someone to see me, and I knew they were doing it to me on purpose. Did they think I, too, was drunk or on drugs just like the others here? I started to complain that I had waited long enough and needed to see someone. I was NOT drunk, did not need to dry out. Where was the doctor? There was nothing wrong with me, I did not need to be here. I wanted to go home!
Things started happening then. Memory fails me however and even the chart, which I just obtained a couple of days ago leaves out way too much. All it says is that I was uncooperative, then irritable, screaming and combative. Meds were “offered”.
I remember this: When I refused to take soul-deadening Haldol by mouth, they descended on me, wheeled my gurney into a solitary room and jumped on me, intending to inject me by brute force. In the struggle, a guard gripped my neck and compressed the arteries, strangling me. I tried to get the nurse’s attention, burbling through forcibly compressed lips that I could not breathe. But her response, attending only to her needles and not even looking at me, was an impatient, “You’re all right!” In a pulse of panic, I jerked away as she started to shove the first needle into my arm.
“Damn!” she cried as a rush of blood spattered us and the needle danced away from my skin. “Hold still!”
I’d hoped to get some respite from strangulation but instead of letting go of me, the guard reasserted his grip on my neck and pressed down harder. I felt the light go black as blood failed to reach my brain. Darkness descended. Sounds grew confused and dim. Suddenly I knew that I could die, that this was how patients had been “accidentally” killed during notorious restraint episodes in Connecticut. I did the only thing I could: I went limp, hoping the nurse would get the injections over with quickly and that the guard would not kill me before she was through.
One, two, and then, astonishingly a third needle punctured my arm. She wiped my deltoid muscle with an alcohol wipe then removed herself from the gurney. “All done,” she said, removing her gloves with a smack and she nodded, indicating the door.
With a cruel leisure, the guard let go of my neck, but he leaned down as he did so and muttered in my right ear: “That’ll teach you a lesson about bringing a JCAHO case against M— Hospital…” Then he and all the others strode out of the room, leaving me alone in what I had already been warned was a soundproof room where you can “scream all you want, but no one will hear you.”
In other circumstances, I would have screamed, soundproof or not, as the door was left open. But nothing was ordinary anymore. A guard – thuggish bully, no doubt a reject from the police academy — paid to protect people, had just partially strangled me in revenge for – what? What had I done to him? My case against that other hospital should have meant nothing to him. But what was clear to me, trying to get a breath and calm myself, was that I was not only not protected in the this ED, I was in mortal danger. I could not scream or rage in outrage, I could not even complain or demand to see a patient advocate. My life was imperiled. Still panting, trembling, in shock, I lay in the semi-dark of that single room and prayed — not to any god, mind you, but simply for my life, prayed to get out of that ED alive. I promised myself that I would not say or do anything “wrong,” would comply with everything they asked from then on in order to survive the night. But it was a long night ahead of me and I had no idea whether or not the guard would come back and finish the job. I was so terrified my teeth chattered. I felt a hollow coldness inside me of unutterable fear. And there was nothing I could do but lie there and hope he did not return.
__________________________________
I did not name the hospitals in the piece above, though I usually do, and I refrained from doing so because I do not know whether what I am going to write now is indeed true or not. But if it is not, then I do not want certain people being alerted to this blog post and reading it and taunting me with “Yehaw, we got away with it!” Read on, and you will see what I am talking about further on.
So as I said, I am in possession of my chart, the entire thing, 60 pp for a mere four day stay in the hospital about which I speak, including an approximately 10 hour stay in the ED. In it, there is absolutely no evidence that anyone ever took me or what I had to say seriously at any time. Everything I said was dismissed as paranoid and delusional, grandiose, disorganized or confabulating. (BTW Confabulate does not mean lying, it means to unintentionally “fabricate imaginary experiences as compensation for loss of memory.” But whatever they thought I was confabulating I have not the faintest idea. Or memory. Alas, the chart says nothing of what I spoke about.)
What has completely upset the applecart is my own statement, written in my journal and elsewhere: “Why on earth would that guard care whether or not JCAHO was involved in that other hospital?” On that thought rests everything, because of course, he had to have cared mightily to have wanted to strangle me for it. Or did he? Did he care, and in fact did he try to strangle me, and did he even say those words in my ear? I am serious.
