As Connecticut works to improve its mental health system, new federal data shows that hospitals in the state restrain psychiatric patients at more than double the average national rate, with elderly patients facing restraint at a rate seven times the national average.
In addition, the state lags behind in providing adequate post-discharge continuing care plans for psychiatric patients, especially teens and the elderly. Connecticut’s 28 inpatient psychiatric units and hospitals developed continuing-care plans for fewer than 70 percent of patients they discharged from October 2012 to March 2013 — indicating that thousands of patients may have left facilities without adequate treatment and medication plans.
A C-HIT analysis of the federal data, released by the Centers for Medicare & Medicaid Services for the first time, shows that Connecticut ranks in the top fourth of states (11th highest) in the use of physical restraints in inpatient psychiatric facilities — and is the third highest state in restraining patients 65 and older.
Two psychiatric units — at Bridgeport Hospital and Masonicare Health Center in Wallingford — have the 10th and 12th highest rates of restraint use, respectively, among the 1,753 psychiatric facilities nationwide that are included in the federal reports, which cover October 2012 through March 2013.
State and federal guidelines — tightened over the past 15 years, partly in reaction to deaths in Connecticut facilities — say that restraints should be used only in cases of imminent physical danger to a patient or others. They call for less restrictive interventions when patients are acting out aggressively.
But the data show that Bridgeport Hospital, Masonicare and three other Connecticut hospitals — Waterbury, Hartford, Danbury — restrain patients at more than triple the national rate.
James McGaughey, director of the state Office of Protection and Advocacy for Persons with Disabilities, said he was disturbed by both the high rate of restraint use and the low rate of post-discharge plans.
“The numbers are pretty compelling,” he said. “Some of our hospitals have done a significant amount of work on this, but clearly there’s more to be done.”
He suggested that the Department of Public Health, which oversees hospitals and is charged with reviewing annual reports of restraint and seclusion, should “get a little less timid in looking at this.” Hospitals rarely have been cited or penalized in recent years for improperly using restraints, a review of inspection reports shows.
McGaughey noted that the state-run Connecticut Valley Hospital in Middletown has pursued a reduction in restraints and seclusion that has cut its restraint rate significantly in the last five years. The new data show CVH’s rate at .52 hours per 1,000 patient hours — below the statewide rate of 1 hour per 1,000. The national average is .39.
“It’s ironic that our one remaining large state hospital has done such a good job of reducing restraint and seclusion, but you have some very different results at private institutions,” McGaughey said of CVH, which was cited for excessive restraint use in 2007 by the U.S. Justice Department. “What it shows is that it’s possible to address this issue, but you need leadership to effect this kind of culture change.”
Mental health advocates say seclusion and restraint should be avoided because they are traumatic and dangerous to patients and staff.
Alternatives include individualized aggression-management plans, the use of “comfort rooms” or time-out spaces, and one-on-one interventions. Among the innovations at CVH are 22 “comfort rooms,” designed to calm agitated patients, and a reduction in the time interval that a physician’s order of restraint or seclusion can remain in effect, according to a state report.
Yale-New Haven Hospital has a restraint rate of .36 hours per 1,000 patient hours — just below the national average of .39 hours. But its rate of developing care plans for discharged patients is relatively low — 50.36 percent, compared to a national average of 73.5 percent of cases.
Officials at Connecticut hospitals with high rates of restraint say they are working to reduce those incidents, and they stressed that even minimal mobility restrictions, such as soft wrist restraints or brief therapeutic holds, are counted in the federal numbers.
Robert Bernstein, executive director of the Bazelon Center for Mental Health Law, a national advocacy group that successfully sued Connecticut in 2006 to stop housing psychiatric patients in three nursing homes, said he worried that progress made in the early 2000s to reduce restraints might be slipping in some hospitals because of staff shortages and “pushback” from clinicians.
“Some of the procedures put in place may have been weakened, because it’s a lot of work” to use alternative interventions, he said.
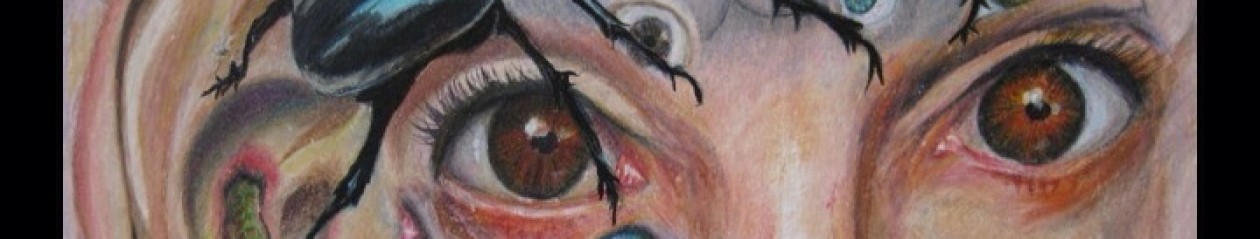
Although patients subjected to improper restraint can file complaints, few speak out, Bernstein and others said. Among the exceptions in Connecticut is Pamela Spiro Wagner, a Wethersfield writer and artist with schizophrenia who has cycled in and out hospitals.
