CLick to enlarge

CLICK ON THE PICTURES TO ENLARGE THEM.
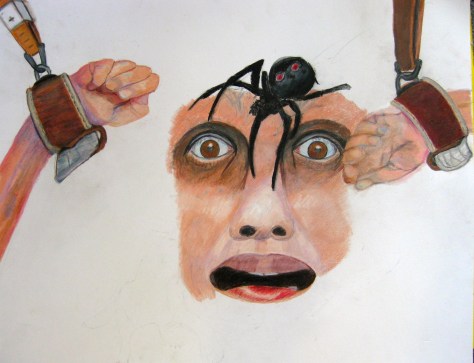
There were few rewards for behavior that toed the line at New Britain General Hospital (HOCC). Mostly it was punishment. If I was found with even a stub of a forbidden pencil, I was carried off to the Supermax seclusion cell, stripped naked and left alone.
At that point, being teeth-chatteringly blue with cold, I would swat a nurse in such a way that she would feel assaulted and bring on the goon squad of “I want to hurt someone today” guards to put me in four point restraints.
Why would I induce this? Because then they would at least cover me up afterwards with the mercy of a sheet, for modesty not warmth mind you, and I would beg for a blanket in vain. But at least my body would be protected from head to toe from the blasts of the A/C up full bore, and I could rest after I had had screamed out my lungs and my despair for a lonely twenty minutes or more.
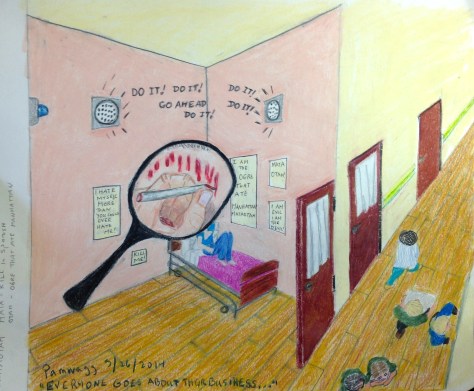
No one cared, no one heard or paid any attention. The doors were double, and the cell was utterly soundproof. NO one ever even knew I was locked in there. When my screaming was too heart-wrenching for the softer ones of the staff down the hall in the room where they had retired to, they simply turned down the monitor and intercom so they didn’t have to listen.
I know, because I heard when the telephone rang, telling the person sitting outside the inner door they could turn it back on now (after I had quieted down). This was brutality of the nth degree. But they always called it treatment for safety, though I mentioned the CMS regs to the security guards one day as they were inflicting their usual pain in order to bring me to the room, and they stopped in their tracks.
“You’re kidding,” one said, “Its true that the only legal reason for seclusion is Imminent Danger to self or others?” (I had been brought there for disturbing the peace…)
I nodded, Look it up. She looked gravely at the others. but proceeded o do what she had been ordered to do anyway. And I proceeded to behave in a wildly immodest and terrified fashion likewise…knowing I would be left alone and freezing for at least two to three hours, no matter how fast I calmed myself.
They didn’t care. it was PROTOCOL…




HOLY SHITE AND URINE TEAM
Her cool wordless RN face expresses nothing
as she scoops the ice cream turd and quickly disinfects.
But I think for her, thinking, knowing this:
“Asshole, shithead, you think
your shit don’t stink…” While I have no working sense of smell,
I know I’m an unofficial pain in the ass here
because no one can be officially PIA
on a psychiatric ward, not even I, the wild shit smearer
who knows no disgust first hand
for not smelling it.
What I know well and sadly is
the consequences of disgusting others,
the distancing, the shunning,
how killing the ultimate loneliness is, double-locked away
in a soundproof seclusion cell.
Shackled naked into leather 4-point restraints, I shriek my soul away,
from the bottom of my lungs for 20 minutes straight.
The illegally silenced intercom remains dumb.
Even the 1:1 monitor positioned behind the door.
peering lazily through the judas-eye of a small plexi-port-hole,
doesn’t really pay attention. Why bother, the shit smearer
gets what she deserves.
Oh, I know I disgust them, what with my out of control turd throwing
and my illegible scribbling with my feces on the wall
but they refuse me so much as a marker and board,
and they won’t sit down to listen when I speak.
Mute for 16 days, I will be heard now, one way or another.
But this is no way to think, and i think without thinking, just do with do do, mindlessly, enraged by trauma.
I foul myself because no one cares,
because their disgust is threaded, even so heat-felted with hatred
they have long forgotten I’m just another patient
with problems bigger than the shit I fling.
Instead, cucumber skinned nurses sneer their disgust,
Bad dog! Bad, bad dog!
But I know dog is just God spelled backwards.
And God created the living world
from dust and mud and excrement.
I am no god, I am Live backwards to Evil:
I create chaos from utter chaos within.
There are always turds to form and fling.
And in the end all they can do is kill me.
Fuck me! Do me a favor you turds, kill me!
But first, you have to silence the hate on your faces,
clean the smeared walls,
and pretend I am nothing to you.
When you came in to take me down,
restrain me for any excuse, even for just wanting a blanket.
you had to breath in my shit, that fear,
and knew what it could do to you.
You’d heard the stories, deadly E-coli, C diff.
Something in me might kill you,
I don’t know what scared you more, my wildyelling
or my excrement.
That was always the struggle. Shit stinks. I stank.
You hated me for my smell. You feared me for what I did.
I know your fear. It was: what would happen if you
lost control of yourself.
Would you, control freaks,
too dance naked in dung?
I understand now why Dr. Michael E. Balkunas, the psychiatrist at New Britain General Hospital (Hospital of Central Connecticut) W-1, general psychiatry, gave up on me. He decided, even after eliciting my brother’s opinion both from a professional and a personal standpoint, and Dr Angela’s equally professional opinion that I do not suffer from Borderline Personality Disorder, to diagnosis me secondarily as exhibiting that disorder.
Oh, he knew I had come in with an acute exacerbation of schizophrenia and that I had PTSD. He knew that I had in my electronic medical record documents stating from other psychiatrists that I do not and never did have any personality disorder, despite in-hospital “behaviors.” But I know why Dr Balkunas diagnosed one. He did it for the same reason the other hospitalist psychiatrists have done it in the past: 1) in order to justify the use of a Behavioral “Treatment” Plan that was tantamount to torture and 2) to excuse his liberal use of seclusion and restraints in instances when they went against all CMS regulatory guidelines. And 3) in order to dismiss me and call my behaviors “manipulative and devious” instead of taking me and what I said seriously.
I also suspect, for all the second shift RN Barbara’s telling me that Michael Balkunas MD is a caring man and “never gives up on a patient” that he DID in fact give up on me. In fact I suspect that he never really tried to deal with or treat me at all, that from the first time he resorted to seclusion and restraints, he knew he had opted to terminate any treatment alliance.
But how did I figure this out? Well, it isn’t as if there ever had been any kind of alliance between us. From the first day after he admitted me from the ER, when he came into my room while I was still mute, he just walked away, saying dismissively, “I won’t talk with you unless you speak.” Immediately I understood that this man was willing to jeopardize everything about me and about my treatment in order to assert his power.
The same thing came into play after I began speaking about a week later. Now the issue was that he would not speak to me, would not deal with me at all but would immediately leave the room if I became angry and spoke with anything resembling a raised voice. (Argh, this was so many shades of Amy Taylor MD at the Institute of Living last year! — and Dr Balkunas tortured me in similar ways with predictable ineffectiveness — but powerful people behave in predictable ways, right? It seems I must have threatened their sense of entitlement. Why else take it out on me? Who am I? I’m a big fat nobody! They could have ignored me or just treated and released me, like anyone else. But instead they did their damnedest to crush me and destroy me. Why? Because in the end, I think I must have triggered some underlying feelings of resentment and impotence in these two psychiatrists and you know you do not threaten to unearth the feelings of a psychiatrist, or at least not with Michael Balkunas MD or with Amy Taylor MD …)
I learned very quickly, but not quickly enough, that everything about the Hospital of Central Connecticut W-1 Unit at New Britain was about coercion and control. Not about trauma-informed, patient-centered care. I don’t know how other patients managed to be discharged from there within a few days, but it would never have been possible for me. Mostly because I was simply too out of control to BE controlled by people who used such methods to undermine any possible calm and stability I might have achieved in those early days. They did NOTHING to help me but take away the very coping methods and objects that might have helped me. They used the carrot-and-stick method liberally, but mostly they used sticks. The very fact that the ED staff had seen fit to seclude me, give me IM meds twice and also to four-point restrain me naked to a bed tells you something about the brutality that reigns supreme there.
You know the very first thing I did was give the ER and the W1 staff a Psychiatric Advanced Directive. It was supposed to help them to help me. But instead they seemed to resent my knowing myself, and wanting them to know how to help me. They reacted badly and worked against it in every way possible, instead helping me. It appeared to anger them that I knew myself, and instead of using it, they did everything in their power to abrogate each and every section of it, right up to the section where it asked them to notify my doctor and my brother when and if they used seclusion and/or restraints despite the warnings.
No one ever called anyone in each instance that they chose to restrain or seclude me, even though I begged them to verbally at the time as well, and this document, which was at the front of my chart all along, stated in no uncertain terms that I wanted both people to be notified.
It was the worst hospitalization I have ever had, and I say that having had many serious and difficult stays. I was not just a difficult patient, I was a pain in the ass, but this was a direct result of the trauma I experienced in the ED and immediately following it on the floor. If I had not been traumatized, on the unit and in the ED, I feel certain that my “behavior,” outrageous, “disgusting,” and out of control as it was, would never have been so damaged. But because everyone saw fit to go against everything advised in the PAD, and do everything they could to re-traumatize me– even after I had a conversation with a nurse about my three experiences with date rape, even after that, she decided to seclude me, involving the forcible removal of me from my room by brute guards who bodily threw me into a cell without any mean s of communication with the world — because of this, they got the regression and degeneration and worsening of symptoms that my PAD predicted would happen. What did they expect? That I would simply thank them?!
I realized, though, the Monday morning of the week he discharged me when he came into my room and asked me how I was doing, that Dr Balkunas, who “never gave up on a patient,” had given up on me. Now, my brother had indicated to him that the “kindness” Dr Balkunas was offering to me by means of involuntary commitment to CVH would be devastating and destructive to the max. I think “Balkie” had had to think about the wisdom of actually sending me there. So he also had to think about whether he actually had any tools at all to “fix me” or cure me as he had promised. Indeed he was no miracle worker and had never held out anything, NOTHING AT ALL, by way or therapy or treatment modalities beside commitment to the state hospital to help me…so without that threat he had nothing to offer me.
The man never once sat down and even talked to me calmly and caringly. I say this because when he sallied forth with his usual opening that Monday morning, How are you? (I had decided finally, with my brother’s encouragement to “play the game.”) I answered with the socially acceptable, “fake” answer, my game plan, not expecting any real psychiatrist worth his salt to accept it, but trying to “play the game” anyway, as I was desperate to be discharged. My answer?
“I’m fine, thank you. How are you?”
Balkunas really didn’t bat an eyelash, the completely social answer was good enough for him, because he had given up trying to help me. Indeed, he had never even tried. So he proceeded, “How are you eating?”
“Fine.”
“How are you sleeping?”
“Fine.”
“Well, if things continue this way and there are no meltdowns I think you can go home on Friday.”
