Tag Archives: psychiatry
On my art blog, anti-Psychiatry art
Article about phoebe sparrow wagner’s Emergency Department “care”
This Art print is Available
I cannot find the email or the name of the person who mailed me wanting a print of this piece, but I wanted to inform her that art prints and other posters etc are now available at this link at Redbubble.com. Also posted at Zazzle.com.
ZAZZLE STORE
https://www.zazzle.com/psychiatric_take_down_someones_watching_photo_print-190152500586657512
REDBUBBLE STORE
Trauma, And the Stories We Tell Ourselves

I wrote a version of this in a comment at Linda Lee/lady quixote’s Blog: http://ablogabouthealingfromPTSD.wordpress.com
Hi Linda,
Someone I met here in Brattleboro, really just an acquaintance, maybe 2 or 3years ago said, “get over it!” about the trauma I have experienced, and I found that enormously damaging just in itself. My “guide” Wendy, never tells me such things and she is fully committed to helping people who deal with great traumas. Another thing is that true is that global amnesia, such as I had and still have for a couple of weeks-long hospital stays in their entirety, (and I also have amnesia for other life experiences that were documented as having happened but are lost to my memory,) this sort of global amnesia cannot be self-induced. You either can remember what happened or you cannot.
What I have found very helpful, and this may not be something you can or even choose to do, is this: I find that when my thoughts erupt or are triggered by something in the present, into a spasm of terrible memories, the resulting emotions and anger etc are so paralyzing and painful that I did consciously decide “I’m not going there, not until and unless it is safe for me to do so.” To that end, when I notice my thoughts turning bad, I immediately find anything to distract myself away from that terrible rut that trauma has clear-cut into my cortex.
I know the emotions stem from the thoughts I think, and they constitute the story about them I tell myself. So if I try to tell a different story, like, for instance, “okay, that was my life then, but I am here now and if I am happy now then all of my past including the trauma, has brought me here and I would not be here without it all, yes, even the trauma.” BUT I fully confess that re-telling my story in a more positive way does not work when I am acutely triggered, so that is when distraction plays a huge role.
In some sense, I understand that I cannot remain attached to my story of abuse and victimization, because in a real way this will only lead me down that same trauma path, and even “attract further victimization and trauma”..But to explore these things requires a feeling of safety, which is not usually available, so I get relief from the thinking instead, by distractions and doing things with my mind that I love. Like studying or reading French, or listening to songs, because the verbal aspect of both tend to crowd out the insistent trauma memories.
As Wendy says, it is a practice, like any spiritual practice, to know when your thoughts are headed down an unhelpful path way and to consciously decide not to “indulge” their wish to ruin your day! It does take a lot of practice to do this, and I would be the last to say it is easy. On the other hand, I know there is a safe place for them, for me to experience the memories and even triggers in security, and that is during my sessions with Wendy. She allows these to be as long as necessary for me to get through things, so they are usually 2-2.5 hours every time. But the thing is, knowing I can hold on and let things “in” in a safe place with her allows me to also decide NOT to let them in or to control me at other times.
I hope this makes sense. It might not be your cuppa tea, and I dunno if you have a safe place/person with whom you could both process memories or at least let them out, but who also, by being a safe person, might allow you to go the distraction route. I myself have found it very helpful…and you know (I know you above all know!) how terribly I have been tormented by my memories of trauma.
The idea that even trauma memories are part of the story of our lives that we write or create and can de-create also helps me. Because I can decide, of, say, someone who brutalized me, well, in their story I was only a bit character, and they likely told and tell themselves something entirely different from my story about it. But I understand that these are all stories, all dramas, that are not really Truth…and if we can retell the story In such a way as to increase ours and the worlds happiness, that should be our aim.
More to come about blame and being victimized but I have stuff to do and need to distract myself from the pain that even writing about trauma brings on.
Love to all,
phoebe
Q and A, courtesy of Inkbiotic.com
Check out Inkbiotics WordPress blog for the origin of the questions I respond to below…
1. Would you rather be beautiful, an astronaut or able to walk up any surface (ie up walls and along the ceiling)? Why?
Definitely I would love to be able to walk up any surface — it would provide such a “superpower” and afford me entirely new experiences.
2. Would you rather physically age, mentally age or visibly age?
At 65 I have been told I do not “look my age” to which my response is, this is was 65 looks like! That said, my mental and intellectual aging are of prime concern to me, and along with that is generally the requirement of good physical health. So if I had to choose for one of the three, I suppose I would opt for signs of visible aging.
3. What was the last good deed you did?
I hate to tell people what the good things are that I do in the world, it is boasting and so I keep these between “my concept of god” and me, where any accounting of good deeds belongs.
4. I’ve been watching the Good Place. It’s great. To give a spoiler-free description, it’s a comedy about a Heaven-like place, where you can live in your ideal house in a perfect village, eat all your favourite foods, and hang out with your soul-mate. What three things wwould you choose to have in your good place?
Good friends, good books, good memories.
5. You get a time machine watch that can only go up to an hour into the past or future. What would you use it for?
If such a machine existed, I would reserve its use personally for revisiting all the times that I have written and sent impulsively some email I should not have, or likewise, to repair words I spoke that might have caused immediate harm. I would not use it to visit the future, as that could tamper with the present big time and also I prefer the future to remain tantalizingly unknown and unknowable.
6. You’re such an awesome person, that the mayor of your town has asked you to come up with a national holiday, what would you want the holiday to be for (eg Tree Day, Festival of Dreams), and when would you want it?
Peace Day would be a national holiday of forgiveness where people are supposed to reconcile and make amends for past conflicts , both on the micro or personal scale and on the macro or international level, where this day is reserved for nations to think and act peaceably towards each other, and make attempts to end conflict.
7. What small something would you change right now?
I would start being able to speak again, having been mute since November 2017…
8. What are your plans for getting older? How do you want to spend your time when/if you stop working? Where do you want to be?
Having been on disability and not working all my adult life, retirement is meaningless, but I hope to be able to do art till the day I die.
9. You find out (probably from a magic floating wizard or by text or something) that nothing you do today will have consequences. What’s your itinerary for the day?
First of all, everything we do has consequences, absolutely everything, it is unavoidable, that is the beauty of what is called The Butterfly Effect. Small changes in a system can have enormous down stream consequences, like the butterfly that flaps its wings in Beijing and by a long series of directly traceable consequences and events eventually leads to a hurricane in the Atlantic. We all always affect others and the world in ways we can never perhaps predict or understand the full ramifications of. So given this, I cannot in any rational way answer this question.
10. When you die your ghost will be trapped in the place of your death, where do you want to die?
Sorry, but this question again leaves me bereft of an ability to answer. I do not believe in trapped ghosts. Energy exists, yes, and maybe we can “leave behind” personal energy that imbues a place, but I do not think one’s Life energy could get trapped in any place just because you died there. And frankly I think your “living ghost,” the life energy and intentionality you project and leave in your LIVING wake is far more important than where you die. We are trapped only insofar as we believe in traps. Ghosts or spirits or just human energy, life is where energy matters, as it warms the blood and invigorates the mind and body. I worry less about where I will die, and whether my “ghost” might be trapped, than that while living I am free in mind enough not to feel trapped or in a prison of someone else making. Freedom is a state of mind, an attitude. Where the body or the ghost is scarcely matters when your mind is truly free.
