 You would think that one of the many different pairs of glasses, with some specialized lenses or prisms or bi-focal, or tri-focal or something would help me see through the confusion as I state it in the title above of “dancing and doubling” of images and scenes and texts, oh, especially text, both on-line and hard copy…Or perhaps it simply matters more to me that I cannot read, especially because in two weeks or so I have three or four readings coming up in the space of one week and I fear that I will not be able to simply see my poems on the page. If that should occur, and I do not manage to have each and every poem by heart, what will I do? It so happens that Dr O, or Mary will be at two of the readings, so I can alert her to the problem and ask her to be prepared to (hmmm?) take over for me, at least until it seems that I might be able to resume — though why I could resume I don’t know, since the problem simply recurs immediately and it is only my ability to cope that matters, and by coping I mean my ability to navigate a page of text that has literally gone wild on me, with one line rising up upon another, obliterating it or merging with it, or most commonly simply interspersing with it so I cannot quite make out either one separately and can only try to peer at the paper sidewise as if that could help me parse them out. It of course does nothing, and the words do not separate themselves into readable lines. No, more likely, the words themselves interact and disperse into bits of words or letters, which themselves dance and double and shimmer.
You would think that one of the many different pairs of glasses, with some specialized lenses or prisms or bi-focal, or tri-focal or something would help me see through the confusion as I state it in the title above of “dancing and doubling” of images and scenes and texts, oh, especially text, both on-line and hard copy…Or perhaps it simply matters more to me that I cannot read, especially because in two weeks or so I have three or four readings coming up in the space of one week and I fear that I will not be able to simply see my poems on the page. If that should occur, and I do not manage to have each and every poem by heart, what will I do? It so happens that Dr O, or Mary will be at two of the readings, so I can alert her to the problem and ask her to be prepared to (hmmm?) take over for me, at least until it seems that I might be able to resume — though why I could resume I don’t know, since the problem simply recurs immediately and it is only my ability to cope that matters, and by coping I mean my ability to navigate a page of text that has literally gone wild on me, with one line rising up upon another, obliterating it or merging with it, or most commonly simply interspersing with it so I cannot quite make out either one separately and can only try to peer at the paper sidewise as if that could help me parse them out. It of course does nothing, and the words do not separate themselves into readable lines. No, more likely, the words themselves interact and disperse into bits of words or letters, which themselves dance and double and shimmer.
Oh, it feels hopeless to discuss the matter of vision and what to do about it should I have trouble two weeks from now. So much could happen in those 14 days that nothing is predictable. For instance, I am managing to write this now, without a great deal of tortuous movement and agonizing, though not without trouble — so at this very moment, I could see myself getting through a poetry reading without surrendering to virtual blindness — at this hour of, hmm, at 1AM is it morning or nighttime? Well, I slept from 7:30PM until 11:30PM...Half the night, enough to “take the edge off” my sleepiness. At 11:30 then, for the first time all day, I took a Ritalin, though I had gotten through from 6:30AM -7:30PM of the previous day without any (why? just to prove I could, but without accomplishing anything too). So why now, at 11:30PM? Why in the middle of the night, which to most people would seem the least logical time?
Why? Because I wanted these hours, my time, to be productive, and for that I had to be truly awake and alert, not merely marginally so. (My touchstone of true alertness for years has been how interested I feel…I now know that in my natural state I am never bored, so when I feel a sudden lack of interest in my usual pursuits, that’s when I know I’m getting sleepy. There is no earthly reason why I should have suddenly lost my ordinary passion or fascination, no reason, except that I have become sleepy and sleepiness persents itself as a lack of focus and interest, i.e. as boredom. I am not really bored, I mean only that as a younger person I associated boredom with sleepiness and so whenever I fell asleep doing something I thought I liked, I took that an as indication that I “didn’t really enjoy it after all,” that obviously it bored me. Otherwise, why else would it make me fall sleep? Despite my initial feelings of interest, I evaluated each choice against the proof positive of my falling asleep (which happened whenever I did anything sedentary, including studying), “proof” that I was — the greater truth — bored by it, “proof” that as John Berryman’s poem about “liking valliant fine art” suggests, I had few “internal resources.” Each time I went in for something I thought might spark an interest or fascinate me, as indeed the initial consideration of it did (I cannot give only a few examples, because even just starting in college the choices overwhelmed me, like a penny candy display before a child who has only five pennies to spend. Likewise, there were too many courses and directions I wanted (passionately) to explore, rather than too few. And I could see myself enjoying every one of them, from philosophy to geology!