There were indeed meltdowns, even the night before I was discharged I had a meltdown over my supper tray. But Dr B was not on the floor much and didn’t hear of those, and everyone was so sick of me that they didn’t write them up, knowing I was to go home. And I persisted in answering those three magic questions “correctly.” Socially, as I had been taught, against my will, years ago. He never asked me a single other thing, and never talked about anything else at all after that.
The day of discharge came, and the great and caring Dr. Michael Balkunas popped his head into the room. “How are you?”
“I’m fine thank you. How are you?”
“Okay, I will write your discharge papers now.”
The very minute he said that and turned to leave, I put my sunglasses back on, as I saw that taking them off a week prior had served its purpose and it mattered not whether I wore them from that point on or not. I still wear them today, to protect people from my evil…
Dr. Michael Balkunas may talk a great game about helping people but he has very few tools to do so and really it is all pretence. He has medications, which are by and large bogus (though he has been educated by Big Pharma for so long he fails to understand this), and he had commitment proceedings to the state hospital, unless he happens upon a millionaire family willing to spend on their family member. I was not one of those, nor worth it. CVH – for those who are not in the know, CVH—Connecticut Valley Hospital is the last state hospital and the only long term facility for adults on Medicaid in Connecticut – being sent there would have killed me and he and my brother both knew it.
The difference was that my bother was decent enough to care while Balkunas honestly thought it would be good for me to lose my life there. And that was his treatment? Bullshit. He was a bad doctor and despite the cant, he gave up on me to boot. Well, thank god he did.
But you know, I do not forgive his accepting my social “I am fine thank you. How are you” so easily. That was insulting. He was sick of me, and considered me willfully manipulative and devious, otherwise he would not have diagnosed me with the damning BPD diagnosis, which in his hospital means just that you are a PIA, no less and no more. But he might have at least pretended to be a psychiatrist and not just a social buddy. How are you? Fine thank you, How are you? What sort of answer is that? ON the other hand, if he had asked me, what could I have said? We both know I had to get out of there and there was nowhere to go but home. He was not interested in finding out how I was, in talking to me. Not from the first. All he wanted was to medicate me. Which he did. So fuck me. How are you, I am fine thank you how are you? And it wouldn’t have made a rat’s ass worth of difference if I had not been okay, which I wasn’t, so long as I said I was fine, thank you, how are you’
Like I said, it was a game. That was the name of it, Play the Game…
So fuck Michael Balkunas. He is worthless to me, and his add-on personality disorder diagnosis means less than a fig to me. He knew I had schizophrenia and PTSD. He knew the hospital was abusing me. He knows nothing about me, never spent more than 3 minutes with me on any given day. He knows nothing. And I don’t give a flying femtogram about HOCC (the former New Britain General Hospital) except insofar as they ought to ask me back to educate them and improve the situation vis a vis their abusive use of seclusion and restraints, not trauma-informed patient-centered care at all. However since even supposedly trained Nurse Manager Jessica came around to not objecting, and approving their use, I can see that it might be hopeless to do so. Willing though I would be.
Barbara, RN on the second shift. You alone were a lifesaver and a light in a dark tunnel. I wrote in the scraps of paper I called a journal of your kindnesses again and again, and I forgive your being blind to the cruelty of seclusion and restraints, because you have lived with that culture too long, You just need to be re-educated. But you saved my life. Had you not been on duty that weekend before I was discharged, I might not have calmed enough to say to Dr. Balkunas the socially acceptable “I-am-fine-thank-you-how-are- you” mantra that was the magic ticket out of there.
I know no one on W-1 remembers me with anything but relief that I am gone and a great deal of disgust and anger. Ditto for me. I still wake screaming from nightmares about the place and a great deal of anger that I don’t want to let go of. I want to hold onto it long enough to fix the situation of W1, before I forgive anyone. Then we will see.
But for now I am off to Vermont for six weeks to stay with relatives. I hope to heal. I hope I can heal…
Take care of yourself Barbara. You would do well to find a kinder and better place to work and train. I thank YOU for everything. I mean it when I say you saved my life and sanity.
Blessings on you alone, Barbara, the rest of you can FYandGTH.
Miss Wagner
FROM: THE NEW HAVEN REGISTER May 31, 2014

As Connecticut works to improve its mental health system, new federal data shows that hospitals in the state restrain psychiatric patients at more than double the average national rate, with elderly patients facing restraint at a rate seven times the national average.
In addition, the state lags behind in providing adequate post-discharge continuing care plans for psychiatric patients, especially teens and the elderly. Connecticut’s 28 inpatient psychiatric units and hospitals developed continuing-care plans for fewer than 70 percent of patients they discharged from October 2012 to March 2013 — indicating that thousands of patients may have left facilities without adequate treatment and medication plans.
A C-HIT analysis of the federal data, released by the Centers for Medicare & Medicaid Services for the first time, shows that Connecticut ranks in the top fourth of states (11th highest) in the use of physical restraints in inpatient psychiatric facilities — and is the third highest state in restraining patients 65 and older.
Two psychiatric units — at Bridgeport Hospital and Masonicare Health Center in Wallingford — have the 10th and 12th highest rates of restraint use, respectively, among the 1,753 psychiatric facilities nationwide that are included in the federal reports, which cover October 2012 through March 2013.
State and federal guidelines — tightened over the past 15 years, partly in reaction to deaths in Connecticut facilities — say that restraints should be used only in cases of imminent physical danger to a patient or others. They call for less restrictive interventions when patients are acting out aggressively.
But the data show that Bridgeport Hospital, Masonicare and three other Connecticut hospitals — Waterbury, Hartford, Danbury — restrain patients at more than triple the national rate.
James McGaughey, director of the state Office of Protection and Advocacy for Persons with Disabilities, said he was disturbed by both the high rate of restraint use and the low rate of post-discharge plans.
“The numbers are pretty compelling,” he said. “Some of our hospitals have done a significant amount of work on this, but clearly there’s more to be done.”
He suggested that the Department of Public Health, which oversees hospitals and is charged with reviewing annual reports of restraint and seclusion, should “get a little less timid in looking at this.” Hospitals rarely have been cited or penalized in recent years for improperly using restraints, a review of inspection reports shows.
McGaughey noted that the state-run Connecticut Valley Hospital in Middletown has pursued a reduction in restraints and seclusion that has cut its restraint rate significantly in the last five years. The new data show CVH’s rate at .52 hours per 1,000 patient hours — below the statewide rate of 1 hour per 1,000. The national average is .39.
“It’s ironic that our one remaining large state hospital has done such a good job of reducing restraint and seclusion, but you have some very different results at private institutions,” McGaughey said of CVH, which was cited for excessive restraint use in 2007 by the U.S. Justice Department. “What it shows is that it’s possible to address this issue, but you need leadership to effect this kind of culture change.”
Mental health advocates say seclusion and restraint should be avoided because they are traumatic and dangerous to patients and staff.
Alternatives include individualized aggression-management plans, the use of “comfort rooms” or time-out spaces, and one-on-one interventions. Among the innovations at CVH are 22 “comfort rooms,” designed to calm agitated patients, and a reduction in the time interval that a physician’s order of restraint or seclusion can remain in effect, according to a state report.
Yale-New Haven Hospital has a restraint rate of .36 hours per 1,000 patient hours — just below the national average of .39 hours. But its rate of developing care plans for discharged patients is relatively low — 50.36 percent, compared to a national average of 73.5 percent of cases.
Officials at Connecticut hospitals with high rates of restraint say they are working to reduce those incidents, and they stressed that even minimal mobility restrictions, such as soft wrist restraints or brief therapeutic holds, are counted in the federal numbers.
Robert Bernstein, executive director of the Bazelon Center for Mental Health Law, a national advocacy group that successfully sued Connecticut in 2006 to stop housing psychiatric patients in three nursing homes, said he worried that progress made in the early 2000s to reduce restraints might be slipping in some hospitals because of staff shortages and “pushback” from clinicians.
“Some of the procedures put in place may have been weakened, because it’s a lot of work” to use alternative interventions, he said.
Although patients subjected to improper restraint can file complaints, few speak out, Bernstein and others said. Among the exceptions in Connecticut is Pamela Spiro Wagner, a Wethersfield writer and artist with schizophrenia who has cycled in and out hospitals.
In an April “open letter” to the director of a Connecticut psychiatric hospital, Wagner readily conceded that she is a difficult patient — “easily roused to irritability and hostility” — but insisted that her behavior has not warranted her repeatedly being placed in restraints and seclusion, for hours at a time.
“Once you allow staff to use restraints a little, it only takes a little to use them a lot.”
Nationally, the states with the highest restraint use are Minnesota, Washington, South Dakota, Tennessee and New Hampshire. For patients 65 and older, only Nevada and New Hampshire have rates higher than Connecticut, which restrains elderly patients at an average of 7.69 hours per 1,000 hours. Thirty-five states have rates of less than 1 per 1,000 hours; the national average is 1.01 hours per 1,000 hours.
The U.S. facility with the highest restraint rate is Park Ridge Health in North Carolina, which reports 722 hours of restraint use per 1,000 patient hours overall. Among facilities that report serving children ages 2 to 12, Lakeland Regional Medical Center in Florida has the highest restraint use, at 200 hours.
The federal data shows Connecticut psychiatric facilities fare well in some categories, including lower-than-average rates of restraint for children and teenagers. Five hospitals reported no use of restraints for any age group: Sharon, MidState Medical Center, Bristol, John Dempsey and Natchaug hospitals.
And Connecticut’s rate of keeping patients in seclusion is lower than the national average, with half of the state’s psychiatric facilities reporting that they did not use seclusion at all. Nationally, South Dakota, Montana and Washington report the highest use of seclusion, defined as involuntary confinement where a patient is prevented from leaving.
But the state’s over-65 restraint rate is fueled by excessive rates at Masonicare (35.99 hours), Bridgeport Hospital (37.92) and Hartford’s Institute of Living (9.19).
Officials at those hospitals say they have taken steps in the year since the data-reporting period ended to reduce restraint use.
This is the first time that quality measures from psychiatric facilities have been made available by CMS. The federal agency does not penalize facilities for high rates of restraint or inadequate discharge plans. Instead, an agency spokeswoman said, the public reporting is intended to encourage quality improvements and help consumers to make informed decisions.
At Bridgeport Hospital, Dr. Ryan O’Connell, vice president for performance and risk management, said the hospital’s geriatric psychiatric unit serves many patients with dementia and behavioral problems that cannot be managed in other facilities. About 18 months ago, he said, the hospital put in place an “action plan” to reduce restraints, including using “comfort” rooms. Also, in January, a new policy was implemented requiring that the nurse manager be called before any patient is restrained.
“We realized we were going in the wrong direction with restraints” and have since seen a “dramatic drop” in their usage, O’Connell said.
Hartford Hospital’s Institute of Living (IOL), which has a geriatric unit for complex dementia patients, has made similar changes over the past few years, nursing director Ellen Blair said. She said restraints are now rarely used, and only for patient safety. The IOL requires that a physician’s restraint order be reviewed every two hours, rather than every four, which is the standard of care.
“We look at our data every single day” to ensure that restraint and seclusion are being used only as “a last resort,” Blair said.
Masonicare’s acute psychiatric unit serves geriatric patients who frequently are referred because of difficult behaviors and aggression, said spokeswoman Margaret Steeves. When restraints are needed, the hospital uses “the least restrictive restraint, which is typically a seat belt,” she said. Masonicare has an interdisciplinary team reviewing restraint use.