Institute of Living, 2013, Torture and Illegal Confinement Part 2

Continued from previous post:
Here’s what SAMHSA the substance abuse and mental health services administration publication has to say on seclusion and trauma:
“Studies suggest that restraints and seclusion can be harmful and is often re-traumatizing for an individual who has suffered previous trauma…
“Further, there is a common misconception that seclusion and restraint are used only when absolutely necessary as crisis response techniques. In fact, seclusion and restraint are most commonly used to address loud, disruptive, noncompliant behavior and generally originate from a power struggle between consumer and staff. The decision to apply seclusion or restraint techniques is often arbitrary, idiosyncratic, and generally avoidable.
“Moreover, some studies indicate that seclusion and restraint use lead to an increase in the behaviors that staff members are attempting to control or eliminate.
I have been traumatized, and not just by hospitals. I was date-raped three times in my twenties and experienced traumatic domestic abuse. The cover sheet on the PAD made very clear that due to these trauma issues, I could not tolerate being secluded or restrained without severe consequences: regression and serious worsening of symptoms. Unfortunately, as soon as the staff saw fit to use physical methods of coercion and control on me, that is to say, punishment, from the first time a staff member grabbed me, all bets were off as to how I would behave. I certainly ceased improving, and my symptoms went downhill. Did they really think they were being kind and compassionate? Violence begets violence….
I tried to get help even when on the unit, at least I tried when I was free to make calls or leave my seclusion, err, forced-voluntary “time-out” two-week-long stay in the so-called side room” last winter. I do not know how many times I called the patient advocate office, but the sole time anyone made contact was when she came to hand me some paperwork – I believe I was actually in 4 point restraints at the time – some papers I could not read about a forced medication hearing they would be holding. I needed her advocacy, but she never responded to my panicked called. I wanted her help, but she never came by to ask me what I needed. She was less than useful, the fact that I had to go through her, and her refusal to respond contributed to my ongoing panic and desperate feelings of aloneness and depression. No wonder Dr. Banerjee tried to force me into ECT (about which my feelings of horror and revulsion were stated clearly in my PAD).
And where did the ECT discussion come from at all? My PAD states that I would refuse ECT under any and every circumstance. My brother would be my conservator if Banerjee had sought to go down that road, and he would never have made any decision to counter my wishes on that subject. If Banerjee really read my PAD, he would have known that. He told me that “Dr Mucha and I have made the decision to force you to have ECT.” I recorded the conversation in my journal immediately after it happened and Dr. Banerjee presented it as a two-man decision only, one that I had no choice in.
Regarding ECT and my so-called “depression,” Sanjay Banerjee MD had stopped my 75mg of the antidepressant Zoloft during the first or second week I was there. “Do you really need that?” he had asked, “You don’t seem depressed to me.” Obedient, and in any event glad to get off any medication at any time, I nodded my head, assenting to the change. At least, I thought, if things go haywire, it will not be due to self-fulfilling prophecy, a doctor looking for symptoms he expects to find and conveniently finding them. And at least he will know the reason.
A week later, instead of reinstating the Zoloft, Banerjee blamed my sudden “depression” on my refusal to take Lamictal, a drug I had not taken in 6-9 months. Now he was applying to force me to have ECT, something I was terrified of, convinced it caused deliberate brain damage.
It was this threat, and the brutality with which the decision was made, that started the downhill course of my IOL stay.
The very next day, all hell broke loose. When I entered the conference room, I pushed some important notes I needed Dr Banerjay and Laurie to read across the table in front of them. They refused, claiming that I threw the papers at them. Instead, Dr Banerjay proceeded to berate me, and told me how he had consulted with other hospitals and providers and had read my records against my instructions and Advance Directive, thus violating my HIPAA rights. Moreover, he threatened me with a behavioral treatment plan that would not permit me to do art or writing unless I “behaved.” I hit the roof, telling him I would sue the hospital and complain to JCAHO, then summarily left, slamming the door, an act that stemmed from feelings of utter impotence, because I couldn’t actually say in words anything more effective.
It could have ended there. I could have been left alone, to cool down and calm myself. But no, Dr. Banerjee had to write for stat meds again, and even though I was on the phone and trying to find someone to talk to, to calm myself, I had to be physically dragged off the chair I sat on, away from the phone and brought to the floor in a physical struggle (because they had attacked first, i.e. physically grabbed me, I defended myself, instinctually). They could have waited for me to finish the call. They could have waited to see if I calmed myself. I was not hurting anyone. I did not threaten anyone or myself with harm. ALL that I had done, in terms of physical threats was yell at the phone and refuse to take a pill. Furthermore, it was done and over with. I had left that area and gone to my room. I had then come back and now sat on the chair by the phone, speaking to my interlocutor on the other end. There was no need to pick a fight or encourage a struggle. A wait-and-see policy could have successfully guided things to a better resolution not only for the situation at hand but for my entire hospital stay. As a famous poem by Dylan Thomas ends: “After the first death, there is other.” Once the IOL staff decided to use restraints, there was no going back. The first time broke everything. So, they used them again, and again, and each time more freely and without justification but for convenience and punishment.
Some final points:
CMS regulations on use of Restraint and Seclusion
Restraint or seclusion may only be imposed to ensure the immediate physical safety of the patient, a staff member, or others and must be discontinued at the earliest possible time.
At no point in my stay was anyone ever in immediate physical danger except me, from the staff who were assaulting me…They may have claimed that I bit and fought and resisted, but this was always in response to their manhandling me first. Always. In fact, my medical records show they had restraints re-evaluated and approved while I was sleeping. They even discharged me from the hospital directly from restraints and seclusion, on a day when the usual attending physician happened to be out of town.
(ii) Seclusion is the involuntary confinement of a patient alone in a room or area from which the patient is physically prevented from leaving. Seclusion may only be used for the management of violent or self- destructive behavior.
This means that IOL’s definition of seclusion as being “kept alone in a room to which the door is locked” is wrong. I protested that I had been secluded all along, for a good two weeks before they instituted formal seclusion. I was not violent or self-destructive, and certainly not imminently dangerous to self or others…Never was anyone in immediate physical danger.) Yet the IOL allowed staff to abuse me and seclude me because I was loud and made people uncomfortable…I was surely not the first person to be so treated and brutalized. It remains traumatizing to this day, and I know it is still happening to patients at the IOL even now, because no one can stop them if they don’t know it is happening. Due to this sort of brutal treatment, my PTSD escalated. I think about what happened there and I can’t stop trembling. I have nightmares every night that literally keep me from sleeping.
“The highest price of all is the price paid by the people who are restrained: their recovery is stalled by a practice that can disempower them, break their spirit, and reignite a sense of helplessness and hopelessness…” from Recovery Innovations
Worst of all, using restraints doesn’t work to make either the patient calmer and safer or the unit a calmer safer environment to work in for staff. In truth, things only go from bad to worse once you restrain an unruly patient…Violence only begets more violence…Moreover, when I was another hospital, I was told by one of their mental health workers that she had wanted to experience the process of being four-pointed so she could identify with patients. She was told no, because as the aide informed me, hospital administrators feared it would be too traumatizing.
Restraints are traumatizing, let’s face it, in order to restrain me the manifold times I have been brutally restrained, putting up no resistance whatsoever, even the most jaded and brutal should have felt a twinge of conscience and questioned why he or she was doing. Unless they had become so inured to cruelty that they no longer considered it degrading and obscene to spread-eagle a naked woman, shackling her legs to the bed posts, so hardened to sadism that they did not consider tying her wrists to the underside of the bed as torture, only a mild form of discipline, meted out in order to teach her the lesson they had decided to teach her…
I hope you manage to read this letter and look at the supporting materials. You could learn a lot. You have more power than I do in this world, and could change things, if you know they are happening and are wrong. I beg you to think about what I have written to you. The IOL is not an isolated case. Brutality happens in nearly every psychiatric ward and hospital in Connecticut, and I believe this is the reason: As long as seclusion and restraints are permitted in any fashion, brutality and abuse will continue and at rates that are higher than where they are eschewed.