In an April “open letter” to the director of a Connecticut psychiatric hospital, Wagner readily conceded that she is a difficult patient — “easily roused to irritability and hostility” — but insisted that her behavior has not warranted her repeatedly being placed in restraints and seclusion, for hours at a time.
“Once you allow staff to use restraints a little, it only takes a little to use them a lot.”
CONNECTICUT VS. THE NATION
Nationally, the states with the highest restraint use are Minnesota, Washington, South Dakota, Tennessee and New Hampshire. For patients 65 and older, only Nevada and New Hampshire have rates higher than Connecticut, which restrains elderly patients at an average of 7.69 hours per 1,000 hours. Thirty-five states have rates of less than 1 per 1,000 hours; the national average is 1.01 hours per 1,000 hours.
The U.S. facility with the highest restraint rate is Park Ridge Health in North Carolina, which reports 722 hours of restraint use per 1,000 patient hours overall. Among facilities that report serving children ages 2 to 12, Lakeland Regional Medical Center in Florida has the highest restraint use, at 200 hours.
The federal data shows Connecticut psychiatric facilities fare well in some categories, including lower-than-average rates of restraint for children and teenagers. Five hospitals reported no use of restraints for any age group: Sharon, MidState Medical Center, Bristol, John Dempsey and Natchaug hospitals.
And Connecticut’s rate of keeping patients in seclusion is lower than the national average, with half of the state’s psychiatric facilities reporting that they did not use seclusion at all. Nationally, South Dakota, Montana and Washington report the highest use of seclusion, defined as involuntary confinement where a patient is prevented from leaving.
But the state’s over-65 restraint rate is fueled by excessive rates at Masonicare (35.99 hours), Bridgeport Hospital (37.92) and Hartford’s Institute of Living (9.19).
Officials at those hospitals say they have taken steps in the year since the data-reporting period ended to reduce restraint use.
This is the first time that quality measures from psychiatric facilities have been made available by CMS. The federal agency does not penalize facilities for high rates of restraint or inadequate discharge plans. Instead, an agency spokeswoman said, the public reporting is intended to encourage quality improvements and help consumers to make informed decisions.
At Bridgeport Hospital, Dr. Ryan O’Connell, vice president for performance and risk management, said the hospital’s geriatric psychiatric unit serves many patients with dementia and behavioral problems that cannot be managed in other facilities. About 18 months ago, he said, the hospital put in place an “action plan” to reduce restraints, including using “comfort” rooms. Also, in January, a new policy was implemented requiring that the nurse manager be called before any patient is restrained.
“We realized we were going in the wrong direction with restraints” and have since seen a “dramatic drop” in their usage, O’Connell said.
Hartford Hospital’s Institute of Living (IOL), which has a geriatric unit for complex dementia patients, has made similar changes over the past few years, nursing director Ellen Blair said. She said restraints are now rarely used, and only for patient safety. The IOL requires that a physician’s restraint order be reviewed every two hours, rather than every four, which is the standard of care.
“We look at our data every single day” to ensure that restraint and seclusion are being used only as “a last resort,” Blair said.
Masonicare’s acute psychiatric unit serves geriatric patients who frequently are referred because of difficult behaviors and aggression, said spokeswoman Margaret Steeves. When restraints are needed, the hospital uses “the least restrictive restraint, which is typically a seat belt,” she said. Masonicare has an interdisciplinary team reviewing restraint use.
Statewide, the Connecticut Hospital Association has been working with the state Department of Public Health to minimize the use of restraints, said Dr. Mary Cooper, the group’s vice president and chief quality officer. She said the new federal data “indicate that there is more work to be done in this area” and will help to identify best practices.
Nationally, the federal government tightened rules on the use of restraints and seclusion between 2001 and 2007, including time limits on physician orders and strict documentation requirements. The changes were prompted by a series in The Hartford Courant, “Deadly Restraint,” which documented restraint-related deaths in psychiatric facilities nationwide.
In 2007, the U.S. Department of Justice cited the state-run CVH for excessive overuse of unnecessary restraint and seclusion. Since then, policy and training initiatives have significantly reduced restraint episodes — from 26,290 hours in 2000, to 529 hours in 2012 — a state report shows.
State DPH spokesman Bill Gerrish said the agency collects restraint and seclusion reports from hospitals and works to “ensure that care is appropriate.”