That was true for me the unexperienced but so far as I knew or thought about it, alert freshman. I still believed that my falling asleep at the movies and during classical music concerts and even simply listening to music I couldn’t sing along with, or in classes where I was not allowed to knit while I listened to the teacher…
For me the senior, there was no longer any penny candy in the display, only a few largely indigestible rounds of “hard tack” that were the very few requirements my “major” required for graduation. I’d actually chosen my major (“Ancient and Medieval Culture” because of its very few requirements and because I’d already fulfilled most of them without meaning to. But the fact that I graduated at all in 1975, that remains a mystery. I had only 27 Brown credits, with a 28th I was fighting for for Spanish taken at the Yale Summer Language Institute, which Brown had warned me in advance it would not grant credit…no matter how well I did. This was their policy, and since Brown only required 28 credits, one credit per full course, rather than most schools bare minimum of 32 or 36, they felt they had a right to insist upon all 28 credits all coming from Brown. I don’t want to go into this here, but I did graduate, and I do not know how or what happened, only that a friend called me after my advisor told her to, and while I had no cap or gown and did not attend, I recieved a diploma, Phi Beta Kappa and my advisor’s encouragment (so much for how well he knew me) in my new life as a pre-med student…More sedentary than ever, more proof I was bored, and more ambivalence about what I had chosen for my lifetime career…
But for the most poignant example, because for me the most painful, take that for years, in fact for as long as I remained an active, if amateur, field botanist (from age 19 until age 39 or even 49 or so, when Lyme disease laid me low), I assumed that while I was devoted, enthusiastic and extremely, even uncannily talented, someone who could recognize and spot a plant I’d never seen before and know everything there was to know about it that one could possibly learn from a glimpse at a guide book, then later a taxonomy chart, and any brief, say 2-page, description as to its medicinal or gustatory uses. Yet I also “knew” that I could never learn plant physiology, or anything technical o biological within plants, such as genetics (important if I want to explore taxonomy) or biochemisrry (important for just about everything else). I knew this was true largely because they “so bored me, they put me right to sleep.” And so, despite an IQ of around 165, so I’d been told, I felt I could not study botany more deeply than the literal surface of plants, because it would put me to sleep…i.e. I was so inadequate in my internal resources that a deeper pursuit of understanding bored me to sleep…
Can you can imagine how I felt, coming to self-understanding of such a dismal sort? And believe me, I was devoted to honesty, at least about myself, to myself.
But I have strayed widely, and perhaps have so diverged from my inital topic, which I vaguely recall started with an image of glasses, as to have rendered it irelevant… Hah! But let me see if I can wend my way back. My discussion of glasses no doubt was in reference to whether or not I could successfully accomplish the poetry readings coming up in 2 or 3 weeks. Which somehow lead to a discussion of my being up at — well, it is now nearly 3AM, so I am awake and alert, having taken Ritalin 2+ hours ago, and I do not feel I have mis-used it, writing this. A discussion of being up and taking the Ritalin, no doubt. Taking the Ritalin… and (althought what follows seems relevant, it was in fact written earlier than all that precedes it) –>
feeling for the first time all day (meaning the entire 24 hour cycle), during the hours when I usually am the most alert and productive, I could not bear wasting time, not even in service of proving to Li that I could in fact forgo Ritalin. (Sure, I am able to do without it, I am not addicted to it I can prove that, if necessary (though to combine doing without it, along with taking Zyprexa is singularly cruel and unusal punishment. The Zyprexa is incredibly sedating for me, so I could never use the intellectual powers it endows me with, simply because I am too sleepy taking it (this has ALWAYS been the problem, and was one reason why Dr O always increased the Ritalin when I took Zyprexa, rather than attempted to decrease it. Another thing that Li does not understand was that Dr O never decreased my Ritalin or made any effort pro forma to do so. For me it was simply one medicine in her armamentarium, and if it worked the best, so be it. She was not even averse to giving me Adderal when and if I told her I wanted to try it. She was completely agreeable to anything I needed in the battle for alertness, and never once accused me to abusing drugs or worse absusing her willingness to prescribe for me. In point of fact, she was right. Why should she accuse me of anything, when all I wanted was what she wanted? As much alertness and “on” time as possible, within the limits imposed by my narcolepsy coupled with the super-sedating effects of Zyprexa. It was because of her absolute trust in me that I felt I could trust her, i.e. trust that if we lowered the Ritalin dose when I did not need it that would not preclude raising it again, if I needed it again. Because of that trust, I could tell her when I no longer needed the dose she was giving me and it was in that fashion that we cut it down from a high of some Adderal plus both ER and regular Ritalin five times a day — this was when I was taking some 35mg of Zyprexa — to only 20 mg of regular Ritalin PRN, of which I rarely take all 5 pills. And she was right, I never got addicted…In point of fact, I was not even habituated, as we discovered as I went on cutting back and back.
