My comments on this article will follow it. If I can I may highlight points that I particularly wish to discuss.
New Working Definition of ‘Recovery’ from Mental Disorders and Substance Use Disorders
ScienceDaily (Jan. 5, 2012) — A new working definition of recovery from mental disorders and substance use disorders is being announced by the Substance Abuse and Mental Health Services Administration (SAMHSA). The definition is the product of a year-long effort by SAMHSA and a wide range of partners in the behavioral health care community and other fields to develop a working definition of recovery that captures the essential, common experiences of those recovering from mental disorders and substance use disorders, along with major guiding principles that support the recovery definition. SAMHSA led this effort as part of its Recovery Support Strategic Initiative.
The new working definition of Recovery from Mental Disorders and Substance Use Disorders is as follows: A process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential.
“Over the years it has become increasingly apparent that a practical, comprehensive working definition of recovery would enable policy makers, providers, and others to better design, deliver, and measure integrated and holistic services to those in need,” said SAMHSA Administrator, Pamela S. Hyde. “By working with all elements of the behavioral health community and others to develop this definition, I believe SAMHSA has achieved a significant milestone in promoting greater public awareness and appreciation for the importance of recovery, and widespread support for the services that can make it a reality for millions of Americans.”
A major step in addressing this need occurred in August 2010 when SAMHSA convened a meeting of behavioral health leaders, consisting of mental health consumers and individuals in addiction recovery. Together these members of the behavioral health care community developed a draft definition and principles of recovery to reflect common elements of the recovery experience for those with mental disorders and/or substance use disorders.
In the months that have followed, SAMHSA worked with the behavioral health care community and other interested parties in reviewing drafts of the working recovery definition and principles with stakeholders at meetings, conferences, and other venues. In August 2011, SAMHSA posted the working definition and principles that resulted from this process on the SAMHSA blog and invited comments from the public via SAMHSA Feedback Forums. The blog post received 259 comments, and the forums had over 1000 participants, nearly 500 ideas, and over 1,200 comments on the ideas. Many of the comments received have been incorporated into the current working definition and principles.
Through the Recovery Support Strategic Initiative, SAMHSA has also delineated four major dimensions that support a life in recovery:
* Health: overcoming or managing one’s disease(s) as well as living in a physically and emotionally healthy way;
* Home: a stable and safe place to live;
* Purpose: meaningful daily activities, such as a job, school, volunteerism, family caretaking, or creative endeavors, and the independence, income and resources to participate in society; and
* Community: relationships and social networks that provide support, friendship, love, and hope.
Guiding Principles of Recovery
Recovery emerges from hope: The belief that recovery is real provides the essential and motivating message of a better future — that people can and do overcome the internal and external challenges, barriers, and obstacles that confront them.
Recovery is person-driven: Self-determination and self-direction are the foundations for recovery as individuals define their own life goals and design their unique path(s).
Recovery occurs via many pathways: Individuals are unique with distinct needs, strengths, preferences, goals, culture, and backgrounds, including trauma experiences that affect and determine their pathway(s) to recovery. Abstinence is the safest approach for those with substance use disorders.
Recovery is holistic: Recovery encompasses an individual’s whole life, including mind, body, spirit, and community. The array of services and supports available should be integrated and coordinated.
Recovery is supported by peers and allies: Mutual support and mutual aid groups, including the sharing of experiential knowledge and skills, as well as social learning, play an invaluable role in recovery.
Recovery is supported through relationship and social networks: An important factor in the recovery process is the presence and involvement of people who believe in the person’s ability to recover; who offer hope, support, and encouragement; and who also suggest strategies and resources for change.
Recovery is culturally-based and influenced: Culture and cultural background in all of its diverse representations, including values, traditions, and beliefs, are keys in determining a person’s journey and unique pathway to recovery.
Recovery is supported by addressing trauma: Services and supports should be trauma-informed to foster safety (physical and emotional) and trust, as well as promote choice, empowerment, and collaboration.
Recovery involves individual, family, and community strengths and responsibility: Individuals, families, and communities have strengths and resources that serve as a foundation for recovery.
Recovery is based on respect: Community, systems, and societal acceptance and appreciation for people affected by mental health and substance use problems — including protecting their rights and eliminating discrimination — are crucial in achieving recovery.
—————————————————————
At first, I admit, I read the basic definition of recovery and was unimpressed, in fact massively under-whelmed. All I could think was: “A process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential” pretty much describes how anyone should live life. What is so unique and different, I wondered, that this should say anything about recovery from mental illness or substance abuse or that we should care about it? I almost threw up my hands and neglected to finish the article, which would have been a pity as it was worth reading, even if some of the conclusions were a little “pie in the sky,” given the economy and current attitudes towards “entitlements” and public services.
Health, Home, Purpose, Community. Four essential supports for anyone who is attempting to sustain recovery. But as the red words make obvious, it is hard to have a safe and secure home when you don’t have a job, and it is impossible to find a job when you have never worked before and are only just now entering the workforce years late, even as so many others, vastly more experienced, are being laid off. So without those, independence, income and resources go out the window, and with them often go the hope that things can change. Surely if this is often the case for “normal” people, we should expect it also for those with substance abuse problems or mental illness.
Poverty is draining, mentally, physically and spiritually. And it does not foster recovery. But it is a fact of life for many of those with addiction problems and/or mental illnesses. As so many researchers, sociologists and psychologists know, raising oneself from poverty, even in good times is difficult. In hard times such as these, unless you happen to be lucky enough to have a family with resources (in which case you are not truly poverty-stricken) or to reside in safe subsidized housing with enough foodstamps to live on, you are out of luck. How can anyone expect recovery to blossom in such circumstances as hunger and homelessness, not to mention a lack of medical care and medications…But I agree, if health and home can be obtained, then purpose and community can be sought, and the four are indeed recovery’s under-structure; without any or all of them, a person’s stability is easily undermined.