You have to understand something: Once, years ago, I heard, or hallucinated, hospital nurses announce over the public address system in nearly the same words how they were going to “teach me a lesson” about — whatever it was I had done…and I knew I had heard it, knew I was hearing it at the time, except for the fact that I was on the phone with my sister at that time. I held out the phone in the air so she could hear it too, but she told me she heard nothing, assured me that I was hallucinating. What I described was not only unlikely but so beyond the realm of the likely that she was certain it could never have happened. “Its just your voices, Pammy,” she said, “you have to trust me, you are hallucinating.”
So remembering this, it gives me pause. For why would that guard care about JCAHO and that other hospital in the first or even the last place? What could it possibly mean to him? Security guards are usually hired from outside agencies so his over-involved concern with another hospital’s accreditation suddenly seems to me absurd. And if he did not care, why would he have tried to strangle me? Oh, maybe he did hold me down too hard, and I felt that, yes. But if I could speak, then I know I could breathe, so I was not actually being strangled either.
Perhaps I was simply frightened? And could it be that in fact he never said anything at all? That I “imagined” those words, hallucinated them, and then continued to believe that I heard him say them and that he wanted to kill me, all the time since then? Could it possibly be that some of what the hospital personnel said was true — NOT all of it, but some part of it. That I was in fact hallucinating and delusional? It doesn’t make their behavior right. It doesn’t justify throwing me into seclusion and injecting me with IM meds when I was not a danger to myself or others. It doesn’t even make admitting me to the hospital the proper thing to do in the first place. But, but, but…if I have heard people say things, visible people say things that they simply have not said, when they have not said anything at all, and I know this has been the case, then it is, I admit, just possible that what happened at the ED this summer might be another instance of the same…It pains me to think this. It frightens me to think that I could have been so mistaken for so long.
But what’s more, I worry that I am wrong to believe I might be wrong! That the guard DID say what I think he said, did intend to strangle me, and that I am giving him what he wanted: I am letting him drive me into believing I was/am crazy!
I do not know what to think. And I may never know for certain what happened. Not about this. However, one fact that I can corroborate in the record I am painfully aware I “knew” for months: I was given 3 IM drugs during that episode. Yet you only have to read my chart to see that I was given only 2: Geodon and Ativan. The third drug, Haldol, was canceled immediately after it was ordered. The records clearly state that only the Geodon and Ativan were ever administered. This is so striking an error of memory that it too makes me think again about trusting what I was certain I heard in that terrifying room where they held me down and injected me.
I don’t know what to do with this…I don’t know how to handle it or deal with it. It doesn’t feel good, or give me any sense of relief. I dunno how I feel. Just shocked, I guess. And perturbed, because I don’t know what else I have experienced that never “really” happened.
*Note that when I write of a psychiatric crisis, I mean a patient who is not actively on street drugs. I cannot speak to any situation where someone has been taking unknown quantities of unknown chemicals. In such a situation I have absolutely no experience.
That said, I would like to tell you a few simple things about dealing with an unarmed, undrugged person who seems agitated and paranoid. It is true that I speak of myself, but I believe that the only difference between me and a two hundred fifty pound man, is only size and the fear factor. I think that there is no reason on earth why he would not respond to the following interactions just as well as I know I would.
First all of, remember that the person you are dealing with is indeed agitated, and is if paranoid by definition terrified. Keep that uppermost in your mind, because everything you do will be evaluated by her in terms of what threat it poses. If you frighten her or threaten her, she will become much more unpredictable, and the probability of violence increases enormously.
Never approach such a person with a show of force.Not even if she is being “loud” and disruptive. You gain nothing by such brute force methods, and you lose a great deal…Ganging up on a patient who is paranoid only puts her in the “fight” mode. After all, she is already frightened and you have cut off her only perceived avenue of “flight.” Why escalate a crisis situation, making it worse, upping the potential for a violent response. If the situation has already devolved into accusations, yelling and swearing — all three signs of increasing anger and desperation — that is a signal that whatever you are doing is making the paranoia worse; at such a time the best thing to do is NOT to worsen the situation by pushing back, responding with equal anger, and making demands and ultimatums. No, instead back off and WAIT. The person most likely has not had access to a weapon or anything to hurt herself or others, so patience is a virtue and can be put to good use here.