One thing Dr O always understood was my need to feel secure in terms of this medication, not to feel that I was ever in danger of its being taken away from me because a new doctor had decided I was either addicted or for the umpteenth time and without proof decided I didn’t have narcolepsy. I do not know how to convince anyone but Li at a minimum ought to listen to the taped Voice of Narcolepsy at the New York Times Health section…These patients speak well on behalf of those ordinary people with my condition, Narcolepsy without Cataplexy. So many docs are unwilling to grasp the notion that many many people suffer — and suffering it truly is — from TRUE narcolepsy, even though we do not have cataplexy. Despite the numbers cited, I myself believe that the reverse is true, that N without C is far more prevalent than N with C…And that better tests, shorter and more discriminating diagnostic tests than long stays at a sleep center will find that Narcolepsy is more comon than people ever thought. (Every time I tell someone I have narcolepsy, they tell me of a ceertain person in their family who falls asleep “just like that”…but was never taken to a sleep specialist etc). Few people and fewer doctors are aware that the falling asleep with one’s face falling into a plate of spaghetti is just a myth, and that narcolepsy has many different faces, just as anxiety, or ADHD or schizphrenia does…Why so many seem satisfied with that myth, and do not question it is beyond me, but they don’t, or it is the rare internist or primary care doc who bothers to question the received wisdom that questions the patient’s motives in asking for Ritalin, rather than the doctor’s compassion in failing to so much as take a sleep history or approach the patient with an open mind…
Dr O knew that I had for way too long been treated as a drug addict when in fact I needed the precise medication other docs considered merely placative. She refused to go that route, and never made it an issue. Even in the hospital, every hospital I went to, she was able to persuade them to give it to me…It was only Li who was not committed to my taking it, disbelieving perhaps that I have narcolepsy (again, again! Why must I put up with this? Is it worth it, or should I go elsewhere, perhaps to a sleep medicine clinic to handle my Ritalin instead of trusting Li to do so…because clearly he cannot be trusted to believe me, to believe Dr O, to believe anything, or even to want to find out!). Why now, when I could have/should have (except that I have spent all the day in a kind of avoidant daze) gone back to sleep, if necessary by taking a dose of Xyrem, as prescribed, why did I take Ritalin at 1AM and stay up writing especially since Li is trying to “wean” me off the Ritalin?