The problem is not that there may remain some exceptional cases who, it is claimed, will need to be restrained, but that someone somewhere will start finding such exceptions and boom, we’ll be right back where we started, with abuse and mistreatment of the most vulnerable. I believe the only way to stop the abuse of seclusion and restraints is to simply stop using them, period. Killing in self-defense is a good defense in law, and every decision to use restraints should be evaluated with similar strict thinking. Say No, we don’t go there, first, and then if done, know that it was a violation of the law and harmed the patient above all else, but under some conditions, this is the lesser evil compared to what might have eventuated without their use.
Now hospital workers are allowed to use restraints and seclusion as legitimate forms of “treatment. But when you permit staff to use violence against even one patient, it imbues their culture with an acceptance of violence as a treatment modality rather than something criminal. Restraints help no one. They are always retaliatory. Always discipline and punishment. Oh, in the short run the unit may seem quieter and easier to manage, but in the subsequent days, when the prisoner in restraints re-enters the community more chaos than ever may ensue.
Please help me. Do something about it today.
New Poem by Pamela Spiro Wagner
FIXING YOU – A REWRITTEN POEM
Recalling my month-long “treatment” at New Britain Hospital a.k.a Hospital of Central Connecticut on Grand Street, in May 2014, under the supervision of Dr. Michael E. Balkunas

Only nine days after that last adders-pit hospital —
You still wear sunshades to protect others from you
though no one out here believes they are in peril.
Nevertheless, the staff there described you
as “assaultive,” dangerous to self and others,
unfit for company or visitors.
Neither accurate nor truthful
they wrote lies for the sake of their convenience.
Now you are a week from making new friends
in far northeastern Vermont,
in a place magically named the Kingdom
and it’s a move your bruised mind
requires, still unable to let go of
the half-nelson grip of hospital guards
bent on eliciting pain, who, when told to strip you
then four-pointed you naked to a mattress,
replaying their favorite rape scene,
yanking each limb apart to expose and humiliate, knowing
that the nurses’ own official policy was hands-off
and would protect their asses.
You want truth, you wish for reconciliation
but how, you wonder, does any Truth or Reconciliation proceed
when so many refuse to acknowledge
that hospital staff broke every rule,
stopping short of murder only
because you submitted nick of time,
your terror strangled in a towel they wound
around your head and face,
before they injected punishment drugs into your buttocks,
then muted the intercom and sealed the door
No one was ever there to bear witness.
That was always the point,
from your father to the hairdresser
and all the hospital staffs in-between.
They’ve made a religion of secrecy
and no one Outside wanted to know
what they didn’t want to know…
Call this, “our family business,”
call it, “a private shampoo,”
call it, “necessary treatment.”
they could always do what they wanted to you.
And when it broke you, as it eventually would,
when your sudden screams split the night,
and no one could explain what drove you
to empty your lungs,
ripping the air to shreds,
they stood aside and declared you
just “one of the family” now,
no better and no different than anyone else,
now that they’d finally fixed you for good.
Final presentation of “GOING SANE”
Julie Mad Blogger Interview Recorded at Link Here…
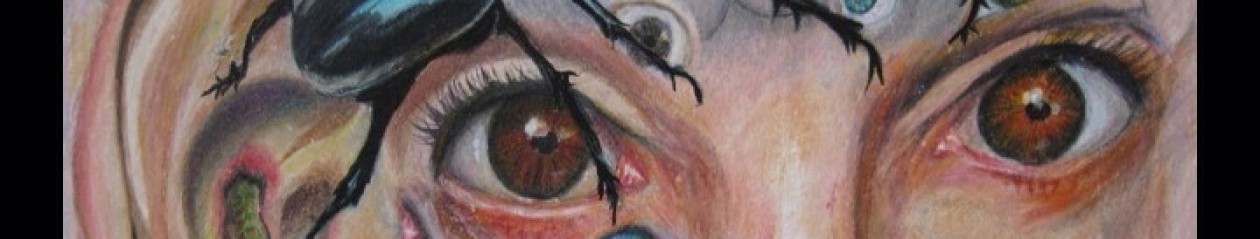
Psychiatrie Macht Frei…(huh?) Art Work
All i can say is everything in this picture was as deliberate as i know how to make it, without planning it at all, and it contains symbolism both public and private. With reference to my signature quotation, (see below) it makes use of what the negative spaces offered me without leaving any in the end.
“There is no negative space, only the shapely void. Hold your hands out, cup the air. To see the emptiness you hold is to know that space loves the world.” P. Wagner
(for those who are not familiar with WWII, over the gates over Auschwitz, the notorious concentration camp where Jews and many other despised groups were taken to be tortured and killed, were emblazoned the words: ARBEIT MACHT FREI, or “work will set you free,” which was of course a lie and a horrible joke, because it was only meant to kill you at what was not a labor camp but just a death camp. )
PSYCHIATRIE MACHT FREI?

Psychiatrie Macht Frei? Mixed media anti-psychiatry picture, 24″by 19″
Paula Caplan is AMAZING: Diagnosis in Psychiatry is BULLshit!

Take a look at this amazing Youtube Video link PLEASE!
Short Story with “Structural Tension” and more!
Dear Readers, here I am again, some scant four months after getting out of the Vermont state hospital unit in Rutland, Vermont, after two years of nearly nonstop institutionalizations, and i am dedicated to the proposition that i will never again see the inside of another mental health facility in this state, or any other state for that matter. Nor will i allow myself to be lied to again by a practitioner of mental health care, a subject i consider almost completely bogus, both the diagnosis of so-called mental disorders and their almost universally dangerous “treatments.”
In this spirit of rejecting the mental health system, rejecting even the non-system, except insofar as I need assistance in getting out of it, and rejecting *any* and all mental illness diagnosis, i decided to take a course in creativity for five days in Newfane, Vermont, just to try my hand at something outside the usual realm of “recovery-” and or madness-oriented activities.
While this ended up being, frankly, a bust — for reasons i will explain, i can report that i really liked the people i met there, some of whom came from as far away as the UK. As for the course itself, I feel that a requirement of valor means that i leave this at “the less said, the better.” I admit, however, that the teacher, a certain Robert Fritz of self-proclaimed international renown, seems to have been taking out his private pique on me ever since the course ended, for leaving the class early, on a few days, and for not praising him lavishly, or even, god knows, “enough.”
So be it, so be it. If he is so small as to exact such petty revenges, i myself need not stoop to his level.
Alas, the course ended up depleting me deeply and the sole worthwhile lesson it left me with concerned “structural tension.” This, Fritz repeated literally ad infinitum, or at least ad nauseam, all day long for five days, 8 hours a day. Sadly, the one time we did worthwhile hands-on practice, when he *first* outlined this notion and gave us a narrative structure — take point A and reverse it to point B (with a character, crisis and certain developing plot points) around which to easily design a monologue — Fritz then gave us an hour to write a piece in the voice of a single person, and was rewarded when every single person in the class wrote what i thought was a professionally competent piece, this was never to be repeated.