Statewide, the Connecticut Hospital Association has been working with the state Department of Public Health to minimize the use of restraints, said Dr. Mary Cooper, the group’s vice president and chief quality officer. She said the new federal data “indicate that there is more work to be done in this area” and will help to identify best practices.
Nationally, the federal government tightened rules on the use of restraints and seclusion between 2001 and 2007, including time limits on physician orders and strict documentation requirements. The changes were prompted by a series in The Hartford Courant, “Deadly Restraint,” which documented restraint-related deaths in psychiatric facilities nationwide.
In 2007, the U.S. Department of Justice cited the state-run CVH for excessive overuse of unnecessary restraint and seclusion. Since then, policy and training initiatives have significantly reduced restraint episodes — from 26,290 hours in 2000, to 529 hours in 2012 — a state report shows.
State DPH spokesman Bill Gerrish said the agency collects restraint and seclusion reports from hospitals and works to “ensure that care is appropriate.”
McGaughey and Bernstein said they were especially troubled by the failure of many hospitals to develop continuing care plans for discharged patients, and to transmit those plans to the next level of care.
Statewide, Connecticut facilities developed adequate discharge plans 69.4 percent of the time — lower than the national average of 73.5 percent. For teens, hospitals transmitted care plans only 55 percent of the time — lower than the national average of 74 percent — and for seniors, just 42.7 percent of the time, below the national average of 56 percent.
Discharged patients are supposed to receive care plans containing their diagnoses, reasons for hospitalization, medications and treatment recommendations.
The federal data shows that 10 Connecticut hospitals, including Waterbury Hospital, Masonicare and Yale-New Haven Hospital, properly transmitted care plans to the next provider in less than half of cases.
A few hospitals — St. Mary’s, Bristol, Norwalk, Natchaug Hospital and Southwest Connecticut Mental Health — transmitted care plans more than 90 percent of the time.
McGaughey said that without continuing care plans directing further treatment, many discharged patients may languish in nursing homes, shelters or land back in the hospital.
“The lack of continuity of care, to me, is a huge issue,” he said. “It’s a pretty brutal business — insurance companies want you to medicate and discharge as fast as possible. The question is, what happens after they’re out?”
Bernstein said the lack of attention to continuing care plans was “jaw-dropping.”
“Those numbers should be at 100 percent,” Bernstein said. “It’s shameful.”
Hospitals with low rates of discharge care plans blamed much of that lag on their failure to document that the paperwork was done.
At Masonicare, for example, Steeves said the 31.3 percent rate of developing care plans was due to problems with the “tracking of the discharge document . . . not that it wasn’t actually sent.”
This story was reported under a partnership with the Connecticut Health I-Team (www.c-hit.org).
COMMENT:
This is the comment that I posted online at the paper a few days after the article was published, (as it happened, while I was a patient being tortured at the former New Britain General Hospital, the present day, Hospital Of Central Connecticut).
Pamela Spiro Wagner: “As someone who has been subjected to more use of seclusion and four-point restraints over the past “decade of change” than in the two decades previous it boggles my mind that anyone would even dare to state that things are improving in CT mental health care institutions. During my nearly month-long captivity in the winter of 2013, the Institute of Living in Hartford regularly restrained me to a bed for as long as 19 hours at a time, without ever releasing me for so much as a bathroom break — I had to defecate in my clothing. I was not even released to eat. When I was not in four point restraints “for not following directions, I was in seclusion, which they called the “Quiet Room” and not seclusion, but by CMS definitions, it was seclusion as I was separated from the rest of the patient population by force, and was not permitted to leave the room I was isolated in.
The one time I did actually saunter away, walk down the hall to look out the window, and return to my non-seclusion Quiet Room, I was punished with immediate use of four point restraints, into which I was placed without a struggle, hoping that would make it easier to win my freedom. Alas, for me, there was no way to earn freedom from restraints I never “deserved.” The entire point was discipline, and that would last as long as the staff wanted me to be in shackles to learn my lesson. There was literally nothing I could do, –stay calm, sleep, quietly ask for release — nothing, until they were finally satisfied that I was submissive enough to obey their orders, some 6-19 hours later. But I had to cry Uncle, and submit to a set of degrading humiliating “debriefing questions” that assured them that I took responsibility for my own being restrained and that my behavior would henceforth conform to their norms.
I was surprised to see Natchaug Hospital being given good ratings of any sort. One of their chief psychiatrists on the Adult Unit, a longtime presence their Emeritus psychiatrist you might say, was so insouciant about this job as to be nearly incompetent, but probably hard to fire even for negligence. HIs name I will not mention. He routinely did drive-by visits with his patients– a wave in the hallway might not be a completely standard morning meeting, but it happened often enough that peatients knew that would be all of this doctor they would see for the day. He routinely discharged patients with GAF scores at or around 60, the highest “global assessment of functioning” that one can have and still be rated “disabled” — not because he knew this level of functioning to be the case, but because it made him and his psychiatric ministrations at Natchaug look good. After all, if person comes in with a GAF in the 20s, and barely able to function, and you discharge him or her a week or two and some drive-by counseling sessions later with a GAF of 60, you must be doing a terrific job, esp for a 75 year old doctor not too keen on using anything like trauma-informed or patient-centered care. I had never left a hospital before Natchaug with a GAF higher than 40, but suddenly I rated a 60….by a doctor with whom I never spoke.
Natchaug Hospital, when the nursing director was Sharon B Hinton, APRN, was a decent place, because she made certain that abuses like restraints and seclusion rarely to almost never happened under her watch. I know, because I was there about three times during her administration. I also knew her when she was Hartford Hospital’s psychiatric Head Nurse at CB-3, where she and her never failing humanity and respect for the dignity of every patient made all the difference in the world. I might have come from an abusive hospital in the early 90s, like University of Connecticut’s Dempsey Hospital, which in those days four-pointed people to an iron bedstead, by shackling them spreadeagled to the four corners of the bed, a stress position that is not just tantamount to but is in fact torture. But I would be rescued by someone finding me a bed at Hartford Hospital, where Sharon would discover me arriving there in tears and tell me, unfailingly,”Its not you, Pam, you did nothing wrong, It is the hospital that treats you badly…We don’t have any problem with you, because we treat you well and you respond to it. When they treat you with cruelty, you respond badly…That’s very normal.”
But as to Natchaug…Bravo if they have done away with restraints completely. They had not done so when I was there last in 2012. Nor with seclusion, which was imposed in mostly a disciplinary and arbitrary fashion. Largely it was used to force medication on loud obstreperous patients or for angry fed-up senior nurses to take out their peeves on patients they didn’t particularly like (e.g. me). I still remember one APRN demanding that I be dragged to locked seclusion, and left there alone (despite all Sharon’s previous assurances that such would NEVER happen, that someone would ALWAYS remain in that room with me if I ever ended up there.. Alas, Sharon had left by then, so rogue nurses like D could have their way…) and when I peed on the floor in panic, and took off my clothes they rushed in to take them away from me, and inject me with punishment drugs, then made me stay for an hour alone on the pee-soaked mats, freezing cold, pretending to sleep and calm myself just to convince them I could leave and not bother anyone. I managed to do so, or at least the APRN D. got over her fit of pique and finally released me, but I was not really calm, and when they finally draped two johnnies over my naked body so I could decently traverse the distance to my room, I left, disrobing as I went…Who gave a damn about my flabby flat behind? I certainly did not. And it served them right if everyone got an eyeful…served them right..
Natchaug’s biggest problem was and probably still is a lack of staff cohesiveness and bad morale between the staff nurses and the well-educated techs/mental health workers who were all very dedicated college grads but were treated like grunts…The MHW’s did most of the important patient contact, but were not trusted to write patient notes, or the notes they wrote were never read, or accorded any import. This was not just despicable but very unfortunate in more than one instance during my stay, as the notes they took personally might have saved me from some terrible misunderstandings and outrageous misdiagnoses that harmed me terribly..
Most places use techs who are trained by shadowing for a day or two, which means, badly trained, if at all…
You have to take all such in-hospital diagnoses with such a heavy grain of salt, you know, even when they are labeled with the words, “THIS IS A LEGAL DOCUMENT.” Because they get so much of fact-checkable, factual material garbled that you cannot believe a word it says. And as for diagnosis, well it is all of it opinion, one, and two, it depends largely upon whether you are a likable patient or a disliked one, what they finally say about you on any given day. No one should have that sort of power over another human being, frankly. And the idea that they can brand one for life with certain psychiatric diagnoses just sickens me.
Be that as it may, my recent last experience was beyond the beyond, at Hospital of Central Connecticut, The old New Britain General…and I expect to go back to talk to someone there about it. I always do And I have much to say to them, after the pain and rawness have worn off a little. They considered it SOP to strip me naked and leave me alone in a freezing seclusion cell without any access to human contact, unless they chose to speak to me over a loudspeaker hidden in the ceiling. If not, I was utterly abandoned, no contact or even view of another human being for as long as they wanted to keep me secluded. They also restrained me, having male security guards four-point me stark naked to the bed, before they had the decency to cover me with a light sheet, even though I begged for a blanket for warmth. (A nurse manager came in and shivered, saying “Brrr its cold in here!” but did they relent and let me have a blanket…No, clearly I was not human, didn’t need warmth.)
This is just the tip of the SR iceberg in CT in the current years, Remember this is happening right now, not ten years ago, or before the so-called reforms. Nothing is getting better. Things are worse than ever, And when you are a patient in these hospitals, you have no help, no recourse, anything and everything can be done to you and you have no way to refuse or say “no”. No one will help you, or offer assistance. They can just grab you and seclude you or restrain you without your having the power to stop them or any recourse to make them pause and reconsider. You are powerless to stop anything…And so they get away with it every time. And once it is done, who will fight for you? What lawyer will take your case if the guards hurt your shoulder rotator cuff, or bruise you up, or degrade or humiliate you? No one….so you are deprived of your human and civil rights, completely, but the hospital knows that no one cares enough to fight for you, so they get away with it each and every time, and they know this when they do it. They have nothing to worry about,….You are just another mental patient, a nobody, a nothing.
That’s what you are if you are diagnosed with schizophrenia and hospitalized in CT hospitals in 2014. A nobody that the hospitals can abuse with impunity and will. Just wait and see if any of this changes…I doubt it highly. They have no motivation to change. They don’t think they are doing anything wrong now.”

I haven’t spoken out loud in several weeks
bullied into a frightened by myself silence.
Though what does “speechless” mean
in these days of text-to-speech software,
with its choice of Vikki or Samantha or Victoria voices,
Or when I’m possessed of a blogging platform
and writing fluency enough to speak my mind to my heart’s content?
Still, being mute is not a manner of speaking.
i tell you I could speak, I can talk. Nothing physical impedes
my tongue, or locks my lips,
except my brain’s hallucinated snarls, like Jerry Mahoney
and Charlie McCarthy thrown into surrounding shadows
ordering up this stoppage, blockage, blockade.
Now, like that fire-fangled bird at the end of the mind
feathered unlucky, tarred, locked in golden cage
my voice remains only a memento
of everything that I wanted
to say, but couldn’t get out, I couldn’t get out, I couldn’t get it out…
*In the Greek myth, Philomela is raped and has her tongue cut out by Tereus, the husband of her sister Procne. Rendered mute, Philomela weaves a tapestry detailing the crime to inform her sister, who, enraged, takes revenge on Tereus. At the end of the story, both Procne and Philomela are transformed into birds. Some versions have Philomela become a nightingale, the female of which does not sing. In other versions she becomes a swallow, which is a non-singing bird.