Usually a patient who is paranoid will not do anything of her own accord but try to escape the situation. But if you force the issue, if you prevent her from escaping to a comforting place or from her own feelings of fear by permitting her what she needs to calm herself, or worse, attempt to do something to her that she could perceive as an attack – for instance, if you try to force medication, or grab her or simply threaten her with a group of staff or guards approaching en masse, you may very well provoke her to respond as anyone would when attacked, i.e. with self defensive maneuvers.
Why be surprised, when several people try to rush her and grab her to hold her down for IM medication, or simply gang up on her in some misguided attempt “to calm her down,” if she then responds with apparent aggression? After all, it is several of you against the one of her and it is surely understandable that she feels threatened. Her life feels in danger and in such a situation all bets are off as to what she thinks she must do to preserve her safety.
If you really want the situation to end well, refrain from threatening or attacking her, no matter how impatient you may feel. Instead, choose one calm, unthreatened and unthreatening person, preferably of the same sex or somehow compatible with the paranoid patient’s personality, and have that person approach to a safe distance (safe for the paranoid patient, not just “safe” for the staff person or for lack of a better term, “negotiator.” The negotiator is safe so long as he or she does not threaten or attack the patient, who is much more frightened than the negotiator.
Approach to a safe distance and possibly sit down, calmly and in a relaxed position, so that she understands that you are not scared of her but also not angry or threatening. If necessary, you might indicate that the patient is speaking too loudly for you to hear her, or too rapidly, but that you are there to listen and talk, when she can lower her voice or slow down. Do not speak loudly or angrily yourself. Talk about anything at first. Don’t talk about the patient or what is going on and do not argue or demand. order or talk about your expectations of or for her. Try to talk about calming external things. Does she like nature, art, sports, reading? Is she cold? Hungry? Can she take some deep breaths? Maybe she would like to sit down now, too? Finally, when she can, would she like to tell you what is going on? There is plenty of time, no hurry. It is important to find out what the problem is…
It may be you fear that she will attempt to self-harm or hurt someone impulsively. If the latter, keep everyone a safe distance away. And emphasize the possibility of violence so that they will stay away until the all-clear. Then talk to the person in a soft voice and gently remind her that you know she doesn’t want to hurt anyone, not even herself, that she is already in enough pain…What does she need, right at this very moment, to help her feel better? Then negotiate a way to get it for her, or something that will do as a substitute or an approximation.
It isn’t that hard to negotiate a calm solution to this sort of crisis, without violence or retribution, when you don’t threaten the person and are truly on her side. But you must never lie to her or to swoop down upon her immediately afterwards to put her in restraints. The point is to bring the crisis to a peaceful resolution. It is not a contest you must somehow win, and then punish her because you were scared and got angry. Exacting retribution is unconscionable and if that is your impulse you need to have a talk with your supervisor. Negotiators and other employees who do such things need to be reassigned to other areas or other jobs. They do not belong in crisis intervention settings.
Now I am certain that you can think of other scenarios where four point restraints are absolutely essential. If so, I would like to have you describe one. We can discuss this because I am becoming more and more convinced that Seclusion and Restraints CAUSE more mental illness and suffering than they relieve. How would you feel if you found out that by putting a patient in four point restraints even once, you may have caused enough trauma to induce more self-injurious behavior, plus PTSD? I believe this happens. I also believe that it is terribly dangerous for the sense of self and the self–esteem and the relationship between the patient and ANY health care provider of any sort at all. I see nothing good to come from restraints. NOTHING. I do not even see them as providing safety, not in the long run and scarcely in the short run since those who are restrained tend to become more violent not less. Why will people not learn that the “catch more flies with honey than vinegar” works with people in every instance?
But talk to me. Let me know what you think. A confession: I once wrote an Op-Ed for the biggest state paper around her that suggested that restraints could be an okay form of treatment if patients were taught to ask for them voluntarily! (I cring just thinking how I toed my sister’s “party line” about the helpfulness of restraints. She learned that sort of thinking from being the attending psychiatrist at Y__ Psychiatric Institute where they taught patients to ask for wet packs or to have their wrists chained to their belts all day long… The difference between us is that she still believes in that sort of brutality.)