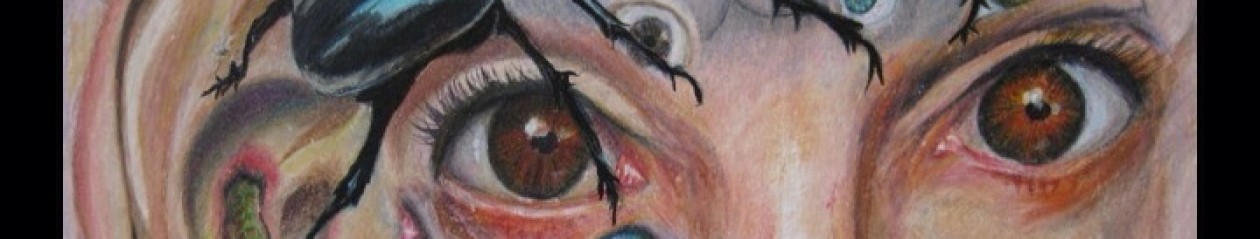
I really liked the guiding principles of recovery, though. Hope is the sine qua non of recovery. If you do not believe that you can get better, do something, feel better, then you will never get there. It once helped me, I thought, that others had hope for me, kept hope alive when i had no hope. And perhaps it did. Because it kept me alive, at a minimum. But it did not help me recover. It was only when I started to feel some hope of my own that recovery began to be possible. In fact, I believe it was only when I began to take up art, teach myself something new, and discovered a brand new interest, talent and passion, that suddenly something opened up in me, in my brain and heart and soul, and hope sprang forth. I had a purpose. I had a purpose, for the first time in decades. I had always had writing, but somehow this was different. For a long time I wasn’t sure why. Then it occurred to me: even if I was only drawing at a table, it was physically active, which meant that it woke me up rather than being dependent on my being sedentary and staying alert. That was the first joyous thing about art: it stimulated me, it kept me awake rather than by its sedentary nature putting me to sleep. I loved writing, never get me wrong on that, I used to love reading when I could attend to books, but because of narcolepsy it was so terribly discouraging that whenever I sat down to write or read I had to battle daily the demon of drowsiness. No matter what I did. Nothing ever helped for long, not even Ritalin. Not, exercise, not diet, not sleeping at night, not, well, nothing. I found Zyprexa such a miracle drug, one that helped me attend and read, but that, that was so sedating in and of itself, that without mega doses of Ritalin, I could barely stay awake to read a few pages.
Somehow, though, art found me, and with it hope was roused. Simple as that.
Or maybe not so simple. First of all, I had to give myself permission to do art. I had to say, it is okay if I don’t write all the time, art is “just as good” as writing, even if my father looks down on it. Many people think art is even better than writing! And I do not have to live to please my father, god knows, though his capacity for devastating judgment is ever mauling my shoulders like a great lion. But what he likes and values, are not absolutes, they are opinions not morals. He is not god, God knows, and I do not need to listen to or absorb what he tries to get me to take in, subliminally or explicitly.
As the next Recovery Principle implies, recovery comes from within, is person-driven, so I had to tell myself that no one could tell me how to do my life but me, and if art kept me alive and awake, so be it. Maybe it wouldn’t be his choice, but so what. It wasn’t his life either, was it?
Recovery cannot be coerced or compelled, only determined by the individual. I would add that treatment too ought to be person-driven, person-determined. That treatment, in-hospital or out-patient should NEVER be coercive but person-centered and self-determined. Why? For the same reason in both cases: It works best that way. Coercion never works; it may appear to but it only breeds trauma and ill will and resentment. It doesn’t foster either health or recovery. Period
However, that Recovery is holistic? While I agree, I had to laugh at the following: “The array of services and supports available should be integrated and coordinated.” I dunno about the “array of services and supports” in your state, but around here there ain’t no such thing…I mean, there are very basic services, like Foodshare and the Food Pantry and hospital inpatient units. But aside from that, and the visiting nurse service that provides/assures medication administration and that grows more precarious every month, I dunno about anything that counts as an “array of services and supports” in this state. I do for myself because sure as shooting the state isn’t going to provide it. Array of services and supports, my eye! You get an appointment for medication every 3 months, in a clinic, and that’s it. And as for integrated and coordinated? What a joke. Who is going to do that? That is like the Centers for Medicare and Medicaid setting new strict regs for seclusion and restraints, and making accreditation of hospitals dependent upon their proper use, and then when it comes time for their yearly review, the psychiatry service isn’t counted or even looked at. Anyhow, I am digressing more and more as I go, I apologize.
Finally, as you know if you have followed my blog, I have had many words to say about traumatic experiences, so I am appreciative of these principles taking the role of trauma into account. If I may read between the lives, since they are talking about “services and supports” being “trauma-informed” perhaps they do mean to speak to the seclusion and restraint issue, as well as the fact that many people have been traumatized and should not be coerced or re-traumatized by treatment. The final passage about respect, however, says it all. No one would have to say a word to anyone providing services and supports about being trauma-informed, if only those needing treatment for substance issues or mental illness had always been treated with respect and dignity.
My apologies for the ineloquence of my writing today. I am coming down with a cold and am not writing up to par. Perhaps the next time I will be back to my usual self.