How much more he could have taught us and built on that, had he used the example of what we had learned and done and our confidence to “grow on and go on…” but instead he opted only for more of the same old same old, which was just going over the same ground again and again, with analyzing music video after music video but doing it FOR us, not even having us participate in any meaningful way. Readers, it truly appeared that class participation in any real sense was simply too threatening for this teacher, who was not one of those who felt he could learn anything from his students, no matter their age and life experiences…
No more recriminations on my part. I could not have known this would happen, especially since we were provided no clues, no syllabus, no handout that gave any hint as to Robert’s plans…I went in every day, every single day, and to every session with (dimming but) renewed hope that things would change, right to the last session of the last day…To my dismay and disappointment and growing exhaustion, it never did.
At least i enjoyed the monologue- writing exercise. The following was mine, which is fiction, though it was based on someone i know pretty well (and he knows who he is! )
_____________________________________
I, Winton Wooster the third, had sex for 30 years with one man and one man only, Arturo, whom I’d met in Culinary Arts school and absolutely despised. It took me another three years and five other men, one woman, and an Electrolux, before I came to realize that it was Arturo to whom I was attracted and loved with all my heart and soul and body. “Over The Rainbow” sung by Izzy Kamakawiwo’ole was our song.
Some people think gay men can’t be monogamous. That is so not true, so not true. I might have been promiscuous before Arturo, but A.A, that is After Arturo, I never looked away, that is until…well, how do I explain this?
It all started with cars. And collections. Collections of cars. And collections of everything else under the sun. I had the car collection, and I had the other collections. I had Kewpie dolls and Christ statuettes and I had spoons and books of spoonerisms, and I had jackknives and jack-in-the-boxes, I had bowls and bowling ball collections. If there was something to be collected, I collected it and more. I collected art and books, and books of art and china and vintage Chinese clothing and if you think there was no space left in my three-story house, that is saying nothing. I rented space in several other houses, my clients’ houses, which I cleaned each week, and those were soon filled with my collections as well. As for the cars? I had seventeen cars and that was only after culling them down from a high of thirty-seven.
As for Arturo? He had one. One car, and no collections. Only an affection for zinnias, which he called the gay flower and he grew tons of them, for me. His car was named Ada, and she was a 1987 Toyota Tercel. I always said I didn’t think they still made the Tercel that year, but he showed me the papers and proved that they had. Ada was pale yellow, a custom color, and still had the original fabric on her seats and the same original everything, just a tad creaky and fading. I joked with Arturo that we too were creaky and fading. Now, to tell a gay man of 55 that he is beginning to fade and creak is dicey at best, but we were not just old lovers, we were practically brothers, so the degree of his taking offense surprised me. But then he retorted that I shouldn’t talk, since I needed Viagra more often than not and that was only when I managed to get interested enough to take it.
Oooh, that got me where it hurt. But he wasn’t wrong. The thing is, I had once had enormous sex drive along with everything else but along the way, things seem to have just dissipated. I don’t know why exactly. But it was that remark that crystallized an amorphous dissatisfaction into the huge lump of cruel coal it was: Arturo was the source of my problems and my discontent. If I hadn’t been supporting him, if he didn’t live in my house, I would have more space for my things, and furthermore I would find someone I could, frankly, feel something for and well, get it up for. Period.
The end of our partnership came one night during a quarrel about my car collection, which was occupying several other garages as well as parking spaces in town. Several times a year during snow storms we had to play a desperate game of move the cars – in order to stay ahead of the tow trucks and the tickets to get them out of wherever they might be impounded. Arturo was sick of this, and frankly so was I and I wanted, I proposed, and I had actually had the plans secretly approved by the town zoning board, to build a giant garage in the back yard, a “garage-mahal” that would house my entire car collection on site. The problem was that in order to finance it, I wanted Arturo to pay rent, to help out, that is, with my second mortgage.
Arturo was hurt and he said so in no uncertain terms. He had lived with me and paid me in so many other ways, he told me, how could I do this to him? He cooked, he cleaned and he shopped and he did everything in the house to have made it a home for us and now I expected him to pay rent like a mere tenant? Firmly and obdurately I stood my ground and said, yes.
With tears in his eyes, for which I admit I felt a small pang, but not as big a pang as I ought to have, he turned around, climbed the stairs to our bedroom and packed a suitcase. Then I heard him tread the stairs downward, open the front door, and close it with a thud.
I was such a cad I did not even ask him where he was going or see him off. I felt a relief just to be rid of him. I can’t even say why. It was only the next morning that I discovered, in the small car shed I was planning within the week to tear down and replace with my garage-mahal, Arturo’s pale yellow Toyota Tercel, which he had left behind, for reasons I did not know and could not divine. After he didn’t pick it up for a month, I decided that he likely could not afford the payments or the gas, now that I was not paying for everything. Nevertheless, I could not bring myself to get rid of it, so I paid the insurance and made sure the registration was up to date and kept it on the first floor of the new enormous garage that was soon built on the back of my property.
I did not hear from Arturo at all after that. I learned from friends that he was renting a small first floor apartment on the outskirts of town, in exchange for taking care of the owners’ property. He was rumored to have neither phone nor email. I did not try to contact him but got absorbed instead in my own busy-ness.
In the garage-mahal there was room for all of my vehicles, all the ones in driving condition, including the Bentley for which I had paid only $22,000.00 but kept in mint condition. I had some cars on lifts and others were withdrawn down into specially constructed rooms underground. Only my special fire engine red Mustang and Arturo’s Tercel were in the front bay, readily available for driving.
I spent many of my leisure hours polishing and cleaning the cars, as the house had gone to seed, ever since Arturo was not there to pick up after me or sort the collected items. Also, it was – to be honest — lonely. I was able to have sex after Viagra, yes, but then only to have the Electrolux as my partner — what was the point? I gave up sex altogether. But that made me feel even worse. I tried the gay dances and party scene, and once even an “orgy” that a friend urged me to go to. But all of that just made the loneliness worse.
One night in the summer, sitting in a deck chair, under the bright LED lighting in the garage-mahal, I thought I heard someone’s radio playing a yard away. I got up to listen and heard our favorite song, “Over the Rainbow” performed by Izzy. I stole down the street, and listened to the radio on a porch nearby, and found myself standing in a clump of tall bright-petalled flowers as if by coincidence. No coincidence, I thought, there are no coincidences. I am a total cad, but I can’t let this be. I have left the love of my life and I need him back.
I ran back to the garage-mahal and jumped into the red Mustang, but the starter just made a coughing sound, as if it had just then given up the ghost. “Damn!” I yelled, then I realized that Arturo’s Tercel was still insured and ought to be drivable. Ought to be. Hell, yes, why not?
It was. As if it knew just where it was going the Tercel seemed to drive me all by itself to a small pink stucco house on the edge of town, a house surrounded by trees and with planters filled to the brim with zinnias. To this day I don’t know how it was that Arturo happened to be there, or why he did not seem surprised or even taken aback that I’d come. But without questioning anything, he just smiled warmly, opened the door and opened his arms.
Five Point Restraints At Vermont Psychiatric Care Hospital (cont)
After they had me trussed up in restraints…No, let me back up a bit, because it was not that easy…Hannette was the point person, shall we say, the person who had my head between her hands and was cradling it, “oh so gently” as she “oh so soothingly” commanded me to CALM DOWN RIGHT THIS MINUTE!” Again and again, she subjected me to these absurd demnds as if I could possibly do so upon her order. And as if I ever would do anything but attempt to writhe away from her clammy awful grip on my ears that nearly deafened me to her voice even so.
Finally the job was done and they had fastened a thick plate of velcro across my chest so I could not even sit up or do more than bend my neck a bit to see their handiwork, briefly, before i lost strength and had to lie back down. But I was emotionally overwrought with the situation, and what had happened in the space of only minutes.