WHY indeed? Why the f–king hell is he trying to “wean me off the Ritalin in the first place, when it was helping me function so well that most people had no idea I had a disability at all? Why question my meds when they are working so well? I’d say to anyone who wants to then interfere, merely for the sake of not using a “potentially addictive drug,” for Chtist’s sake, don’t break what is nicely repaired already. It doesn’t seem necessary, given how well things were going in general. And when they fell apart, I told everyone and him what was wrong: the ABs needed to be changed. I have said that again and again, ever since the hospitalization in February, but nobody is listening to me. I told Dr L then and there that the Bicillin and the Minocycline was not a good combination, that for some reason the two ABs were inadequately treating the three toughstone symptoms, cardinal symptoms in my case, in the sense that if they are taken care of, I seem to be safe from a relapse, but if they are still present, I am not. In point of fact, every single time one of these three symptoms appears or fails to disappear, I eventually wind up in the hospital, either in the spring or in the fall, without fail! (Did I make it through this past spring, or was that when I was in St F/Mt S and trying to tell them that the Minocycline/Bicillin was not aduquate even then? I’d have to look back to see…)
Anyhow, stopping the Ritalin may seem to be fixing something that wasn’t broken, but instead is rather to be breaking something that was functioning extraordinarily well…I mean, if I was writing and doing art and relatively happy and content, why ruin that by stopping one of my essential medications as an outpatient, just because the in-patient docs thought I ought not to take it there? I think Li is in fact trying to stop it for just that reason, because it seemed to be unnecessary inside the hospital, just because there, under those hothouse conditions, having no requirements but sleep, I “did okay.” But doing okay “inside” which is to say, within the protective walls and given the constraints (to say “constraints” is barely a euphemism) of that sort of an institution is scarcely the same as to do okay or even well outside those walls. I didn’t need to stay awake there, or do anything there, and in fact could sleep at will. And so I did, much of the day in fact, every day! If I then needed to sleep at night, well, I could ask for “something for anxiety” anytime, though in point of fact, I mostly could sleep then too. Much of the three week stay was spent sleeping, and when I did not, I was so paranoid that sheer fear and that adrenalin rush kept me going. Near the end of my stay, I became somewhat manic, hypomanic clinically as Li diagnosed it when he saw me. I couldn’t shut up and my speech was — and I felt this as well — pressured. That is a very good word for it, indeed. There was an internal feeling of pressure to get words out in a rush, an unpleasant need to say things, as if they had especial importance and absolutely had to be expressed, even though if I thought about their content, which of course I could not really do in such a state, there was in fact nothing particularly urgent to them.
Well, I am getting tire finally of writing here, and yet I have not finished. I quickly then let me summarize. Because of this recent pressure of speech, coupled with some manic energy put into actually cleaning up this place, and getting more painting and such done, though still hypo manic not truly manic, Li felt something ought to be done to “bring me down” — I am not quoting him so much as quoting the idea…Anyhow, first he suggested stopping the Ritalin, which was okay temporarily, since I already felt enough adrenalin and did not want to add more to my own felt pressure of speech and heart beat. But I had and have no intention of this being anything but temporary…Then he wanted to increase the Topomax, which he said would also decrease the pressure and help hypomania, at the same time that it might help any appetite increase that came with our adding back some Zyprexa, which in his opinion, and of course Elissa the RN’s insistence, was the best drug for me…So far they have only gotten to 2.5mg but even Li has suggested 5mg if I will agree. Now that I have summarized the pharmacological plans for me (including with this, the ultimate decreasing to 0 of my Ritalin) Let me say right here and now, that I will not stand for a rigid “fixing” of the Ritalin problem…
Below I have summarized a few absolute requirements for a psychiatrist, if I am to trust him or her, or continue to see him or her:
One requirement of any psychiatrist I see is that he agree the Ritalin is a necessary medication for an illness, which is narcolepsy, with which I was diagnosed by a sleep specialist at the Sleep Disorders Center at Norwalk Hospital (records available) and it needs to be understood between us that he will not in the middle of therapy decide suddenly to meddle with it (unless I agree and do so not under duress, or decide myself not to take it); it needs to be understood absolutely and without any fishiness or unspoken mistrust, that I am NOT a drug seeker, and that I have narcolepsy, a genuine neurological disease, which needs to be treated, independently of any other illness I might suffer from, so that my being given Ritalin is not dependent on whether or not I agree to take any other drug like Zyprexa etc. though taking Zyprexa might in fact influence the dosage of Ritalin needed.The Rx needs to be permanent as well as flexible according to my needs, which may increase as well as decrease as the ilness waxes, wanes and responds to other drugs and illnesses. Ritalin, however, is never to be used as some sort of bargaining chip…
Argh, Icannot write another word, and in fact, I feel as if I am giving up on a personal letter I was writing to a specific someone. If you are that he or she, you know who you are…I do not!