I think it is time to explain the trigger for my being mute these five days now, and what happened to start the voices unloosing their barrage of hatred on me. In order to do so, I take a huge risk, because I may unleash more of what happened rather than less. But at least part of what happened was real, the trigger was at least, and it disturbed me deeply. I need also to say that when I tagged yesterday’s audio file “abuse” as well as “health” I meant it. It is almost always abuse of some sort, verbal, emotional or physical abuse that triggers the voices and self-hatred has in the past triggered muteness.
So let me be up front: It was “Alice’s” comment five days ago in which she said, “I think you are a bit of a bully”…which was the specific trigger for all of this. Now, as I read through it — reposted below — I see that nothing she wrote has any bearing on either the post she commented under (which I didn’t write) or anything else I have had to say. But first let me take it point by point. Note that Alice’s comments, for clarity, are in color.
Alice, you wrote: “I must say there is no consistency in your writings. You say about how well Yale New Haven Psychiatric – Hospital treated you and the next entry indicates the opposite- how awful they were to you.”
I must write about inconsistencies and the facts as they happened, and I am sorry if that discomfits you, Alice. But the first experience in the early spring was very gentle and positive, and the other, as I wrote before, was brutal. Nonetheless that is not an “inconsistency in my writing” just an inconsistency in my treatment. You must be someone who is very unhappy with the world as the world tends to be “inconsistent.” Even the weather has a habit of changing, at least it is famously so in New England and I suspect that nowhere in the US has entirely “consistent weather.” Of course there are those people who need hobgoblins…
Alice continues on the issue of consistency: “You say you don’t like anti-psychotic medications yet you take them (and you also don’t like anti-depressants – yet you take them…”
In my defense,I think mature adults often do things they don’t like, even taking medications they don’t like. Most cancer patients hate chemotherapy but take the pills etc anyway. I don’t think merely disliking a medication is reason by and of itself not to take it. Nor to criticize anyone for being inconsistent. There are plenty of reasons to do things you may not like. Many people don’t like eating vegetables, but they sure as shooting ought to eat them!
On one other hand, I more than dislike antipsychotic drugs, I deeply distrust them. I do not believe they work. I do not believe they were developed on any scientific basis or are necessary on any but the shortest of short term bases, if that.
That said, on the other other hand, I both took and was forced to take antipsychotic drugs for decades, from the oldest Thorazine and Mellaril at doses up to 1500mg, to weekly IM injections of Prolixin, then on to Clozaril, which nearly killed me, transitioning to seizure-inducing Seroquel to catatonia-inducing Risperdal then eventually to 35 mg of Zyprexa, which made me gain 70 pounds. Given this history, I think I can be excused from blame for withdrawal-induced psychosis when I try to stop my present two anti-psychotic meds, a very real and difficult situation that a growing number of researchers and physicians now acknowledge, including Robert Whitaker and Joanna Moncrieff among others.
Alice notes: “for example why would you need your Zoloft reinstated when you had your sudden “depression” after it was taken away. )I thought these pills didn’t work.”
What I said was that SSRI’s do not work as their developers state they do. They do not relieve depression by selectively inhibiting serotonin re-uptake at the pre-synaptic neuron. Yes, they DO selectively inhibit this process, but it isn’t necessary, and it isn’t an anti-depressant mechanism. Why? Because the serotonin levels in depressed people’s brains have been shown NOT to be lower than anyone else’s. If you had read what I wrote, you would have understood that I indicated that SSRIs are not placebos, they are not inactive substances, so they do something. They are psycho-active, after all they alter serotonin levels! So they change something in the brain, and that change — any change – may make a depressed person feel better, temporarily. But I have never met anyone who felt permanently better on a single level dose of an SSRI and no one knows for certain what these drugs are doing. I think this is problematic. But I especially think it is FOUL and dangerous to tell a depressed person that they have a chemical imbalance of serotonin that the drug is regulating. That is just a downright lie.
As for my sudden “depression” when my dose of 75mg of Zoloft was lowered? Who can say what happened? It may have been that the nurse/director who was my protector at the hospital was away for a few days too at the time, and I sensed the difference…All I know is, well, what happened. I only report the events, neither justifying them nor attempting to make the case that Zoloft “works.” In fact, 6 months later at Yale, when I was down to 50 mg of Zoloft, Dr Milstein felt that I should just come off it entirely, which I did without difficulty. I have no wish to start it again
Oh yes, Ritalin you take but that’s for a “physical” problem so that’s Okay.
Yes, in fact that is the case. My question is, why is it any of your business and why do you care?
Alice, you then proceeded out of the blue to write: “I think you are a bit of a bully and I think that you think you are profoundly smart. But I’m not taken in…………”
First I want to say, Alice, that I’m not too concerned about my intelligence…I’m certainly not worried about you think about my intelligence, in any event. But it was here, where you called me a bully, that the voices were triggered. Instantly, specifically, instantaneously. In fact, the minute I read those words, the trouble began. And even though I managed to pen a calm enough response, my heart started beating rapidly and the voices muttering louder and louder in the background even as I wrote. I cannot explain — though of course this whole post is trying to — just what happened. I felt my ears explode with the pressure of deep sea diving and as if a huge bell were clanging in my head.
You called me a bully. Me, a bully? Why? Were you just reaching for the worst name you could call me? Certainly, it incorporates my worst fear in the world and it was as if you just knifed my jugular… I didn’t know how to defend myself. Before I knew it, the first thing that happened was that the voices zeroed in for an attack, snarling, blaming me for everything wrong I’d ever done. Believe me, they remember every detail! And more and worse, they blamed me for everything wrong ANYONE had ever done! Before I knew it, I was Dr Mengele, Heinrich Himmler, and Adolf Hitler rolled into one.
Did you, Alice, know this? Did you intend for this to happen? Did you want this shit to hit the fan and intend for me to feel so terrible? Did you want me to feel in fact God-forsaken? I sensed that you did. I sensed that you wanted me to feel desperate, and desperately alone. I sensed then that you wanted me to HATE myself and perhaps even to KILL myself as a response…After all, you called me a bully! You would only do that if you wanted repercussions to ensue: Bullies make people commit suicide, so wouldn’t the punishment for bullies be to kill themselves in turn? What else can they do to make up for the evil that they have caused? (NOTE: I would never ask anyone else to so punish themselves; only I myself can never be forgiven for the evil I have done. I am unforgivable, nothing I do can ever be forgiven…But you, Alice, who know me so well, knew this, didn’t you?)
You see, Alice, what you unleashed? Do you see?
No, you wouldn’t see. You couldn’t possibly see. You would have no idea, because you don’t know me at all. You don’t know anything about me, not in the way you pretend you do…The person “Pam” you think you know is all in your mind, a fantasy created out of your imagination to suit your own angry needs and purposes.
But the thing is, Alice, you know what? It is not I who am the bully in the end. I understand this now. I may be a lot of things, and I may be Evil, but I am not a bully. You do not know me. You know nothing of me but my writings. Even if lurking incognito on my blog you are actually one of the staff members at Yale or Hartford Hospital, pursuing me, you would still know nothing about me, not really, and would never be qualified to call me a bully. None of my friends have ever called me a bully. No one who has ever met me socially even briefly or just once has ever called me a bully. Why? Because I am nothing even remotely like a bully.
Instead, Alice. you have proved yourself to be an abusive person who lashes out at strangers and who says harmful and hurtful things to vulnerable strangers, regardless of whether you know these things to be true or not. Look in the mirror, Alice. Look yourself square in the face because you are angry and you are bitter, and you, Alice, YOU ARE THE BULLY.
Now, let me tell you something else. You think you can get away with it because you did not use your last name, safely tucked away at several states distance or at least protected by your anonymity.,. That because I don’t know who you are, I can do nothing about it. But ALICE, I have my methods of investigating and I know your last name. I also have two photographs of you — and I will post them and name you publicly right here on my blog if you EVER write anything cruel or abusive like this to or about me or to or about anyone else on my blog again.
I hope I make myself perfectly clear on this.
Now, you know what? I was going to go on to “disprove” the rest of your comment, but suddenly I realized I don’t have anything more to say you. Nothing you wrote holds any value .
I’m tired, and it has been a long devastating night. I am going to bed…We will see what the day brings. Whether it will bring back speech or more devastating voices I do not want to say. I can only hope things improve…If not, at the very least you know where I stand.
Pam
I know this audio file may be difficult to understand, but this is what happens when the voices go haywire…I can’t speak. And I cannot even tell you what triggered it, but something did. I tried to go to a Voice Hearers workshop on Tuesday about Taboo and Dangerous voices, but i could scarcely enter the building. I had to “get permission” just to open the door, and when I did, I could not stay…Just could not stay. Forget it. I’m worthless.
I THOUGHT THIS WAS INCREDIBLY WELL WRITTEN AND IMPORTANT INFORMATION. SEE CREDITS AT THE BOTTOM. Posted on January 12, 2014 by annecwoodlen THINGS YOUR DOCTOR SHOULD TELL YOU ABOUT ANTIDEPRESSANTS September 12, 2012 By Paul W. Andrews, Lyndsey Gott & J. Anderson Thomson, Jr. Antidepressant medication is the most commonly prescribed treatment for people with depression. They are also commonly prescribed for other conditions, including bipolar depression, post-traumatic stress disorder, obsessive-compulsive disorder, chronic pain syndromes, substance abuse and anxiety and eating disorders. According to a 2011 report released by the US Centers for Disease Control and Prevention, about one out of every ten people (11%) over the age of 12 in the US is on antidepressant medications. Between 2005 and 2008, antidepressants were the third most common type of prescription drug taken by people of all ages, and they were the most frequently used medication by people between the ages of 18 and 44. In other words, millions of people are prescribed antidepressants and are affected by them each year. The conventional wisdom is that antidepressant medications are effective and safe. However, the scientific literature shows that the conventional wisdom is flawed. While all prescription medications have side effects, antidepressant medications appear to do more harm than good as treatments for depression. We reviewed this evidence in a recent article published in the journal Frontiers in Psychology (freely available here). The widespread use of antidepressants is a serious public health problem, and it raises a number of ethical and legal issues for prescribers (physicians, nurse practitioners). Here, we summarize some of the most important points that prescribers should ethically tell their patients before they prescribe antidepressant medications. We also discuss the ways that prescribers could be held legally liable for prescribing antidepressants. Finally, we implore practitioners to update the informed consent procedure for antidepressant medication to reflect current research and exercise greater caution in the prescription of antidepressants.