WTF? How could this have happened when all I ever wanted was an Ativan to calm down and help me speak? And now what?
But they just trooped out, with Annette leaving last, saying, “You will tell us in WORDS when you are safe enough to be released, or you will remain in restraints.” She then departed too.
Although two monitors were posted silently in the adjoining room, I could not see them for my position, nor were they permitted to speak to me, as I knew from prior experience. I let out a scream that echoed through the empty chamber like a banshee howl but it made no difference. Yes, I could hear Chelsea from somewhere, — a sweet female staff member who remembered my Advance directive and the other times I had been restrained — saying, “Pam, take a deep breath, try to stay calm, I am here, you are not alone…” And I mentally thanked her. But as soon as I could remember that she was there, she was taken away, removed by someone who was told not to talk to me….and so it went. A Dr. Lasix came to me within the half hour and told me he wanted me to come out of the restraints as soon as possible but I would have to agree to talk with him. What did I have to say to that?
I could not respond with a shake of my head or a simple nod so I remained silent. He shrugged and left.
Several people attempted to engage me in conversation, but as no one phrased their comments as Yes or NO questions, I had to remain still. I was not unwilling to answer, simply unable to. But time and again they told me I was “unresponsive” or non-compliant, though I was calm and had been rewarded with the requisite assessment to possibly come out of restraints every fifteen minutes. But no one let me, because they would not let me answer their questions without speaking aloud.
The hours passed. First one then two then three. Finally the nurse Jennnifer decided to relent and allow as how I might answer the safety questions with a shake or nod of my head.
“Will you remain safe and not hurt anyone?” she asked me, standing above me.
I nodded my head.
“Will you remain safe and not attempt to harm y0urself?”
I nodded again.
Will you get up go back to the unit to and to your room and continue to behave safely if we let you out of restraints?”
Nod nod nod.
Jennifer seemed happy with my responses but also at a loss as to what to do with them. She paused. “Okay, thank you Pam. I have to go back and confer with Hannette and see if she will agree to take you out of restraints now that you have agreed to be safe.”
She left, turning her back, promising to be back within a few minutes.
Instead, it took a good half hour, and when she did, both she and Hannette arrived with a plan. “We have decided that we want to free up one hand and you will write a safety plan with the free hand. Then we will approve it and if it is adequate we will see about taking you out of restraints.”
I frowned. Even as she spoke, Hannette had moved to the end of the gurney where my stocking feet lay exposed. Her belly squished against my toes and soles of my feet, and I felt an immeidiate disgust and worse. I felt instant revulsion, as if I were being deliberately molested by someone who knew I was helpless to resist. So I kicked at her mightily. If I could have spoken in words I would have yelled something too, like “You effing …something or other…!” but alas, I could say nothing in protest, only scream, and kick. This did have the effect I wanted of getting her to stop and move away. Someone told her to move past me at the head of the bed next time and she did…
But the safety plan writing thing was their way of upping the ante abominably. How dare they? They had already illegally kept me restrained in FIVE points for far longer than necessary, just because they wanted to prove a point and force me to speak. without even offering me Ativan to calm down let alone to promote speech. Now this??? I flat out refused. And so somewhat triumphantly they trooped out, leaving me alone again, still in restraints at 6:00 o’oclock in the morning.
I knew I had to remain as still as possible to earn yet another assessment within the next fifteen minutes. But my muscles and veins hurt becuase I had remainedstill for so many hours, and no one had done any range of motion exercises on me, actively or passively. I was becoming afraid that I would develop a blood clot if I did not move my limbs on my own, and no matter what they interpreted it as, I began a methodical program of movement. I carefully circled each leg ten times in each direction, the restraints clanking as I did do. Then I bent each knee up and down, up and down. Ditto with my arms, until I was satified that I had exercised them at least a minimum and could relax into the required absolute stillness for the next fifteen minutes so I could earn an assessment.
Finally, Jennifer returned a final time. But this time it was only to tell me that they were leaving for the night. “First shift will have to take you out of the restraints. It is too let for is now.”
when end I herd this, I let out a bnshee scream of exhaustion and utter frustration, but it was too no avail. Only when first shift finally came on and found me still in restraints at 7:00 am did they relent and give me Ativan and take me out by 7:30.
Article about Michael E Balkunas,MD !
I moved to Brattleboro Vermont on February 4, 2015, leaving my home state of Connecticut where I’ve lived for nearly 60 years. l had to move because of the horrific psychiatric abuses I experienced in Connecticut hospitals and my fear that if ever I were hospitalized again I would be killed.
I feel guilty, however, just getting out without accomplishing something to stop what continues to happen in Connecticut psychiatric units and hospitals.
The experience of mechanical four-point restraints – leather cuffs that are tightened around the wrists and ankles to immobilize a patient to a bed – or being isolated by force in an often freezing seclusion cell is almost universally terrifying. Nevertheless, both cell and/or restraints are routinely employed to curb loudness and undesirable behaviors at the Hospital of Central Connecticut on Grand Street in New Britain. I know this because I was subjected to both seclusion and restraints multiple times in the spring of 2014, despite a diagnosis of chronic paranoid schizophrenia, as well as PTSD that was triggered by precisely this sort of thing.
Bizarrely, the hospital psychiatrist, Dr Michael E Balkunas, treating me at HOCC challenged my PTSD diagnosis. “Patient misperceives her treatment as traumatic,” he wrote in my chart. Well, maybe so, but I don’t know how I can be accused of misperceiving three entire days callously abandoned alone, tied to the four posts of a metal bedstead at U-Conn’s Dempsey Hospital (for trying to escape the locked unit) as anything but brutality, even if it was in the 1990s. I also think it is nearly by definition traumatic to be forced to defecate in one’s own clothing while tied to a bed which is what they did at Hartford Hospital’s Institute of Living in the winter of 2013. This was after I was told to lie down and place my own limbs in the leather cuffs (“as a consequence but not a punishment”) for walking away from the very same “Side Room” that I had just been assured was “not a seclusion room unless you call it a seclusion room.”
Again, maybe I misperceived being grabbed and held face-down and nearly suffocated numerous times by staff at Yale Psychiatric Hospital in August 2013, who injected 10-20 milligrams of Haldol, a known drug of torture. Maybe this was just kindliness that I misunderstood as traumatic, maybe it was merely a “psychotic misperception” on my part? Maybe, and maybe not.
Nevertheless, the fact remains that in the ED of New Britain’s HOCC, a security guard in May 2014, grabbed me by my left shoulder immediately after he was warned by the nurse that it was my left shoulder that had a rotator cuff tear.
My New Britain chart records that I was admitted to that hospital, and to the IOL and others with a detailed Psychiatric Advance Directive, the first page of which states that seclusion, four-point restraints and forced medication invariably result in regression to “primitive states and severe worsening of symptoms.” It also makes several concrete suggestions how better to deal with me when I am upset. Even though I spent many hours on this document, Psychiatric Advance Directives have no legal clout in Connecticut and doctors can and do ignore them freely.
Perhaps because of this, HOCC staff literally forced me (“escorted me”) to seclusion and/or restrained me again and again. They took to stripping me “for safety’s sake,” and even though I put up no resistance, they had the male guards spread-eagle my limbs while still naked and put restraint cuffs on without even covering me.
Is it any wonder that what resulted was someone who would wash her hair in her own urine, defecate on the floor of her room and smear feces on the wall? Yet Dr Balkunas, the director of W-1, the general psychiatry unit at HOCC claimed that my trauma was imaginary. Why? Because treatment cannot be traumatic. He simply never got the connection between my horrendous decompensation and his so-called “therapy.” Maybe he never appreciated that he was torturing me, like a person who ripped the wings off butterflies as a child. Someone like that would not have understood how those creatures suffer either.