(Before I write this blog entry, I want to send this message:To certain people from Middlesex Hospital who read this and are following developments in my case against you please be aware that I know who you are and I am watching you. You do not and will not get away with what you did nor with what you are doing now.)
That said, let me tell all the others of you out there what happened at the mediation- meeting-that- wasn’t, this morning at Middlesex Hospital.
As you know, I have been wanting this meeting for a long time, but when I got there not only did I discover that they were playing the game of “Oh, I had no idea that you wanted a mediation meeting, I didn’t know what this meeting was about at all…” but that the CEO had actually cancelled on last Friday the people that he had arranged to meet with me. So in fact the only people who came were administrators, not anyone who had treated or dealt with me on the unit itself, except the doctor who saw me for the last 11 days of my 6 week stay. He may have been the director of the unit, but he was hardly the main doctor I saw, despite what he claimed.
Anyhow, the meeting was extremely — well, first of all, it was largely a waste of time, because NOTHING was said of interest to me. Except that Dr Grillo, the unit director, after I read what follows, actually had the gall to claim that restraints were entirely appropriate…He said nothing whatsoever about what they did to me. OTOH, I can understand why. After all, he had already been told that we were writing the Department of Justice and the Joint Commission regarding his unit, so he must have felt supremely threatened. Naturally he could not have admitted wrong- doing. Not that any god, excuse me, doctor that I have ever met has ever admitted doing anything wrong or ever apologized. God forbid, a doctor apologize! No, that would be too hard and too demeaning for them to ever do. Better that they go along and permit torture and abuse than that they admit that there was wrong done to a patient on their watch, much less that they personally even made so small a thing as a leetle eensy meestake…
Well, I know what they did to me and I know it was abusive and wrong, and so far, except for Dr Grillo and that lot, NO ONE I have ever met outside of Middlesex Hospital has ever ever agreed with him and said, Yes, in fact the use of restraints was proper and necessary, and they were right to do what they did to you.
So take that, you watchers from MH. I hope you tremble in your boots for torturing me so. Because you never apologized, and wouldn’t’ meet with me to talk about it, it serves you right whatever happens now. I came down there today , and it took all the courage I could summon up to do so. I came down there, after two nights without sleep, just to meet with you and talk about what happened on April 28, 2012. But you couldn’t be bothered to deal with me, and so now you will deal with the DOJ and JCAHO. And too bad for you if that means that heads roll and some of you lose your gd jobs. I do not care any more. I tried, I tried to reconcile and talk with you about it, but you didn’t have the courage to do so, you wouldn’t deal with me, and so now you can deal with the powerful ones, and not me. Now I don’t give a damn what happens to you.
Meanwhile, this is what I was going to read to all of you, and what I did read to the hospital CEO and the administrative personnel, and what the advocates are sending along with the letter to the DOJ and JCAHO.
Although I have a longer statement, I first want to read you a poem that I wrote about my experience here. It is only half a page long, but like any decent poem, it says a great deal in few words. The expression “Long pig” means a human being intended for eating.
I came to you fractured,
splintered to syllables,
all-fired to incinerate
the house of my body
where the devil lived.
But I was not nice,
not nice, not nice, no,
I was not nice enough
for balm and kindness,
or to win back my art
or my writing supplies,
so I upended a trashcan
on top of my head
and uniforms nailed
me, naked X, to a bed.
It gouged my brain.
Freight train. Tank.
Two years: still blank.
Nurses, doctors,
thieves: you knew, you
knew. You made of me
pulled pork, long pig
X-posed and pinioned,
not quite a specimen
for your knew the subject
and your objective :
your satisfaction showed
as you struggled to hide
your smiles.