Most antidepressants are designed to alter mechanisms regulating serotonin, an evolutionarily ancient biochemical found throughout the brain and the rest of the body. In the brain, serotonin acts as a neurotransmitter—a chemical that controls the firing of neurons (brain cells that regulate how we think, feel, and behave). However, serotonin evolved to regulate many other important processes, including neuronal growth and death, digestion, muscle movement, development, blood clotting, and reproductive function. Antidepressants are most commonly taken orally in pill form. After they enter the bloodstream, they travel throughout the body. Most antidepressants, such as the selective serotonin reuptake inhibitors (SSRIs), are intended to bind to a molecule in the brain called the serotonin transporter that regulates levels of serotonin. When they bind to the transporter, they prevent neurons from reabsorbing serotonin, which causes a buildup of serotonin outside of neurons. In other words, antidepressants alter the balance of serotonin in the brain, increasing the concentration outside of neurons. With long-term antidepressant use, the brain pushes back against these drugs and eventually restores the balance of serotonin outside of the neuron with a number of compensatory changes. It is important to realize that the serotonin transporter is not only found in the brain—it is also found at all the major sites in the body where serotonin is produced and transported, including the gut and blood cells called platelets. Since antidepressants travel throughout the body and bind to the serotonin transporter wherever it is found, they can interfere with the important, diverse processes regulated by serotonin throughout the body. While physicians and their patients are typically only interested in the effects of antidepressants on mood, the harmful effects on other processes in the body (digestion, sexual function, abnormal bleeding, etc.) are perfectly expectable when you consider how these drugs work.
Many people who have suffered from depression report a substantial symptom-reducing benefit while taking antidepressants. The problem is that symptoms are also substantially reduced when people are given a placebo—a sugar pill that lacks the chemical properties of antidepressant medications. In fact, most of the improvement that takes place during antidepressant treatment (approximately 80%) also takes place with a placebo. Of course, antidepressants are slightly more effective than placebo in reducing symptoms, but this difference is relatively small, which is what we mean when we say that antidepressants have a “modest” ability to reduce depressive symptoms. The pushback of the brain increases over months of antidepressant treatment, and depressive symptoms commonly return (frequently resulting in full blown relapse). Often this compels practitioners to increase the dose or switch the patient to a more powerful drug. Prescribers fail to appreciate that the return of symptoms often occurs because the brain is pushing back against the effect of antidepressants. 3. The risk of relapse is increased after antidepressant medication has been discontinued Another effect of the brain pushing back against antidepressants is that the pushback can cause a relapse when you stop taking the drug. This pushback effect is analogous to the action of a spring. Imagine a spring with one end attached to a wall. An antidepressant suppresses the symptoms of depression in a way that is similar to compressing the spring with your hand. When you stop taking the drug (like taking your hand off the spring from its compressed position), there is a surge in the symptoms of depression (like the overshoot of the spring before it returns to its resting position). The three month risk of relapse for people who took a placebo is about 21%. But the three month risk of relapse after you stop taking an SSRI is 43%—twice the risk. For stronger antidepressants, the three month risk is even higher.
Antidepressants can kill neurons (see our article for a review). Many medical practitioners will be surprised by this fact because it is widely believed in the medical community that antidepressants promote the growth of new neurons. However, this belief is based on flawed evidence—a point that we address in detail in our article. One way antidepressants could kill neurons is by causing structural damage of the sort often found in Parkinson’s disease. This neurological damage might explain why some people taking antidepressant medication can develop Parkinsonian symptoms and tardive dyskinesia, which is characterized by involuntary and repetitive body movements. Many prescribers mistakenly think these syndromes only occur in patients taking antipsychotic medications.
Recent research indicates that antidepressants may increase the risk of cancer outside of the brain, such as breast cancer. However, the neuron-killing properties of antidepressants may make them potentially useful as treatments for brain cancers, and current research is testing this possibility.
Since neurons are required for proper brain functioning, the neuron-killing effects of antidepressants can be expected to have negative effects on cognition. In rodents, experiments have found that prolonged antidepressant use impairs the ability to learn a variety of tasks. Similar problems may exist in humans. Numerous studies have found that antidepressants impair driving performance, and they may increase the risk of car accidents. Recent research on older women also indicates that prolonged antidepressant use is associated with a 70% increase in the risk of mild cognitive impairment and an increase in the risk of probable dementia. 7.Antidepressants are associated with impaired gastrointestinal functioning The action of antidepressants results in elevated levels of serotonin in the intestinal lining, which is associated with irritable bowel syndrome. Indeed, antidepressants have been found to cause the same symptoms as irritable bowel syndrome—pain, diarrhea, constipation, indigestion, bloating and headache. In a recent study, 14-23% of people taking antidepressants suffered these side effects. 8. Antidepressants cause sexual dysfunction and have adverse effects on sperm quality. Depression commonly causes problems in sexual functioning. However, many antidepressants make the problem worse, impairing sexual desire, arousal, and orgasm. The most widely studied and commonly prescribed antidepressants—Celexa, Effexor, Paxil, Prozac, and Zoloft—have been found to increase the risk of sexual dysfunction by six times or more. Evidence from case studies suggests that antidepressants may also interfere with attachment and romantic love. Some antidepressants have been found to negatively impact sperm structure, volume, and mobility. 9. Antidepressant use is associated with developmental problems Antidepressant medication is frequently prescribed to pregnant and lactating mothers. Since SSRIs can pass through the placental barrier and maternal milk, they can affect fetal and neonatal development. Generally, if SSRIs are taken during pregnancy, there is an increased risk of preterm delivery and low birth weight. Exposure during the first trimester can increase the risk of congenital defects and developing an autism spectrum disorder, such as Asperger’s Syndrome. Third trimester SSRI exposure is associated with an increased risk of persistent pulmonary hypertension in the newborn (10% mortality rate) and medication withdrawal symptoms such as crying, irritability, and convulsions. Prenatal exposure to SSRIs is also associated with an increased risk of respiratory distress, which is the leading cause of death of premature infants. 11\\10. Antidepressant use is associated with an increased risk of abnormal bleeding and stroke Serotonin is crucial to platelet function and promotes blood clotting, which is important when one has a bleeding injury. Patients taking SSRIs and other antidepressants are more likely to have abnormal bleeding problems (for a review see our article). They are more likely to have a hemorrhagic stroke (caused by a ruptured blood vessel in the brain) and be hospitalized for an upper gastrointestinal bleed. The bleeding risks are likely to increase when SSRIs are taken with other medications that reduce clotting, such as aspirin, ibuprofen, or Coumadin . 11. Antidepressants are associated with an increased risk of death in older people. Depression itself is associated with an increased risk of death in older people—primarily due to cardiovascular problems. However, antidepressants make the problem worse. Five recent studies have shown that antidepressant use is associated with an increased risk of death in older people (50 years and older), over and above the risk associated with depression. Four of the studies were published in reputable medical journals—The British Journal of Psychiatry, Archives of Internal Medicine, Plos One, and the British Medical Journal—by different research groups. The fifth study was presented this year at the American Thoracic Society conference in San Francisco. In these studies, the estimated risk of death was substantial. For instance, in the Women’s Health Initiative study, antidepressant drugs were estimated to cause about five deaths out of a 1000 people over a year’s time. This is the same study that previously identified the dangers of hormonal replacement therapy for postmenopausal women. In the study published in the British Medical Journal, antidepressants were estimated to cause 10 to 44 deaths out of a 1000 people over a year, depending on the type of antidepressant. In comparison, the painkiller Vioxx was taken off the market in the face of evidence that it caused 7 cardiac events out of 1000 people over a year. Since cardiac events are not necessarily fatal, the number of deaths estimated to be caused by antidepressants is arguably of much greater concern. An important caveat is that these studies were not placebo-controlled experiments in which depressed participants were randomly assigned to placebo or antidepressant treatment. For this reason, one potential problem is that perhaps the people who were taking antidepressants were more likely to die because they had more severe depression. However, the paper published in the British Medical Journal was able to rule out that possibility because they controlled for the pre-medication level of depressive symptoms. In other words, even among people who had similar levels of depression without medication, the subsequent use of antidepressant medications was associated with a higher risk of death. These studies were limited to older men and women. But many people start taking antidepressants in adolescence or young adulthood. Moreover, since the risk of a relapse is often increased when one attempts to go off an antidepressant (see point 3 above), people may remain on medication for years or decades. Unfortunately, we have no idea how the cumulative impact of taking antidepressants for such a long time affects the expected lifespan. In principle, long-term antidepressant use could shave off years of life. It is commonly argued that antidepressants are needed to prevent depressed patients from committing suicide. Yet there is a well-known controversy over whether antidepressants promote suicidal behavior. Consequently, it is not possible to reach any firm conclusions about how antidepressants affect the risk of suicidal behavior. However, most deaths attributed to antidepressants are not suicides. In other words, antidepressants appear to increase the risk of death regardless of their effects on suicidal behavior. We suggest that antidepressants increase the risk of death by degrading the overall functioning of the body. This is suggested by the fact that antidepressants have adverse effects on every major process in the body regulated by serotonin. 12. Antidepressants have many negative effects on older people Most of the research on the adverse health effects of antidepressants has been conducted on older patients. Consequently, our conclusions are strongest for this age group. In addition to cognitive decline, stroke and death, antidepressant use in older people is associated with an increased risk of falling and bone fracture. Older people taking SSRIs are also at an increased risk of developing hyponatremia (low sodium in the blood plasma). This condition is characterized by nausea, headache, lethargy, muscle cramps and disorientation. In severe cases, hyponatremia can cause seizures, coma, respiratory arrest and death. The fact that most research has been conducted on older people does not mean that antidepressants do not have harmful effects on the young. As previously discussed, antidepressants can have harmful effects on development. Moreover, many people start taking these drugs when they are young and remain on them for years or decades. In principle, the negative effects of these drugs could be substantial over such long periods of time. Altogether, the evidence leads us to conclude that antidepressants generally do more harm than good as treatments for depression. On the benefit side, the drugs have a limited ability to reduce symptoms. On the cost side, there is a significant and unappreciated list of negative health effects because these drugs affect all the processes regulated by serotonin throughout the body. While the negative effects are unintended by the physician and the patient, they are perfectly expectable once you understand how these drugs work. Taken together, the evidence suggests that these drugs degrade the overall functioning of the body. It is difficult to argue that a drug that increases the risk of death is generally helping people. There may be conditions other than depression where antidepressants are generally beneficial (e.g., as treatments for brain tumors and facilitating recovery after a stroke), but further research in these areas is needed (see our article). Ethical and Legal Issues Physicians and other medical practitioners have an ethical obligation to avoid causing greater harm to their patients. The Latin phrase primum non nocere (“first, do no harm”) that all medical students are taught means that it may be better to do nothing than to risk causing a greater harm to a patient. Although all prescription medications have adverse side effects that can cause harm, practitioners have an ethical obligation to not prescribe medications that do more harm than good. The evidence we have reviewed suggests practitioners should exercise much greater caution in the prescription of antidepressants and to reconsider their use as a first line of treatment for depression. Additionally, we suggest that physicians and other medical practitioners should consider their potential legal liability. Legal liability for prescribing antidepressants Medical practitioners can be sued for prescribing antidepressant medications if doing so violates their state’s standard of care laws. In most states, the standard of care is what a “reasonably prudent” practitioner in the same or similar field would do. The standard of practice is not defined by what the majority of physicians do because it is possible for an entire field to be negligent. Since studies on the health risks associated with antidepressant use (e.g., stroke, death) have been published in well-respected medical journals, medical practitioners could possibly be vulnerable to malpractice lawsuits. For instance, it seems likely that a reasonably prudent physician should be aware of the medical literature and avoid prescribing medications that could increase the risk of stroke and death. Prescribers can also be held liable for not discussing information about medical risks so that patients can give informed consent for medical treatments and procedures. Prescribers have a duty to discuss the benefits and risks of any recommended treatment. Consequently, medical practitioners should discuss with their patients that antidepressant medication is only modestly more effective than placebo and could increase the risk of neurological damage, attentional impairments, gastrointestinal problems, sexual difficulties, abnormal bleeding, cognitive impairment, dementia, stroke, death, and the risk of relapse after discontinuation. Antidepressants must cause harm to create liability A medical malpractice lawsuit can only succeed if the antidepressant caused harm to the patient. It is important to realize that the antidepressant does not need to be the only cause of the harm—it only needs to contribute to or exacerbate the harm. As we have argued, antidepressants play a causal role in many adverse health outcomes because they disrupt serotonin, which regulates so many important processes throughout the body. This may make it particularly difficult for a medical practitioner to defend against a medical malpractice suit from a patient who experiences any of a number of adverse health effects while taking an antidepressant. For instance, if a patient has a stroke while taking an antidepressant, the evidence that antidepressants increase the risk of stroke suggests that the antidepressant may have contributed to the patient’s stroke, even if it was not the only cause. Conclusion The evidence now indicates that antidepressants are less effective and more toxic than commonly believed. From ethical, health, and legal perspectives, it seems prudent for individual practitioners and professional medical organizations to revise informed consent guidelines and reconsider the status of antidepressants in standards of care for many diagnoses and as the front line treatment for depression. With older people, for instance, the current data suggest informed consent must include a discussion of the increased risk of hemorrhagic stroke and even early death. We suspect that if prescribers realized they were placing themselves at legal risk for failing to discuss the adverse health effects of antidepressants with their patients, not only would they be more likely to discuss such information, they would be less likely to recommend these drugs in the first place. Paul W. Andrews is an assistant professor in the Department of Psychology, Neuroscience & Behaviour at McMaster University in Canada. He has a PhD in Biology from the University of New Mexico and a law degree from the University of Illinois at Urbana-Champaign. His work on the evolution of depression with J. Anderson Thomson, Jr. has been featured in the New York Times Sunday Magazine and Scientific American Mind. Taken with respect and gratitude. directly from ANNECWOODLEN’s Blog BEHIND THE LOCKED DOORS OF INPATIENTS PSYCHIATRY. http://behindthelockeddoors.wordpress.com/2014/01/12/you-and-your-antidepressant-2/
Do you work at a job and earn a living while you take anti-psychotic drugs? Do you support a family or take care of one while your wage-earner partner can keep her or his job without worrying about your sanity? Good, then the “anti-psychotic” pills you take (or I’ll add in for good measure, god help us all, the “anti-depressant” pills) are doing what we were always told they were supposed to do. Or if you don’t work or care for a family, if not, do you at least live a fulfilling single’s life, with good capable friends and family and a worthwhile occupying activity that keeps your mind free of craziness and despondency the preponderance of the time? Terrific!Then those pills, whether they be antipsychotic or anti-depressant pills actually function and you are one lucky dude or chick. I say to you, whoever you are, All Cheers and GO FOR IT! Please do not worry about anything further I say in this or any other blog post. Whatever I write from here on in, whatever I say that you do not agree with, IT IS NOT INTENDED FOR YOU. Why? Because by your report, YOUR PILLS WORK and they do a bloody good job of it. So who’s to tell you to change anything? You have no complaints and aside from the possibility that your brain might sustain a little shrinkage, if research about such things proves correct, you have nothing to worry about. In truth, most aging brains shrink and sustain bits of damage along the way. Lots of things can happen…most of them not drug related at all. One simply cannot worry about a “what if” future, when the present is so bright.