TO MY “PROTECTOR” AT THE MENTAL HOSPITAL: NO THANKS!
Mushroom-Head in Four-point Restraints: Cannibalism as RAPE by Michael Edward Balkunas, MD, the instigator…

TO MY “PROTECTORS” AT THE MENTAL HOSPITAL
You nurses who, wanting a quiet shift, shackled me into four-point restraints: you ought to have known better: violence only begets more violence…
I came to you, broken —
speaking only splinters of syllables –
“ma-ta-o-tam, ma-ta-o-tam..”
on fire to burn down
the house of my body,
for the meaning of my life
but I was not nice,
not nice, not nice, no,
I was not nice and quiet enough
for the balm of art supplies and human kindness.
Your uniforms ex-cruciated me, tying me
me naked to the four corners of a bed
so your eyes could flay me, the silent shame
gouging my brain to a darkness
years later still vacuumed blank.
Nurses, healers, thieves,
racked there, I lay helpless before you,
even as you raped what was left
of my human dignity.
So intent on getting satisfaction,
you violated my soul
with your smirks
and conspiratorial smiles.
Mental Patient Anti-Psychiatry Rap
TRY ON IPHONE OR IPAD OR APPLE …DOES NOT WORK ON INTERNET EXPLORER…Okay, this may not please everyone and it isn’t exactly ready for Primetime, but if you can’t hear the lyrics (and in any rap song it is difficult to catch all of them the first time, you can read them along below…Enjoy?? Or at least you will understand, if you are familiar with Wagblog, where I am coming from. Please let me know if this file does NOT play for any reason.
Mental Patient Rap
by P.Wagg
CHORUS:
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, I ain’t nothing but a nomad
in the white-coats’ lab.
They say fake it till you make it, so I take it, take it, take it,
Careening through a maze of rules that make me wanna break shit.
Sanity won’t save me, nor all the pills they gave me.
Their remedy’s my enemy, so we mad go fucking crazy.
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, I ain’t nothing but a nomad
in the white-coats’ lab
VERSE 1:
I remember being locked in, tied down, drugged up,
nurses in control of me, rushing me, coercing me.
Worse than their forcing me was all the pills they pushed on me
then Thorazine or Stelazine jammed into my ass cheeks.
Abuse was inexcusable. Psychiatric orderlies
cuffed my wrists and ankles to a bed when I refused them.
Bruising me, mis-using me — and black and blues-ing me,
A/C cold as ice; retaliation taken twice.
Tied down, naked, there, I shit myself but who cared?
Just another everyday mental patient nightmare.
CHORUS:
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, I ain’t nothing but a nomad
in the white-coats’ lab
They say fake it till you make it, so I take it, take it, take it,
Careening through a maze of rules that make me wanna break shit.
Sanity won’t save me, nor all the pills they gave me.
Their remedy’s my enemy, we mad go fucking crazy.
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy I ain’t nothing but a nomad
in the white-coats’ lab
VERSE 2:
As bad as leather cuff restraints their isolation cell was hell.
so supermax it made me faint, don’t tell me they meant it well.
No one should have dumped me there, hearing voices, terrified
they stripped my clothing off then left me locked alone inside.
and told me that they had the right to keep me there both day and night
or as long as it would take, for me to learn from their mistakes
I might never get out, never get out, never get out, never get out–
but I started freaking out. I shouted, “I will not bow down
to those with nothing more to do than cause me pain, you cowards, you
you have no heart, you’re inhumane. You torture me to entertain.
CHORUS:
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, I ain’t nothing but a nomad
in the white-coats’ lab.
They say fake it till you make it, so I take it, take it, take it,
Careening through a maze of rules that make me wanna break shit.
Sanity won’t save me, nor all the pills they gave me.
Their remedy’s my enemy, so we mad go fucking crazy.
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, I ain’t nothing but a nomad
in the white-coats’ lab
Verse 3:
Let’s sing ring around the posey-o: “Hospital Guantanamo!”
Isolation, prison SHU, and mental patients just like me who
traumatized and tortured just go c-c-c-crazy, too.
Abuse is S.O.P. from doctors of psychiatry,
Pusher docs who love to dish out electro-shock therapy
and chemical lobotomies, but it’s all about their money.
Crocks of shit! You’re so wack. You psycho-quacks, you pricks
sized us up and tricked us. But didn’t we wise up quick?
We won’t take no more horseshit, we won’t take no more crap
Take your fucking psycho-meds and ram them up your —-!
CHORUS:
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, I ain’t nothing but a nomad
in the white-coats’ lab
They say fake it till you make it, so I take it, take it, take it,
Careening through a maze of rules that make me wanna break shit.
Sanity won’t save me, nor all the pills they gave me.
Their remedy’s my enemy, so we mad go fucking crazy
C-c-c-crazy, l-l-l-lazy, c-c-c-crazy, mad and bad.
C-c-c-crazy, l-l-l-lazy, I ain’t nothing but a nomad
in the white-coats’ lab
Oh, you know, you know, yes I know you know,
that I ain’t nothing, never been nothing, never been nothing…
I’ve never been nothing, except a lonely nomad
in the white-coated doctors of psychiatry lab
Spoken CODA:
PT:“I want outta here.”
RN: “Uh uh, not so fast. We’ve got your ass for fifteen days.”
PT: “Fifteen days?! No way, José. You can’t keep me here. I want a lawyer!”
RN: “Doctor, we need to calm her pronto. She’s disturbing the whole unit.”
MD: “I agree. Give her 20mg, IM Haldol, stat.”
PT: “What do you want? What’s going on?! No no! Don’t touch me…Wait!
He-e-e-elp! Help me! Please somebody! Help! Help me…!”
YOU AND YOUR ANTIDEPRESSANT — From Anne C Woodlen’s Blog
I THOUGHT THIS WAS INCREDIBLY WELL WRITTEN AND IMPORTANT INFORMATION. SEE CREDITS AT THE BOTTOM. Posted on January 12, 2014 by annecwoodlen THINGS YOUR DOCTOR SHOULD TELL YOU ABOUT ANTIDEPRESSANTS September 12, 2012 By Paul W. Andrews, Lyndsey Gott & J. Anderson Thomson, Jr. Antidepressant medication is the most commonly prescribed treatment for people with depression. They are also commonly prescribed for other conditions, including bipolar depression, post-traumatic stress disorder, obsessive-compulsive disorder, chronic pain syndromes, substance abuse and anxiety and eating disorders. According to a 2011 report released by the US Centers for Disease Control and Prevention, about one out of every ten people (11%) over the age of 12 in the US is on antidepressant medications. Between 2005 and 2008, antidepressants were the third most common type of prescription drug taken by people of all ages, and they were the most frequently used medication by people between the ages of 18 and 44. In other words, millions of people are prescribed antidepressants and are affected by them each year. The conventional wisdom is that antidepressant medications are effective and safe. However, the scientific literature shows that the conventional wisdom is flawed. While all prescription medications have side effects, antidepressant medications appear to do more harm than good as treatments for depression. We reviewed this evidence in a recent article published in the journal Frontiers in Psychology (freely available here). The widespread use of antidepressants is a serious public health problem, and it raises a number of ethical and legal issues for prescribers (physicians, nurse practitioners). Here, we summarize some of the most important points that prescribers should ethically tell their patients before they prescribe antidepressant medications. We also discuss the ways that prescribers could be held legally liable for prescribing antidepressants. Finally, we implore practitioners to update the informed consent procedure for antidepressant medication to reflect current research and exercise greater caution in the prescription of antidepressants.