LAGS IN DISCHARGE PLANNING
McGaughey and Bernstein said they were especially troubled by the failure of many hospitals to develop continuing care plans for discharged patients, and to transmit those plans to the next level of care.
Statewide, Connecticut facilities developed adequate discharge plans 69.4 percent of the time — lower than the national average of 73.5 percent. For teens, hospitals transmitted care plans only 55 percent of the time — lower than the national average of 74 percent — and for seniors, just 42.7 percent of the time, below the national average of 56 percent.
Discharged patients are supposed to receive care plans containing their diagnoses, reasons for hospitalization, medications and treatment recommendations.
The federal data shows that 10 Connecticut hospitals, including Waterbury Hospital, Masonicare and Yale-New Haven Hospital, properly transmitted care plans to the next provider in less than half of cases.
A few hospitals — St. Mary’s, Bristol, Norwalk, Natchaug Hospital and Southwest Connecticut Mental Health — transmitted care plans more than 90 percent of the time.
McGaughey said that without continuing care plans directing further treatment, many discharged patients may languish in nursing homes, shelters or land back in the hospital.
“The lack of continuity of care, to me, is a huge issue,” he said. “It’s a pretty brutal business — insurance companies want you to medicate and discharge as fast as possible. The question is, what happens after they’re out?”
Bernstein said the lack of attention to continuing care plans was “jaw-dropping.”
“Those numbers should be at 100 percent,” Bernstein said. “It’s shameful.”
Hospitals with low rates of discharge care plans blamed much of that lag on their failure to document that the paperwork was done.
At Masonicare, for example, Steeves said the 31.3 percent rate of developing care plans was due to problems with the “tracking of the discharge document . . . not that it wasn’t actually sent.”
This story was reported under a partnership with the Connecticut Health I-Team (www.c-hit.org).
COMMENT:
This is the comment that I posted online at the paper a few days after the article was published, (as it happened, while I was a patient being tortured at the former New Britain General Hospital, the present day, Hospital Of Central Connecticut).
Pamela Spiro Wagner: “As someone who has been subjected to more use of seclusion and four-point restraints over the past “decade of change” than in the two decades previous it boggles my mind that anyone would even dare to state that things are improving in CT mental health care institutions. During my nearly month-long captivity in the winter of 2013, the Institute of Living in Hartford regularly restrained me to a bed for as long as 19 hours at a time, without ever releasing me for so much as a bathroom break — I had to defecate in my clothing. I was not even released to eat. When I was not in four point restraints “for not following directions, I was in seclusion, which they called the “Quiet Room” and not seclusion, but by CMS definitions, it was seclusion as I was separated from the rest of the patient population by force, and was not permitted to leave the room I was isolated in.
The one time I did actually saunter away, walk down the hall to look out the window, and return to my non-seclusion Quiet Room, I was punished with immediate use of four point restraints, into which I was placed without a struggle, hoping that would make it easier to win my freedom. Alas, for me, there was no way to earn freedom from restraints I never “deserved.” The entire point was discipline, and that would last as long as the staff wanted me to be in shackles to learn my lesson. There was literally nothing I could do, –stay calm, sleep, quietly ask for release — nothing, until they were finally satisfied that I was submissive enough to obey their orders, some 6-19 hours later. But I had to cry Uncle, and submit to a set of degrading humiliating “debriefing questions” that assured them that I took responsibility for my own being restrained and that my behavior would henceforth conform to their norms.
I was surprised to see Natchaug Hospital being given good ratings of any sort. One of their chief psychiatrists on the Adult Unit, a longtime presence their Emeritus psychiatrist you might say, was so insouciant about this job as to be nearly incompetent, but probably hard to fire even for negligence. HIs name I will not mention. He routinely did drive-by visits with his patients– a wave in the hallway might not be a completely standard morning meeting, but it happened often enough that peatients knew that would be all of this doctor they would see for the day. He routinely discharged patients with GAF scores at or around 60, the highest “global assessment of functioning” that one can have and still be rated “disabled” — not because he knew this level of functioning to be the case, but because it made him and his psychiatric ministrations at Natchaug look good. After all, if person comes in with a GAF in the 20s, and barely able to function, and you discharge him or her a week or two and some drive-by counseling sessions later with a GAF of 60, you must be doing a terrific job, esp for a 75 year old doctor not too keen on using anything like trauma-informed or patient-centered care. I had never left a hospital before Natchaug with a GAF higher than 40, but suddenly I rated a 60….by a doctor with whom I never spoke.