So I repeat, IF you happen to be one of those lucky ones I have described and actually have no complaints, IF, better than that, if you find that your anti-psychotic drug or anti-depressant pills work terrifically well, you have had no relapses, suffer no terrible trade-offs in terms of side effects, then stop reading this blog post right this minute. Why? Because I have nothing to offer you and nothing to say to you. Okay? You don’t need me, and you won’t want to hear what I am going to say to the others of us out there whose experience has been somewhat to radically different.
But this is a SHOUT OUT to you, there, who don’t like your drugs and don’t want to take them. Or find them minimally helpful, or wonder frankly whether they really do any of what the docs tell you they do, forewarned is forearmed…This post is going to be about the charade of anti-psychotic drugs, for the most part, about the fact that they do not in fact function in the anti-schizophrenia fashion that you have been told. (I likely won’t have the time or energy at this point, being on AP drugs myself, to get into the appalling farce of what are called anti-depressants…You could turn to MAD IN AMERICA by Robert Whitaker for a take on those — just check out his chapter on Prozac for a taste…) It isn’t that AP drugs do nothing at all. They do attack the brain’s neurotransmitter levels, in some fashion or another. And not just the vaunted dopamine and or serotonin levels either. No, most atypical antipsychotic drugs have effects on histamine, glutamine, noradrenaline and acetylcholine and likely a whole host of other brain chemicals we haven’t even scratched the surface of, in the sense of knowing their function in the brain, or in any part of the brain for that matter.
Do you know, did you know, that the Dopamine Hypothesis, the fundmental reason why there are antipsychotic drugs out there now in so many burgeoning numbers was always bogus? It never held water, ever. There was NEVER any reason to believe that dopamine caused schizophrenia, or that a dyspfucntional level of dopamine lay behind the majority of schizophrenic symptoms. It was a bold-faced and bald-pated lie, that’s because it is as old as the hills and as tiring. You don’t have schizophrenia the way one has diabetes, because you have a chemical imbalance in your neurotrnamitters that these neat little AP drugs resolve and rebalance. Sorry, folks, but that has been baloney ever since we all started developing parkinsonism and KNEW, just KNEW that something was terribly wrong with these miracle drugs that made us feel so terrible.
Did you know that it used to be the criteria for a true neuroleptic, the only way they knew they had a functioning adequate drug, was because it successfully induced parkinsonism in patients. That is, if it induced adequate BRAIN DAMAGE, then they knew it would “work” against schizophrenia. Because the theory was, both in ECT and insulin coma, as it was in early AP drugs like Thorazine and Haldol that you had to induce brain damage to get a therapeutic effect in the illness. Crazy no? No, not at all, not when you stood to make ZILLIONS and Gazilliions of dollars on these drugs. Not only could you treat a hospialized crazy person with these drugs, and make them “better” and push them out of the hospital, but you could set up a plan for future care, AFTER CARE, that specified that JUST like diabetes, a person had to keep taking these drugs. You never just recovered from an illness like schizophrenia, no. The drugs were miracles yes, but not like antibiotics, They never cured you. they just were a treatment that you had to keep taking. The Gift that keeps on giving…at least for the Pharmaceutical companies who dreamed up the protocol. If they could get a person onto the AP drugs, once, and mandate legally or via a persuasive mental health system that the patient stay on them for life, well then, what a system, and what a money maker!
Oh my eye! What a load of hog wash. All they ever did was dream up neuroleptic (“brain seizing”) drugs that physically subdued people and made them more amenable to nursing. So the hospital nurses could be more nursey nursey and kinder, and more kindly disposed to patients who were now drooling and dulled and seemed much genuinely sick, and the patients could be seen as more ill and less hostile and unpleasant to be around, less difficult to treat qua patients..
But it was a strange transformation, because the more sick the patients were made by taking these neuroleptic drugs, the less they were treated like the troubled and suffering PEOPLE they were to begin with. Once a patient, they assumed that role, and the whole cycle began and has never stopped to this day. “Schizophrenia is an illness just like diabetes.” That was the canard I was told in 1980 — we are still being handed the same disgusting lie! — when I was first officially diagnosed with the condition, or told the name to my face at any rate. “You’ll never recover, and you will likely have relapses, but you won’t be a back wards patient if you take these pills like a good girl, and do as I tell you. No schizophrenia isn’t a death sentence these days but it IS a life sentence…” So what did I do? I swallowed my 500mg of Melleril, yes i did, and I told the doctor I was feeling much better, yes I did. Because frankly I didn’t know how I felt and I felt OBLIGED to tell the doctor what he wanted to hear. How else was I going to get out of the hospital and get off those horrible pills that made me put on 20 pounds in three weeks and made me feel so dull and sluggish and tired all the time? Besides, how could I possibly, in those conditions, KNOW how I felt, when the nurses themsevlves colluded to tell me how much better I looked and was doing? I knew I couldn’t read or think for myself any longer. But they told me that that was my negative symptoms and had nothing to do with the drugs. It was a problem I would have to come to terms with by talking with a therapist…which was a good thing, that they suggested I see a therapist. Back in those days, it was often frowned upon that ANYONE with schizophrenia actually do any talking to anyone at all. After all, if you talked about yourself or your illness, you might upset yourself or the whole applecart…You might actually go crazy again, you were that UNSTABLE! No talk therapy was usually frowned upon for “schizophrenics.” It was seen as not good for them, and destabilizing. What we needed was daily meds and mouth checks and maybe day treatment with a hours job to do each day, like capping test tubes for the lab to keep us busy. Lucky was he or she who could function as a bus boy or table setter. Most of us barely made it to day treatment on time, before sacking out on a couch somewhere for a long snooze to let the morning’s dose of thorazine 1000mg or Melleril 800mg wear off a little before coffee hour or lunch time.
Some of us actually turned blue on high doses of Chlorpromazine, and she eventually died, at the age of 28. There was a lot of relapses and some suicides, but NO ONE actually went out and got a job and quit the hospital and got better. No, because the whole damned system was set up in such a way that once you were set up on anti-psychotic drugs, with a diagnosis of schizophrenia, you were put on social security disability payments for life,..and drugs for life followed, and the trap ensued that meant your whole life was a rolling down hill of poverty and more drug taking and relapses…until maybe something amazing happened to get you out of the systematic rut the psychiatric system had placed you in.
MAYBE you found someone you fell in love with, someone who not only would take care of you, but who hated to see you dull and passionless and sexless on the drugs and encouraged you to SLOWLY wean yourself off of them. And maybe it happened to a few of us that it was a success, because love can really conquer all, even the notion that schizophrenia is a life-long hopeless illness. If you got off the drugs in the right way, slowly, and stopped seeing the doctor who told you you would definitely relapse, maybe just maybe you didn’t. Maybe your sex life came back and you found out it was better than Haldol and thorazine, and better than being dulled by the system’s poverty and being sick. And once in a while that person’s husband was so loving and encouraging that they got married and moved away and she stayed well enough to take up a hobby that turned out to make a little money by itself. So she turned it into a business, and miracle of miracles, she didn’t fall into the trap of SSDI after all but stayed well without the AP drugs and became a businesswoman without enough time to think about being schizophrenic again…
But alas, that didn’t happen very often. Not nearly often enough. There were far too many tragedies compared to the rare success story. Too many people getting diagnosed with schizopohrenia, and then when the fads for multiple personality disorder came, with that, and all the other fads that had to happen because the drug companies had drugs that they needed to sell use on people and they had to have diagnosese to fit the pharmaceutical picture so they could sell the drugs they had on hand. ADHD, autism are only the latest two…
But I digress, I digress, so let me tell me my own story, if I have the time and energy.
I got sucked in. I did. I was hospitalized in 1980, and even before them. But in 1980, as far as I can now recall, I was up late at night, for the third night, in the hospital kitchenette in an absolute sweating panic about my hands. Why? Because I had this strong delusional belief that they were not my own, but that my twin sister had taken them over and controlled them. I could feel them, and in a sense I could see this process happening. And I heard voices telling me that I was in danger. A nurse came in, and asked me why I was up, and in a panic, i told her. I said, somethings wrong with my hands! They aren’t mind, my sister has control of them! And I can’t sleep, I can’t sleep!