- How antidepressant medication works
Most antidepressants are designed to alter mechanisms regulating serotonin, an evolutionarily ancient biochemical found throughout the brain and the rest of the body. In the brain, serotonin acts as a neurotransmitter—a chemical that controls the firing of neurons (brain cells that regulate how we think, feel, and behave). However, serotonin evolved to regulate many other important processes, including neuronal growth and death, digestion, muscle movement, development, blood clotting, and reproductive function. Antidepressants are most commonly taken orally in pill form. After they enter the bloodstream, they travel throughout the body. Most antidepressants, such as the selective serotonin reuptake inhibitors (SSRIs), are intended to bind to a molecule in the brain called the serotonin transporter that regulates levels of serotonin. When they bind to the transporter, they prevent neurons from reabsorbing serotonin, which causes a buildup of serotonin outside of neurons. In other words, antidepressants alter the balance of serotonin in the brain, increasing the concentration outside of neurons. With long-term antidepressant use, the brain pushes back against these drugs and eventually restores the balance of serotonin outside of the neuron with a number of compensatory changes. It is important to realize that the serotonin transporter is not only found in the brain—it is also found at all the major sites in the body where serotonin is produced and transported, including the gut and blood cells called platelets. Since antidepressants travel throughout the body and bind to the serotonin transporter wherever it is found, they can interfere with the important, diverse processes regulated by serotonin throughout the body. While physicians and their patients are typically only interested in the effects of antidepressants on mood, the harmful effects on other processes in the body (digestion, sexual function, abnormal bleeding, etc.) are perfectly expectable when you consider how these drugs work.
- Antidepressants are only moderately effective during treatment and relapse is common Since the brain pushes back against the effects of antidepressants, the ability of these drugs to reduce depressive symptoms is limited (see our article for a review). While there is some debate over precisely how much antidepressants reduce depressive symptoms in the first six to eight weeks of treatment, the consistent finding is that the effect is quite modest.
Many people who have suffered from depression report a substantial symptom-reducing benefit while taking antidepressants. The problem is that symptoms are also substantially reduced when people are given a placebo—a sugar pill that lacks the chemical properties of antidepressant medications. In fact, most of the improvement that takes place during antidepressant treatment (approximately 80%) also takes place with a placebo. Of course, antidepressants are slightly more effective than placebo in reducing symptoms, but this difference is relatively small, which is what we mean when we say that antidepressants have a “modest” ability to reduce depressive symptoms. The pushback of the brain increases over months of antidepressant treatment, and depressive symptoms commonly return (frequently resulting in full blown relapse). Often this compels practitioners to increase the dose or switch the patient to a more powerful drug. Prescribers fail to appreciate that the return of symptoms often occurs because the brain is pushing back against the effect of antidepressants. 3. The risk of relapse is increased after antidepressant medication has been discontinued Another effect of the brain pushing back against antidepressants is that the pushback can cause a relapse when you stop taking the drug. This pushback effect is analogous to the action of a spring. Imagine a spring with one end attached to a wall. An antidepressant suppresses the symptoms of depression in a way that is similar to compressing the spring with your hand. When you stop taking the drug (like taking your hand off the spring from its compressed position), there is a surge in the symptoms of depression (like the overshoot of the spring before it returns to its resting position). The three month risk of relapse for people who took a placebo is about 21%. But the three month risk of relapse after you stop taking an SSRI is 43%—twice the risk. For stronger antidepressants, the three month risk is even higher.
- Antidepressants have been found to cause neuronal damage and death in rodents, and they can cause involuntary, repetitive movements in humans.
Antidepressants can kill neurons (see our article for a review). Many medical practitioners will be surprised by this fact because it is widely believed in the medical community that antidepressants promote the growth of new neurons. However, this belief is based on flawed evidence—a point that we address in detail in our article. One way antidepressants could kill neurons is by causing structural damage of the sort often found in Parkinson’s disease. This neurological damage might explain why some people taking antidepressant medication can develop Parkinsonian symptoms and tardive dyskinesia, which is characterized by involuntary and repetitive body movements. Many prescribers mistakenly think these syndromes only occur in patients taking antipsychotic medications.
- Antidepressants may increase the risks of breast cancer, but may protect against brain cancers .
Recent research indicates that antidepressants may increase the risk of cancer outside of the brain, such as breast cancer. However, the neuron-killing properties of antidepressants may make them potentially useful as treatments for brain cancers, and current research is testing this possibility.
- Antidepressants may cause cognitive decline.
Since neurons are required for proper brain functioning, the neuron-killing effects of antidepressants can be expected to have negative effects on cognition. In rodents, experiments have found that prolonged antidepressant use impairs the ability to learn a variety of tasks. Similar problems may exist in humans. Numerous studies have found that antidepressants impair driving performance, and they may increase the risk of car accidents. Recent research on older women also indicates that prolonged antidepressant use is associated with a 70% increase in the risk of mild cognitive impairment and an increase in the risk of probable dementia. 7.Antidepressants are associated with impaired gastrointestinal functioning The action of antidepressants results in elevated levels of serotonin in the intestinal lining, which is associated with irritable bowel syndrome. Indeed, antidepressants have been found to cause the same symptoms as irritable bowel syndrome—pain, diarrhea, constipation, indigestion, bloating and headache. In a recent study, 14-23% of people taking antidepressants suffered these side effects. 8. Antidepressants cause sexual dysfunction and have adverse effects on sperm quality. Depression commonly causes problems in sexual functioning. However, many antidepressants make the problem worse, impairing sexual desire, arousal, and orgasm. The most widely studied and commonly prescribed antidepressants—Celexa, Effexor, Paxil, Prozac, and Zoloft—have been found to increase the risk of sexual dysfunction by six times or more. Evidence from case studies suggests that antidepressants may also interfere with attachment and romantic love. Some antidepressants have been found to negatively impact sperm structure, volume, and mobility. 9. Antidepressant use is associated with developmental problems Antidepressant medication is frequently prescribed to pregnant and lactating mothers. Since SSRIs can pass through the placental barrier and maternal milk, they can affect fetal and neonatal development. Generally, if SSRIs are taken during pregnancy, there is an increased risk of preterm delivery and low birth weight. Exposure during the first trimester can increase the risk of congenital defects and developing an autism spectrum disorder, such as Asperger’s Syndrome. Third trimester SSRI exposure is associated with an increased risk of persistent pulmonary hypertension in the newborn (10% mortality rate) and medication withdrawal symptoms such as crying, irritability, and convulsions. Prenatal exposure to SSRIs is also associated with an increased risk of respiratory distress, which is the leading cause of death of premature infants. 11\\10. Antidepressant use is associated with an increased risk of abnormal bleeding and stroke Serotonin is crucial to platelet function and promotes blood clotting, which is important when one has a bleeding injury. Patients taking SSRIs and other antidepressants are more likely to have abnormal bleeding problems (for a review see our article). They are more likely to have a hemorrhagic stroke (caused by a ruptured blood vessel in the brain) and be hospitalized for an upper gastrointestinal bleed. The bleeding risks are likely to increase when SSRIs are taken with other medications that reduce clotting, such as aspirin, ibuprofen, or Coumadin . 