I was admitted to North-7 in extremis: confused, psychotic, and traumatized. Exquisitely vulnerable, my sole comforts were doing art and writing. These were also my strengths. Yet instead of using these to help me, you consistently employed them against me–withholding supplies as punishment when you felt I was not behaving nicely and worse, using loss of them as a stick when they were most needed. The first time this happened was on April 9th, nine days after I had been admitted. I had been using glue sticks freely to make a large collage for several days. Angry at me for yelling at her, one of the senior nurses whom I won’t name, decided to withhold them. She would no longer give them to me until, as she put it, “the team puts them on your treatment plan.” This frankly felt like such gratuitous punishment, and so unnecessary, not to mention counterproductive, that I could see nothing in it but petty revenge. Nevertheless, not myself and not in control, I screamed, “Fuck you!” and ran to my room. Luckily, Christobelle from OT, the one person who consistently treated me not only with understanding and kindness but with respect and dignity as well, came in shortly thereafter carrying two gluesticks. I do not know whether she knew of these new restrictions or not, but I was grateful.
On another later occasion, I had been using my soft felt-tipped markers, which my old treatment plan permitted me until 10pm. That treatment plan had been changed, however, and the new, more relaxed one said nothing about markers, so it seemed to me that I was now allowed markers in my room just like anyone else. However, around 10pm, someone called Bob came in demanding them. He threatened that if he had to ask, quote, “a 3rd time you’re in for trouble.” My pulse ratcheted upward. Uh, oh, uh oh. Why was he doing this? Was he deliberately baiting me, trying to pick a fight? He could so easily have discussed my understanding of the new plan. It wouldn’t have been so hard to figure out a compromise. After all, they were just Crayolas, not carbon steel knives. I was sick of the power plays, and sick of the way staff just wanted to control me instead of talk to me and of how they insisted on domination at all costs. Well, this time I was not going to give up without a fight, and it seemed that a fight was what Bob was itching for. Instead of negotiation and attempting to find a compromise, Bob reached out to grab me, which I construed as an assault. I screeched, “Don’t touch me!” Someone else grabbed me from behind. I kicked and punched. Someone told me later it was Ruth I kicked. In my journal I wrote this: “she was furious enough to lie and scream that I caused an uproar ‘every single night and I’m sick to death of it!’…”
I fought them then, clawing and screaming, trying in vain to resist, my body flailing as the chart itself notes, my heart hammering. Why were they doing this to me over a few markers?! I wanted to scream. Why were they being such bullies? They were hurting me! But of course there were several of them against the one of me and they were much stronger than I at 102 pounds so naturally they overpowered me. They literally dragged me to the so-called time-out room and dumped me on the floor, ordering me to calm down. Then they closed the door. No they didn’t lock it, but they kept me from leaving by leaning against the door.
You know, I don’t know why you bothered calling it a time-out room. No one could use it at will. And when you put me there, I didn’t ask to go – I was forcibly dragged there — and I didn’t want to stay: you kept me there by force so it was the same thing as seclusion, literally and legally. Time-outs have to be voluntary, you have to be able to come and go if and when you want to. When it is forced, it is by definition a seclusion. Period. That cold barren room was not a time-out room. Who did you think you were you kidding?
And listen, did it never occur to you that it was always your treatment of me that generated my behavior, yes, the negative behaviors as well as when I was in control? You could have found out what was going on by talking with me. Instead, you decided to dismiss everything I said and did as manipulative and acting out so you didn’t need to listen to me. Perhaps you thought this disregard was kept secret from me, but I knew it at the time and it caused me enormous anguish. All I wanted was to be treated like a human being. All I wanted was to talk to someone and be listened to. But all you did was make assumptions. You never checked them out with me to find out if they were true and they almost never were. Assume makes an ass out of U and me…But mostly it does terrible damage when the assumptions are wrong. I was so afraid, I was so terribly afraid, but you never knew the half of it. All you did was to dehumanize me, ignore my pain and order me to shut up and be quiet. I know I was difficult for you to quote unquote “handle.” Hell, I was difficult for ME to handle. But I do not have a personality disorder. Ask anyone who knows me. Ask my family. Ask the psychiatrist who saw me from 2000 until 2009, ask the psychiatrist I see now. But you decided that you could detect borderline traits (somehow transmogrified into the full-blown disorder upon discharge…) despite the presence of an active psychosis. By decreeing that I had such a disorder, you put me in an utterly untenable position, because then you had a justification, so you thought, for taking nothing I said at face value. To me it felt like nothing less than soul murder and I will tell you that this particular form of soul murder makes a person want to die. It makes a person want to bash their brains out in public just to get someone to acknowledge them and take them seriously.