Natchaug Hospital, when the nursing director was Sharon B Hinton, APRN, was a decent place, because she made certain that abuses like restraints and seclusion rarely to almost never happened under her watch. I know, because I was there about three times during her administration. I also knew her when she was Hartford Hospital’s psychiatric Head Nurse at CB-3, where she and her never failing humanity and respect for the dignity of every patient made all the difference in the world. I might have come from an abusive hospital in the early 90s, like University of Connecticut’s Dempsey Hospital, which in those days four-pointed people to an iron bedstead, by shackling them spreadeagled to the four corners of the bed, a stress position that is not just tantamount to but is in fact torture. But I would be rescued by someone finding me a bed at Hartford Hospital, where Sharon would discover me arriving there in tears and tell me, unfailingly,”Its not you, Pam, you did nothing wrong, It is the hospital that treats you badly…We don’t have any problem with you, because we treat you well and you respond to it. When they treat you with cruelty, you respond badly…That’s very normal.”
But as to Natchaug…Bravo if they have done away with restraints completely. They had not done so when I was there last in 2012. Nor with seclusion, which was imposed in mostly a disciplinary and arbitrary fashion. Largely it was used to force medication on loud obstreperous patients or for angry fed-up senior nurses to take out their peeves on patients they didn’t particularly like (e.g. me). I still remember one APRN demanding that I be dragged to locked seclusion, and left there alone (despite all Sharon’s previous assurances that such would NEVER happen, that someone would ALWAYS remain in that room with me if I ever ended up there.. Alas, Sharon had left by then, so rogue nurses like D could have their way…) and when I peed on the floor in panic, and took off my clothes they rushed in to take them away from me, and inject me with punishment drugs, then made me stay for an hour alone on the pee-soaked mats, freezing cold, pretending to sleep and calm myself just to convince them I could leave and not bother anyone. I managed to do so, or at least the APRN D. got over her fit of pique and finally released me, but I was not really calm, and when they finally draped two johnnies over my naked body so I could decently traverse the distance to my room, I left, disrobing as I went…Who gave a damn about my flabby flat behind? I certainly did not. And it served them right if everyone got an eyeful…served them right..
Natchaug’s biggest problem was and probably still is a lack of staff cohesiveness and bad morale between the staff nurses and the well-educated techs/mental health workers who were all very dedicated college grads but were treated like grunts…The MHW’s did most of the important patient contact, but were not trusted to write patient notes, or the notes they wrote were never read, or accorded any import. This was not just despicable but very unfortunate in more than one instance during my stay, as the notes they took personally might have saved me from some terrible misunderstandings and outrageous misdiagnoses that harmed me terribly..
Most places use techs who are trained by shadowing for a day or two, which means, badly trained, if at all…
You have to take all such in-hospital diagnoses with such a heavy grain of salt, you know, even when they are labeled with the words, “THIS IS A LEGAL DOCUMENT.” Because they get so much of fact-checkable, factual material garbled that you cannot believe a word it says. And as for diagnosis, well it is all of it opinion, one, and two, it depends largely upon whether you are a likable patient or a disliked one, what they finally say about you on any given day. No one should have that sort of power over another human being, frankly. And the idea that they can brand one for life with certain psychiatric diagnoses just sickens me.
Be that as it may, my recent last experience was beyond the beyond, at Hospital of Central Connecticut, The old New Britain General…and I expect to go back to talk to someone there about it. I always do And I have much to say to them, after the pain and rawness have worn off a little. They considered it SOP to strip me naked and leave me alone in a freezing seclusion cell without any access to human contact, unless they chose to speak to me over a loudspeaker hidden in the ceiling. If not, I was utterly abandoned, no contact or even view of another human being for as long as they wanted to keep me secluded. They also restrained me, having male security guards four-point me stark naked to the bed, before they had the decency to cover me with a light sheet, even though I begged for a blanket for warmth. (A nurse manager came in and shivered, saying “Brrr its cold in here!” but did they relent and let me have a blanket…No, clearly I was not human, didn’t need warmth.)
This is just the tip of the SR iceberg in CT in the current years, Remember this is happening right now, not ten years ago, or before the so-called reforms. Nothing is getting better. Things are worse than ever, And when you are a patient in these hospitals, you have no help, no recourse, anything and everything can be done to you and you have no way to refuse or say “no”. No one will help you, or offer assistance. They can just grab you and seclude you or restrain you without your having the power to stop them or any recourse to make them pause and reconsider. You are powerless to stop anything…And so they get away with it every time. And once it is done, who will fight for you? What lawyer will take your case if the guards hurt your shoulder rotator cuff, or bruise you up, or degrade or humiliate you? No one….so you are deprived of your human and civil rights, completely, but the hospital knows that no one cares enough to fight for you, so they get away with it each and every time, and they know this when they do it. They have nothing to worry about,….You are just another mental patient, a nobody, a nothing.
That’s what you are if you are diagnosed with schizophrenia and hospitalized in CT hospitals in 2014. A nobody that the hospitals can abuse with impunity and will. Just wait and see if any of this changes…I doubt it highly. They have no motivation to change. They don’t think they are doing anything wrong now.”