11. Antidepressants are associated with an increased risk of death in older people. Depression itself is associated with an increased risk of death in older people—primarily due to cardiovascular problems. However, antidepressants make the problem worse. Five recent studies have shown that antidepressant use is associated with an increased risk of death in older people (50 years and older), over and above the risk associated with depression. Four of the studies were published in reputable medical journals—The British Journal of Psychiatry, Archives of Internal Medicine, Plos One, and the British Medical Journal—by different research groups. The fifth study was presented this year at the American Thoracic Society conference in San Francisco. In these studies, the estimated risk of death was substantial. For instance, in the Women’s Health Initiative study, antidepressant drugs were estimated to cause about five deaths out of a 1000 people over a year’s time. This is the same study that previously identified the dangers of hormonal replacement therapy for postmenopausal women. In the study published in the British Medical Journal, antidepressants were estimated to cause 10 to 44 deaths out of a 1000 people over a year, depending on the type of antidepressant. In comparison, the painkiller Vioxx was taken off the market in the face of evidence that it caused 7 cardiac events out of 1000 people over a year. Since cardiac events are not necessarily fatal, the number of deaths estimated to be caused by antidepressants is arguably of much greater concern. An important caveat is that these studies were not placebo-controlled experiments in which depressed participants were randomly assigned to placebo or antidepressant treatment. For this reason, one potential problem is that perhaps the people who were taking antidepressants were more likely to die because they had more severe depression. However, the paper published in the British Medical Journal was able to rule out that possibility because they controlled for the pre-medication level of depressive symptoms. In other words, even among people who had similar levels of depression without medication, the subsequent use of antidepressant medications was associated with a higher risk of death. These studies were limited to older men and women. But many people start taking antidepressants in adolescence or young adulthood. Moreover, since the risk of a relapse is often increased when one attempts to go off an antidepressant (see point 3 above), people may remain on medication for years or decades. Unfortunately, we have no idea how the cumulative impact of taking antidepressants for such a long time affects the expected lifespan. In principle, long-term antidepressant use could shave off years of life. It is commonly argued that antidepressants are needed to prevent depressed patients from committing suicide. Yet there is a well-known controversy over whether antidepressants promote suicidal behavior. Consequently, it is not possible to reach any firm conclusions about how antidepressants affect the risk of suicidal behavior. However, most deaths attributed to antidepressants are not suicides. In other words, antidepressants appear to increase the risk of death regardless of their effects on suicidal behavior. We suggest that antidepressants increase the risk of death by degrading the overall functioning of the body. This is suggested by the fact that antidepressants have adverse effects on every major process in the body regulated by serotonin. 12. Antidepressants have many negative effects on older people Most of the research on the adverse health effects of antidepressants has been conducted on older patients. Consequently, our conclusions are strongest for this age group. In addition to cognitive decline, stroke and death, antidepressant use in older people is associated with an increased risk of falling and bone fracture. Older people taking SSRIs are also at an increased risk of developing hyponatremia (low sodium in the blood plasma). This condition is characterized by nausea, headache, lethargy, muscle cramps and disorientation. In severe cases, hyponatremia can cause seizures, coma, respiratory arrest and death. The fact that most research has been conducted on older people does not mean that antidepressants do not have harmful effects on the young. As previously discussed, antidepressants can have harmful effects on development. Moreover, many people start taking these drugs when they are young and remain on them for years or decades. In principle, the negative effects of these drugs could be substantial over such long periods of time. Altogether, the evidence leads us to conclude that antidepressants generally do more harm than good as treatments for depression. On the benefit side, the drugs have a limited ability to reduce symptoms. On the cost side, there is a significant and unappreciated list of negative health effects because these drugs affect all the processes regulated by serotonin throughout the body. While the negative effects are unintended by the physician and the patient, they are perfectly expectable once you understand how these drugs work. Taken together, the evidence suggests that these drugs degrade the overall functioning of the body. It is difficult to argue that a drug that increases the risk of death is generally helping people. There may be conditions other than depression where antidepressants are generally beneficial (e.g., as treatments for brain tumors and facilitating recovery after a stroke), but further research in these areas is needed (see our article). Ethical and Legal Issues Physicians and other medical practitioners have an ethical obligation to avoid causing greater harm to their patients. The Latin phrase primum non nocere (“first, do no harm”) that all medical students are taught means that it may be better to do nothing than to risk causing a greater harm to a patient. Although all prescription medications have adverse side effects that can cause harm, practitioners have an ethical obligation to not prescribe medications that do more harm than good. The evidence we have reviewed suggests practitioners should exercise much greater caution in the prescription of antidepressants and to reconsider their use as a first line of treatment for depression. Additionally, we suggest that physicians and other medical practitioners should consider their potential legal liability. Legal liability for prescribing antidepressants Medical practitioners can be sued for prescribing antidepressant medications if doing so violates their state’s standard of care laws. In most states, the standard of care is what a “reasonably prudent” practitioner in the same or similar field would do. The standard of practice is not defined by what the majority of physicians do because it is possible for an entire field to be negligent. Since studies on the health risks associated with antidepressant use (e.g., stroke, death) have been published in well-respected medical journals, medical practitioners could possibly be vulnerable to malpractice lawsuits. For instance, it seems likely that a reasonably prudent physician should be aware of the medical literature and avoid prescribing medications that could increase the risk of stroke and death. Prescribers can also be held liable for not discussing information about medical risks so that patients can give informed consent for medical treatments and procedures. Prescribers have a duty to discuss the benefits and risks of any recommended treatment. Consequently, medical practitioners should discuss with their patients that antidepressant medication is only modestly more effective than placebo and could increase the risk of neurological damage, attentional impairments, gastrointestinal problems, sexual difficulties, abnormal bleeding, cognitive impairment, dementia, stroke, death, and the risk of relapse after discontinuation. Antidepressants must cause harm to create liability A medical malpractice lawsuit can only succeed if the antidepressant caused harm to the patient. It is important to realize that the antidepressant does not need to be the only cause of the harm—it only needs to contribute to or exacerbate the harm. As we have argued, antidepressants play a causal role in many adverse health outcomes because they disrupt serotonin, which regulates so many important processes throughout the body. This may make it particularly difficult for a medical practitioner to defend against a medical malpractice suit from a patient who experiences any of a number of adverse health effects while taking an antidepressant. For instance, if a patient has a stroke while taking an antidepressant, the evidence that antidepressants increase the risk of stroke suggests that the antidepressant may have contributed to the patient’s stroke, even if it was not the only cause. Conclusion The evidence now indicates that antidepressants are less effective and more toxic than commonly believed. From ethical, health, and legal perspectives, it seems prudent for individual practitioners and professional medical organizations to revise informed consent guidelines and reconsider the status of antidepressants in standards of care for many diagnoses and as the front line treatment for depression. With older people, for instance, the current data suggest informed consent must include a discussion of the increased risk of hemorrhagic stroke and even early death. We suspect that if prescribers realized they were placing themselves at legal risk for failing to discuss the adverse health effects of antidepressants with their patients, not only would they be more likely to discuss such information, they would be less likely to recommend these drugs in the first place. Paul W. Andrews is an assistant professor in the Department of Psychology, Neuroscience & Behaviour at McMaster University in Canada. He has a PhD in Biology from the University of New Mexico and a law degree from the University of Illinois at Urbana-Champaign. His work on the evolution of depression with J. Anderson Thomson, Jr. has been featured in the New York Times Sunday Magazine and Scientific American Mind. Taken with respect and gratitude. directly from ANNECWOODLEN’s Blog BEHIND THE LOCKED DOORS OF INPATIENTS PSYCHIATRY. http://behindthelockeddoors.wordpress.com/2014/01/12/you-and-your-antidepressant-2/
YouTube Video: Mental Hospital Treatment and Abuse -Reality in Art
This time you should be able to view this on an Iphone or Ipad.