April 28.. April 28, 2010. You wrote in my chart your interpretations of my behavior that day and of what happened. Yes, your nursing and physician notes were supposed to be objective but dispassionate as they may have attempted to sound, all observation is but interpretation. I repeat: All observation is interpretation. Now I want you to know what happened from my point of view. (I know that some of you have been snooping around, reading my blog just as you did during my hospital stay, but you will have to sit through this anyway…)
At around 7:30pm, so the evening nurse reported in my chart, I “walked into the dayroom” and if one can believe this, without any provocation I “began shoving and turning over chairs. I then, quote, “picked up the patient trash can and put it over my head.” Staff ordered me to what they called the “time-out room.” Nursing notes report that I refused and, I quote, “went to bed instead.” Because I had not followed her direct order, the nurse wrote that “security was called and patient required security to carry her to time-out room as she refused to move or walk.” No, I simply lay on my bed, mute, trembling with terror when the phalanx of guards roared in.
Despite my lack of resistance, the guards physically took hold of me – unconcerned apparently with my known history of rape and of recent trauma — and took me from my bed where I was calming myself in the least restrictive environment. They physically carried me to the seclusion room and together with staff they forcibly prevented me from leaving.
This is what I wrote in my journal: “It was (freezing in that room) and they wouldn’t give me a blanket so I didn’t stay long…This only led to more goons pushing me back… this time strong-arming me and forcing me to a seated position on the mattress before quickly leaving but not locking the door.”
The nurse wrote this: “Patient refused to stay in time-out room… Patient attempted to shove staff, kicked at staff to get out of room. Patient was instructed several times to sit on mattress and stop pushing at and kicking staff. Patient refused. Seclusion door locked at 7:55pm.”
At this point both records state that I stripped off all my clothing. But the official records record only that fact, and that I then “was changed into hospital garb” and that I immediately stripped these off too. In my journal I wrote something else in addition that is rather revealing: Left alone in that room, I decided, and I quote, “they’d have to give me a blanket if I was [naked] so I quickly undressed and just hid under the mattress for warmth. This caused a stir for some reason and I was forced to put on hospital pj’s and lie down on the mattress. This would not do, not without a blanket which they continued to refuse me.” So once again I took them off and got up and tried to push through the woman barring the [temporarily] unlocked door. She called for reinforcements and they came. In fact, they came en masse.
“At this point” my journal continues, “they again subdued me and told/asked me why I was fighting. I said [it was] because I needed someone to talk to. That was all I wanted, just someone to talk to. One guard seemed taken aback. All these personnel hours wasted when all I wanted was a half hour of one person’s time? It seemed to strike him as ludicrous as it did me….
“Why don’t you just ask to use this room when you feel anxious or upset?” he then asked me.
“I do, I have!” I replied
“Well?
“They always say it has to be reserved for an emergency.”
He seemed completely flummoxed by that reasoning but there was no arguing with Policy so he fell quiet. Finally they decided to leave, telling me to be quiet and lie down.
I did. I did. But I was cold and I begged for a blanket.
“Sorry, it is too dangerous. You will have to sleep without one.””
Why was it so dangerous when I was on one to one and had an observer at all times? It made no sense. And why wouldn’t they just give me a sweatshirt and socks then? Or turn up the heat. How did they expect me to sleep, I was too cold!”
But this last categorical refusal was just too much. No, no blanket, no nothing. Just shut up and freeze. “That was it, I’d had enough! I dashed at them head-first and they parted, only to grab my arms and try to stop me. Someone twisted my right arm and held it behind my back, but I knew how to get him to stop it, so I tried to bite him and he briefly loosened his grip. I twisted my own arm back to me and my left pinky, held, closed tightly onto something, hooked so tightly it wouldn’t budge. My legs, the right one, grabbed the thin leg of a woman behind me, making her lean back off-balance and lose her grip on me. Then I switched to holding both my legs in a death grip around the legs in front of me. It didn’t matter one iota that [I had taken off my clothes again to get a blanket and] was naked…Anyhow, they eventually overpowered me.”