Now, the nurse was a kind woman and I think she meant to help, but she couldnt do anything for me but tell me she would call the doctor, who came, in his fashion, running. I was sweating bullets by then, sitting at the empty lunch table, mumbling about my sister and my stolen hands. What could he do, given his own pharma-company training, but offer me some drug assistance and promise me that it would help, that it was what I “needed” in the throes of my illness?
I believed him, I did. And when he came back the next morning, after I had been dosed three times that night with increasing amounts of Melleril until I finally slept, he pronounced that I suffered from the mental version of diabetes. schizophrenia…The rest, well, if it isn’t everyone’s history, it is a version of it. And it involves SSDI and even SSI because I had never been able to work a full time job even before then. And none of the many drugs I took after that ever did anything for me but disable me more than before. And I would stop them and be hospitalized again with what they now suspect is withdrawal psychosis, or could have been. And I would be started back on the drugs, or a long-acting injection that was supposed to prevent hospitalization. It never did much good…I was a basket case, a basket case. I never washed or changed my clothing, or even took off my shoes, not even to go to bed. NO I wore those hiking boots for a good year and a half before they even saw me take off the socks I wore underneath them…
So how much did the AP drugs help me? And when they started to restrain me for paranoid fears and trying to escape a locked unit, did I then say Enough is enough, you cannot torture me, I have schizophrenia? No, I accepted mechanical restraints for three days at a ttime as a form of treatment. One doctor actually told me that schizophrenics don’t respond badly to being tied to a bed for a long time, it helps them, he said, by reducing stimulation…So they did that, and they kept me in seclusion for weeks at a time…until finally I would cry Uncle and take the drug they wanted me on, and go home again, prepared for the next certain relapse, because what else was there….I had a life, yes, but it wasn’t much. It was just hospitals and restraints and drugs that never helped me and cruelty from nurses that didn’t know they were hurting me. And doctors who were damaging me without thinking twice about it. And I didn’t even have the mental wherewithal to know that the drugs were the prime offenders. The PRIME offenders.
It is now 5:30am and I have been up all night. My shoulder hurts, from where i have a slightly torn rotator cuff and frozen shoulder tendonitis… I don’t have a bed, only a recliner I should not sleep in…I am a mess, and I am also NOT going to continue to take my Abilify and Geodon much longer…I cannot. I cannot. I do not know what will happen, but I am too afraid of what will happen if I take it, to take them, though I have never felt they did me more harm than good. I just don;t know what real GOOD they do me.
More later, or on another day. Sorry this was so impassioned.
TAKE THESE BROKEN WINGS…
This is an incredible video, which, though long, is well worth watching. For anyone who believes that recovery without medications is impossible or not likely, you should watch this with at least half an open mind. And for anyone who has given up hope, this should give you a lot of hope. I usually cannot watch entire videos half this long, but I watched this one all the way through, even though I admit I had to take breaks because (Yes, I take meds myself) my attention span is short…But it was worth it to learn that one of the women featured not only recovered from her severe schizophrenia without taking psychiatric medication, she remained absolutely psychosis free and became a psychiatric nurse for 30 years. What I would give to speak to her about the sorts of treatment, or abuse that passes for treatment here in CT! But be that as it may, do watch this if you can. It is absolutely astonishing. And beautiful too.
I am uploading my new PAD, IN ORDER TO AVOID INJURIES SUCH AS THESE, brought on in Jan 2013 at Hartford Hospital’s Institute of Living. and photographed the very day I was released.



Although I brought the PAD both to the Institute of Living in Jan 2013 and to Yale in Aug 2013, I don’t know what happened that it was abrogated so deeply and so widely. At Yale, they forced medication on me, holding me down three times daily at times, resulting in such psychic regression that as you have all read, I routinely stripped naked, defecated on the floor and smeared feces all over the wall. That I was at one and the same time attempting to communicate with these people, by WRITING WORDS IN MY SHIT, was utterly disregarded by all at the time. But I assure you that if I was regressed and psychotic in doing such things, I was nevertheless still verbal! I am also virtually certain that had they not grabbed me, pinned me to the floor and held me down for three painful injections in the buttocks of a drug that Soviet dissidents have long called pure torture (Haldol in the 60s/70s was the subject of many a televised congressional hearing, and discussed in just such terms…) my response would have been very very diffferent indeed.
That said, they did what they claimed they had to do, and when I left, I left feeling absolutely convinced that my life was and had been mortally threatened, that I could NEVER return, that I would literally be murdered if ever I dared. Nothing more need be said about such sadistic places as the Institute of Living at Hartford Hospital. Even in the Patient Care Guide and Journal, they are at pains to make it clear that any loud or out of control behavior will be dealt with swiftly and severely, with seclusion, restraints, and even charges pressed by the local authorities! (NO attempts to soothe the traumatized patient or act on what CMS has urged be the best practices of trauma-informed and patient-centered-care at the IOL. No, at Hartford Hospital, it is all about NO SWEARING and staying quiet, non-disruptive. The “Or else” threat behind it all is not even implied but openly stated in their rules and obligations section. Why ANYONE would want to set themselves up for treatment in such a place is beyond me…They have even edited out any attempts at kindness from the old handbook that I was given just a year ago. Yale at least attempted to live up to a policy of Trauma-informed and Patient-centered care. When they said No Restraints policy, I believe they meant it, at least in terms of NO MECHANICAL leather and shackles restraints.
And I believe that had Robert Ostroff MD, NOT been in charge of my care during the week or two that Robert Milstein MD was away, some of the brutality might not have occurred at Yale and I might be writing less devastated things about the Washington Square 2 unit, a place I had once so hopefully described as a “soft, gentle place to land in a psychiatric crisis.” But as much as because of my outrageous and disruptive behavior in response to their trauma as because of their repetitive violence and cruelty, I can never return there…a sad thing I suppose, since there is literally no safe place in Connecticut for me.* *more on this later or in another post. What I have posted here is an update in order to Keep me OUT of the hospital as much as to direct my care if I am put inside, It is not the whole thing, only the first two or three pages, I would be happy to upload the whole thing so you can see how I did it, if anyone indicates interest. Let me know. So far it was always the first three pages that got people’s attention. ______________________________________________________
Miss Wagner has experienced multiple episodes of severe psychological and physical trauma, including date rape, the suicide of two friends, and domestic abuse by caregivers. She should NOT be subjected to restraints, involuntary seclusion, or forced medication. The use of these inevitably leads to re-traumatizing and injury, regression and severe worsening of her psychiatric symptoms.
*I cannot reiterate enough that if you utilize 4-point restraints or seclusion, it is virtually guaranteed that you will see regression, increased hostility and aggressiveness as a result. Please don’t do something everyone will regret.
ADDITIONAL STATEMENT TO CAREGIVERS (PLEASE READ)
It is important that you understand that I do not have a personality disorder (you can confirm this with Dr Angela C——, or any of my longtime outpatient providers and friends and family members). If my behavior/emotions seem out of control, it is because I am out of control – temporarily.
I have had tertiary CNS Lyme disease, which I was informed after multiple positive PCR and Western Blots during treatment was likely incurable. During my initial illness, my brain developed MRI lesions which may predispose me to temporary emotional and behavioral abnormalities but these are NOT my norm. Anyone who knows me well would tell you that, if you ask them.
I am not always able to communicate my fear but because I feel so threatened and unable to communicate clearly about it (lest there be consequences to me) I may become very angry at the hospital situation. I am not an angry person, but I do have trauma issues, as many people do.
Please be aware that I am sometimes mute, in frustration and overwhelmed by circumstances. You can provide me with a pad and pen to facilitate communication, but berating me into speaking will no purpose and may only precipitate anger.
Ascertain from me whether the information you have at hand is correct. Too many records and hospital charts have been drawn up on faulty information from earlier charts or information gleaned from others but not from me, and the consequences to my treatment have been devastating.
I would prefer NOT to take any medications and will resist them. I want to experience my LIFE AND MY FEELINGS. If you insist on meds, the ones that work best are _______.
I will not take any drug that induces weight gain. If you force it, know that I will fight you, tooth and nail.
April 16, 2014
Dear Harold Schwartz, Director of the Institute of Living at Hartford Hospital
I believe that I was profoundly harmed by the treatment I received in 2013 on Donnelly 2 South at the Institute of Living at Hartford Hospital, and that what the staff did to me was not only unethical and cruel but that it crossed the line into illegality from the very first. Psychiatric patient abuse is a pattern in Connecticut hospitals, but it was most egregious at the Institute of Living because the staff told me that they knew what they were doing was wrong but that they would get away with it anyway.
That I know I was a difficult patient never justified staff behavior towards me. I was loud and upset and hard for them to deal with, yes. That is precisely why my Psychiatric Advance Directive (PAD) was written out the way it was, and why I made my medical and psychiatric history online so available. When ill, I am frightened and paranoid, which makes me easily roused to irritability and hostility. I know this, from a distance as it were. But knowing this now does not mean I was in control of my emotions. I am by nature neither temperamental nor prone to temper eruptions or throwing things. In addition, I am extremely modest, hardly one to disrobe or urinate in public. My friends and family have at times variously labeled me “stoic” and “peacemaker,” which should tell you a lot. But that I disrobed and urinated on the floor on Donnelly 2 South both horrifies me and concerns me because these behaviors point to something going on distinct from my psychosis: they point to my having been subject to abuse and trauma at the hospital itself.
Let me make it very clear that if I have behaved in such ways before it was only in response to similar extreme circumstances – as when i was subjected over and over to restraints and seclusion in a horrific and sadistic fashion at Manchester Hospital in 2009 and similarly at Middlesex Hospital in 2010. It is too bad that when Sanjay Banerjee MD and Amy Taylor MD took it upon themselves to violate my HIPAA privacy rights and investigate my previous admissions, without my permission (which I expressly refused to grant) they failed to make the connection between the abuse, and my subsequent behaviors…It turns out all they drew as a conclusion was that if those hospitals could use restraints and seclusion ad libitum, so could they. It didn’t seem to matter to Dr Taylor in particular that in 2009 and 2010 measures such as seclusion and restraints not only didn’t work, they made things worse. Not surprisingly, when Dr Taylor followed these examples I regressed completely, just as my PAD predicted.
I was admitted to Donnelly 2 South, and I came in with a very detailed Psychiatric Advanced Directive as I said. I made it very clear that my online electronic medical record was also available. It included documents such as my narcolepsy diagnostic consult and special documentation assessing my need for a higher than usual dosage of Ritalin, written by my former sleep specialist, Mary B O’Malley, MD PHD who was also my psychiatrist from 2000-2009. Included as well was a letter she wrote to my present psychiatrist, Dr Angela Cappiello, explicitly stating her conviction that I do not have a personality disorder, NOS, borderline traits, or otherwise.
According to Dr. Sanjay Banerjee he read every page of these documents. That is what he told me. He even praised me, saying he wished every patient would come so prepared. Moreover, when he spoke with Dr. Cappiello, he brushed off my concerns about anyone misperceiving me as having a personality disorder. My brother, Philip Spiro, MD, himself a psychiatrist, brought up the same matter when in discussion with Laurie Denenberg, LCSW, but her response was much the same: “Personality disorders are not a part of the picture here. We intend to honor her PAD. We are glad that she has had the foresight to prepare such a document.”