Rest assured, or at least rest. If I made too many typos and other errors of eloquence or diction, I shall clean them up tomorrow, so reread this then, if you read this today…Be forewarned, it will change between the two times.
Added on Oct 31.
I have decided not to redact the above, but to leave it as is, with all its typos and lacunae and infelicities of grammar and thought. I was writing spontaneously, as I believe was evident enough and I don’t see why that is not adequate for a post once in a while. I would just like to add a clarifying detail or two. What I think I forgot to explain was that between the post on Zyprexa/cancer treatment I experienced a three week hospitalization, which happened very suddenly, though of course, as I mentioned, my visiting nurse had been alert to the possibility of it, even perhaps the inevitability, for at least two weeks…If you understand that, some of this discussion and the one to come above, will seem a little more undersandable.
I will now go to a new post and continue there.
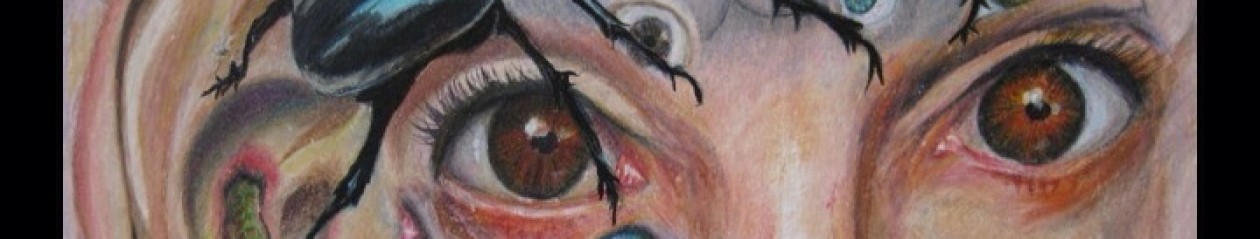


 You would think that one of the many different pairs of glasses, with some specialized lenses or prisms or bi-focal, or tri-focal or something would help me see through the confusion as I state it in the title above of “dancing and doubling” of images and scenes and texts, oh, especially text, both on-line and hard copy…Or perhaps it simply matters more to me that I cannot read, especially because in two weeks or so I have three or four readings coming up in the space of one week and I fear that I will not be able to simply see my poems on the page. If that should occur, and I do not manage to have each and every poem by heart, what will I do? It so happens that Dr O, or Mary will be at two of the readings, so I can alert her to the problem and ask her to be prepared to (hmmm?) take over for me, at least until it seems that I might be able to resume — though why I could resume I don’t know, since the problem simply recurs immediately and it is only my ability to cope that matters, and by coping I mean my ability to navigate a page of text that has literally gone wild on me, with one line rising up upon another, obliterating it or merging with it, or most commonly simply interspersing with it so I cannot quite make out either one separately and can only try to peer at the paper sidewise as if that could help me parse them out. It of course does nothing, and the words do not separate themselves into readable lines. No, more likely, the words themselves interact and disperse into bits of words or letters, which themselves dance and double and shimmer.
You would think that one of the many different pairs of glasses, with some specialized lenses or prisms or bi-focal, or tri-focal or something would help me see through the confusion as I state it in the title above of “dancing and doubling” of images and scenes and texts, oh, especially text, both on-line and hard copy…Or perhaps it simply matters more to me that I cannot read, especially because in two weeks or so I have three or four readings coming up in the space of one week and I fear that I will not be able to simply see my poems on the page. If that should occur, and I do not manage to have each and every poem by heart, what will I do? It so happens that Dr O, or Mary will be at two of the readings, so I can alert her to the problem and ask her to be prepared to (hmmm?) take over for me, at least until it seems that I might be able to resume — though why I could resume I don’t know, since the problem simply recurs immediately and it is only my ability to cope that matters, and by coping I mean my ability to navigate a page of text that has literally gone wild on me, with one line rising up upon another, obliterating it or merging with it, or most commonly simply interspersing with it so I cannot quite make out either one separately and can only try to peer at the paper sidewise as if that could help me parse them out. It of course does nothing, and the words do not separate themselves into readable lines. No, more likely, the words themselves interact and disperse into bits of words or letters, which themselves dance and double and shimmer.