As one guard shoved me onto my stomach on the hard floor, his knee in my back, he muttered in my ear, “You bite me, I’ll teach you a lesson you won’t forget!” Then he mashed my cheek hard against the dirty linoleum till I was breathing dust.
I knew he was capable of hurting me, they all were. I also knew that people can die during prone restraint as the Hartford Courant and others have documented. Adrenalin flooded me, my pulse threatened to rocket out of control but I knew I had to calm down. Very deliberately, I forced myself to lie still, barely breathing.
Fortunately, when I stopped resisting, they released me and let me sit up. Someone gave me a sheet to cover me. The room cleared, except for a tech who was on 1:1 with me. She apparently was now allowed to talk with me, and for this I was supremely grateful. We conversed calmly. The door to the seclusion room had been left open, a big relief.
However, people were still talking in low voices outside the door. I heard someone trot down the hall, heard the open-and-shut of a cabinet door. I asked my 1:1 what was going on. “Don’t worry. They are just getting you some meds or making up a bed for you.”
“A bed?” I said. That gave me a bad feeling…Then I understood what was going on. “Uh, uh. They can’t put me in restraints, I am calm and it is illegal to restrain someone who is not a danger to self or others. You know that.” I repeated it loudly, loud enough so the other staff could hear me. I began to tremble, but forced myself to remain as composed as I could, mustering all the arguments I could against the use of restraints. A nurse entered the room then and asked me to come down the hall. Did I need an escort or could I walk there by myself. “Oh I can walk by myself. But you can’t put me in restraints, I am calm.” I was barely able to speak. I felt dizzy and short of breath but I tried desperately not to show it because I was afraid that if she knew how terrified and upset I was that it would actually give them justification. Nevertheless, I followed her to the empty room — my heart went cold, I could feel urine leak — I felt like “dead man walking” when I saw that in fact they had fastened four-point restraints to the bed.
I entered the room filled with staff members and guards. I told them over and over that I was calm and willing to take PRN meds. I said I knew they were punishing me and that they knew it too. No one contradicted me. The nurse in charge ordered me to lie down on the bed. I protested. She threatened that if I didn’t “they would assist me.” I was terrified of another assault. In fact I was so terrified just of the physiological consequences of fear itself – the flood of adrenalin and painful tachycardia — that I made myself get it over with. I lay down on the bed. Gritting my teeth, I said nothing even when they pushed aside most of the sheet that covered me.
I meant to remain silent. I meant to remain completely still in order to shame them. But when they pulled my wrists right over the edges of the bed, shackling them painfully below the level of the mattress, and spread- eagled my ankles to the corners of the bed, I broke that silence and objected — vociferously. I was appalled at their barbarity but my protests did nothing. I fell silent and let them do what they wanted. Finally satisfied, they trooped out, some of them actually smiling, leaving me alone in the room. I fell asleep quickly, a narcoleptic stress reaction. Nevertheless, no one returned for an hour. They extracted a pledge of obedience from me before taking off the shackles.
“When they released me,” I wrote in my journal, “my back hurt so badly I could barely walk and…my scapula muscles felt as if they had been separated. ‘I plan to sue you for doing this to me.’ I said as calmly as I could as I left the room. Nobody reacted.” As I wrote in my journal the next morning, “I woke in severe pain, the muscles in my chest felt torn from those that connect it to the shoulder… the pain went clear through to the scapula.”
That was not the end of it. Once you treat a human being in such a fashion, all bets are off as to how she behaves from then on. I no longer cared what you did to me after that. When you threatened me with restraints a few days later, I dared you to do it. I egged you on and so you did. My capitulation showed subsequently when I stripped naked multiple times, even voided on the seclusion room floor and smeared urine on the walls. You reduced me to an animal. I hope you were pleased with the results.
From what I witnessed, many of you — on the nursing staff at any rate– took no pleasure in your jobs. You apparently didn’t want to work in psychiatry, and wanted nothing more than peace and quiet and an easy day’s work. When one of you actually screamed at me, after that staff assault occasioned because I didn’t hand in my crayons on time, that you were “sick and tired” of listening to me every night, that was stupid and nonsensical. How can any hospitalized psychiatric patient be expected to worry about what makes a nurse comfortable? By rights it should be the other way around.
I think what it comes down to at the North-7 secure unit is that you expected patients to meet your needs and make you happy and you tried to force us to. In my case, and in at least one other patient’s that I witnessed, you even tried to physically assault us into doing so. But what a farce. Patients in the outer unit warned me to get out of there; they told my friends they were worried staff would hurt me. They were right. By the time I was discharged, I had almost no memory of what had happened over the previous 6 weeks. It is only in the last couple of months that anything has returned to me. Yet every single day since my discharge, when I least expect it, something triggers a thought or bodily memory of my stay here and instantaneously my heart starts hammering, I get dizzy because I can’t breathe, and I tremble and cry just thinking about it because I’m right back in that seclusion room and April 28th is happening all over again…
Now, I don’t expect to recognize any of you. How could I? I still don’t remember much except those episodes I wrote about, and some little snippets here and there. I am told that some of you will be nursing staff on N-7 and some my so-called treatment team. Well, if you were my treatment team and you just turned a blind eye to what went on, for that you are just as guilty as if you accomplished the acts yourselves. Of course, the worst of it mostly took place in the evenings, in relative secrecy and when few were around. But if you knew it was happening nonetheless and If you approved, well, then, I have nothing to say except shame on all of you.
I felt helpless and utterly alone. Frightened beyond belief. No one defended me, no one helped me or came to my rescue. No one except Christobelle Payne. Christobelle treated me with compassion and kindness. She always made sure that I had gluestix and magazines for my artwork, even when your every impulse was to withhold them as punishment. I cannot tell her how grateful I was and how grateful I remain to her for treating me so humanely. I have never forgotten the oasis of kindness she provided in your North-7 desert.
Apparently no one else on the unit understood how to behave humanely or to treat patients with respect, or no one else gave a damn.
Punishment is the nature of what you did to me. You lost your tempers and you punished me. The result was that you permanently damaged and traumatized me. I believe you did what you did absolutely on purpose and I believe you did not care what the consequences would be to me.
Some of you deserve to lose your jobs because of it and because of what I’d venture to guess you have been doing for a long time to other patients. Perhaps you will. You all need to be thoroughly retrained, if that is even possible. Certainly the secure side of the unit needs to be completely reorganized and re-staffed. But that is not my job. You’ll find out what will happen after the Department of Justice and the Joint Commission do their thing.
I hope you remember me and what you did to me for a very long time. Unfortunately, I know I may never be able to forget you. I wish I could, believe me, I wish I could.
The opinions expressed are those of the author. You go get your own opinions.
One minute info blogs escaping the faith trap
Kate Greenough's daily drawings
portraits & figures by an older woman artist, with blue collar roots
Apprenez les langues !
Life is too short to be petty-minded
What sense in chaos.
A pause to admire nature's unparalleled beauty.
Strange Anatomy, Awkward Perspectives
Yeah nah...
Thoughts on all things Autism and mental health
Not your third grade paper mache
Artwork, data analysis, and other projects by Jon
My Life is Art, My Art is Life
“In India when we meet and part we Often say, ‘Namaste’, which means: I honor the place in you where the entire universe resides; I honor the place in you of love, of light, of truth, of peace. I honor the place within you where if you are in that place in you and I am in that place in me, there is only one of us." ~~Ram Dass~~
My adventures in self-publishing and other gibberish
Where Creativity and Imagination Creates Wonderful Ideas for Your Home!
The opinions expressed are those of the author. You go get your own opinions.
One minute info blogs escaping the faith trap
Kate Greenough's daily drawings
portraits & figures by an older woman artist, with blue collar roots
Apprenez les langues !
Life is too short to be petty-minded
What sense in chaos.
A pause to admire nature's unparalleled beauty.
Strange Anatomy, Awkward Perspectives
Yeah nah...
Thoughts on all things Autism and mental health
Not your third grade paper mache
Artwork, data analysis, and other projects by Jon
My Life is Art, My Art is Life