If this was so, then how did it come to pass that Amy Taylor, MD wrote on my history and discharge summary that I have a “long history of Borderline personality disorder” and herself diagnosed “Personality disorder NOS with borderline traits”? I was being treated for four weeks for an active psychotic disorder Axis 1. In any event, she could have no way of knowing whether or not I had a personality disorder, given an active an Axis I diagnosis.
On or around February 4, 2013, I walked in frustration away from the quiet room where I had been held captive for nearly three weeks, strolled down the hall, looked out the window and slowly retraced my steps back to the quiet room, which I had been expressly told was NOT a seclusion room (the definition at Hartford Hospital’s Institute of Living of a seclusion room is a “room to which the door is locked.”) But when I arrived I was confronted by a cohort of staff who proceeded to 4-point restrain me to the bed, even though I was quiet and put up no resistance. Not wanting to give them any reason or justification, I passively lay down on the bed and placed my own limbs out for the restraint cuffs, saying, (I quote my journal entry made later that evening): “For shame. You ought to be ashamed of yourselves. I am not and never was a danger to myself or others.” Their response was “ You refuse to follow directions so we do not know what you will do. This is not punishment, Pamela, this is what your behavior brings on every time.”
From that point on, the threshold for restraints was extremely low. They always restrained me, spread-eagled, so tightly I couldn’t move a muscle. They never permitted bathroom breaks or even used a bedpan, instead they made me defecate in my clothing. They never even let my hands free to eat. I would fall asleep rapidly after three routine punishment needles in the buttocks: Haldol, Ativan and Benadryl—whether I just had my regular meds or not, and they would invent reasons to maintain me in restraints even after I had been asleep for hours. When I woke, groggy and hardly dangerous to anyone, they would grill me with questions that I could not answer. They would then use my inability to respond as reason not to let me out, even when I asked, as the chart recorded, in a “soft sedated voice” for release. They would re-inject me, to put me back to sleep instead.
In the evening on Jan 5th, for the second time that day, they brutally restrained me for throwing half a graham cracker at the wall. Then, as usual, they left me like that for six hours, even after I fell asleep. But in point of fact, though, I could never earn my way to release from restraints by good behavior or quietly, calmly asking for release. I had never done anything to earn my way into them in the first place. I was never violent until they threatened me. They refused to release me until I literally cried, “Uncle” when they told me to.
As to those vaunted “shows of force” what did they expect? Presented with a cohort of threatening staff personnel I saw one thing: an impending assault. I know they anticipated my panic; they said as much in my chart. Isn’t that the point of a planned “show of force” – to induce fear and panic? Why else do it? So why should it be any surprise, when I defended myself when they forcibly, physically grabbed me? When they stuffed me into a body bag and were trying to tighten the straps, surely you can understand why anyone would bite the hand of an attacker whose digits came near the face. I had done nothing but refuse to enter the body bag willingly. I simply was passive. I did not fight or resist until they grabbed my body and assaulted me.
But none of it should have happened. My Advanced Directive explained in exquisite detail exactly what to do and what I respond to better than fear tactics and force. In fact, It is beyond me, knowing that one of the admission diagnoses I came in with was PTSD, how anyone could possibly approve in advance, permission to use restraints and seclusion “just in case they are needed”. Why not counsel the person asking for this advance “right to restrain” to do all in his power not to restrain me and to work with the PAD instead?
Here’s what SAMHSA the substance abuse and mental health services administration publication has to say on seclusion and trauma:
“Studies suggest that restraints and seclusion can be harmful and is often re-traumatizing for an individual who has suffered previous trauma…
“Further, there is a common misconception that seclusion and restraint are used only when absolutely necessary as crisis response techniques. In fact, seclusion and restraint are most commonly used to address loud, disruptive, noncompliant behavior and generally originate from a power struggle between consumer and staff. The decision to apply seclusion or restraint techniques is often arbitrary, idiosyncratic, and generally avoidable.
“Moreover, some studies indicate that seclusion and restraint use leads to an increase in the behaviors that staff members are attempting to control or eliminate.
I have been traumatized, and not just by hospitals. I was date-raped three times in my twenties and experienced traumatic domestic abuse by a long-term roommate. The cover sheet on the PAD made very clear that due to these trauma issues, I could not tolerate being secluded or restrained without serious consequences: regression and serious worsening of symptoms. Unfortunately, as soon as the staff saw fit to use physical methods of coercion and control on me from the first time a staff member grabbed me and pushed me with his lower torso, I ceased improving, and my symptoms went downhill. Did they really think they were being kind and compassionate?
Staff violence begets violence….
I tried to get help even when on the unit, at least I tried when I was free to, to make calls or leave my seclusion… that is to say, forced three -week-long stay in the quiet room last winter. I made many calls to the hospital’s patient advocate office, but the sole time anyone made contact was when the advocate came to hand me some paperwork – I believe I was actually in 4-point restraints at the time — papers I could not read about the forced medication hearing. I needed her advocacy, but she never responded to my panicked calls in any way that was helpful to me. I wanted her help, but she never came by to ask me what I needed. She was less than useful, the fact that I had to go through her, essentially a hospital employee, and her refusal to respond, contributed to my ongoing panic and desperate feelings of aloneness and depression. No wonder Dr. Sanjay Banerjee attempted to force ECT on me, without any prior discussion of it with me whatsoever.
And where did the ECT discussion come from? My PAD states in no uncertain terms that I will refuse ECT under any and every circumstance. My brother would be my conservator if Banerjee had sought to go down that road, and he would never have made any decision to counter my wishes on that subject. If Banerjee really read my PAD, he would have known that. I have already had FORCED ECT and it traumatized me terribly. Also it failed to work.
Banerjee had stopped my 75mg of the antidepressant Zoloft during the first or second week I was there. “Do you really need that?” he had asked, “You don’t seem depressed to me.” Obedient, and in any event glad to get off any medication at any time, I shook my head, assenting to the change. A week later, instead of reinstating the Zoloft, Banerjee blamed my sudden “depression” on my refusal of the anti-seizure medication, Lamictal, a drug I had not taken in 6 months. Now he was applying to force me to take ECT, something I was terrified of, and to have calculated brain damageIt was this threat, and the brutality with which the decision was handed down, that started the downhill course of my IOL stay.
The very next weekday, all hell broke loose. When I entered the conference room, I pushed some important notes across the table that I wanted Dr Banerjee and Laurie Dennenberg to read. They refused, claiming that I threw the papers at them. Instead, Dr Banerjee proceeded to berate me, and told me how he had consulted with other hospitals and providers and had read my records against my instructions and Advance Directive, thus violating my HIPAA rights. Moreover, he threatened me with a behavioral treatment plan that would not permit me to do art or writing unless I “behaved.”
I hit the roof, telling him I would sue the hospital and complain to JCAHO, then summarily left, slamming the door, an act that stemmed from feelings of utter impotence, because I couldn’t actually say in words anything more effective.
It could have ended there. I could have been left alone, to cool down and calm myself. But, no, Dr Banerjee had to write for stat meds again, and even though I was on the phone and trying to find someone to talk to, to calm myself, I had to be physically dragged off the chair I sat on, away from the phone and brought to the floor in a physical struggle (because they had attacked first, i.e. physically grabbed me, I defended myself, instinctually). They could have waited for me to finish the call. They could have waited to see if I calmed myself. I was not hurting anyone or even threatening anyone or myself with harm. All that I had done, in terms of physical threats, was to throw a lightweight chair at the wall. And that, it was clear to everyone, was intended not as a threat to anyone. Furthermore, it was done and over with. I had left that area and gone to my room. I had then come back and now sat on the chair by the phone, speaking to my interlocutor on the other end. There was no need to pick a fight or encourage a struggle. A wait-and-see policy could have successfully guided the situation to a better resolution not only for the situation at hand but for the entire hospital stay. As the poem by Dylan Thomas goes: “After the first death, there is other.” Once they decided to use four—point restraints, there was no going back. The first time broke everything, So they used them again, and again, and more and more freely and without justification but for convenience and punishment.
Back to Feb 5 or 6, after sleeping for six hours, I was taken out of restraints conveniently just in time for a visit from Dr. Angela Cappiello, my outside psychiatrist. Observed by my 1:1 monitor, I only dared whisper and dared not tell the doctor the full extent of the abuse that had been happening. Nevertheless, she took one look at Amy Taylor MD’s behavioral treatment plan posted on my wall, and told me that it would be impossible for anyone, even someone who was well, to follow it properly. She was so worried about me, and about my ability to complete the treatment plan’s requirements, even for the required “24 hours,” that she intervened. The next day, the single day that Dr. Taylor planned to be out of town, Dr. Cappiello asked Dr. Mehendru to evaluate me for discharge, telling her that she feared a power struggle had been set up that I could never win.
When Dr. Mehendru came to see me, at first I was angry, as the chart indicates, thinking she was just another Taylor flunky, preparing to use more restraints and seclusion, But when she asked if I would like to go home, I took one look at her, saw sincerity in her eyes, and burst into a smile, ready to say yes to anything. Miraculously “cured,” I left the IOL that very same day, less than 12 hours after being released from 4-point restraints and not 4 hours out of seclusion.
However, I was not well. Within two weeks time, I was back in the hospital, this time admitted to Yale New Haven Psychiatric Hospital, via their emergency room. Over the next 3 weeks I experienced an entirely different kind of care. At Yale I did not find a staff ready to fight or try to seclude or restrain me.
I was still the same person with the same problems, loud and angry at times, even “violent” to property in my frustration, and still psychotic, yet they never responded with a show of force. Why would they? At Yale it would be absolutely anathema to deliberately frighten a patient. What would be the purpose in that, they would think. They also never pushed me into a seclusion room or strapped me down in punitive 4-point restraints, or any of the other ill-advised responses that my PAD explains are the worst things to do to anyone who is struggling, scared and paranoid. In point of fact, Yale Psychiatric Hospital’s Washington Square unit does not have a seclusion room. They also have a “restraints-free” policy, so they didn’t use those at all either.
The Institute of Living on the other hand with its “We only use restraints and seclusion if we have to” policy, restrained me countless times, and for many more hours than was even legal. When I woke up that last morning, the room opposite me was occupied by yet another person in 4-point restraints! That is because once you allow staff to use restraints a little, it only takes a little to use them a lot. And once you sanction the use of restraints and seclusion at all, it is only time before someone abuses them and abuse becomes the norm.
I would like your response to this letter, I have sent it to many people within the state government and outside of it, But you may have the first response. Also you may be interested in the youtube video of my artwork which can be found at this site:
Prior to when you allowed the staff to body bag and restrain me, when I had done nothing wrong but leave the non seclusion quiet room, and you refused to come to my assistance, you had asked to see my artwork. Instead you left me to be tortured. Well, here is some of the art you might have seen had you rescued me from my abusers.:
Sincerely
Pamela Spiro Wagner
The final one you never saw in featured in the post below this one.
This time you should be able to view this on an Iphone or Ipad.
I have been diagnosed with schizophrenia for nearly forty years and was forcibly medicated and involuntarily hospitalized many times over those decades. Ordering me to take an “anti-psychotic” medication and then physically compelling me to submit to IM injections never got me to a point where I saw the “error of my ways” much less helped me to recover. How can that be? Take my 3-week stay at Yale New Haven Psychiatric Hospital in the summer of 2013. Because I refused the prescribed Zyprexa, I was repeatedly held down and forcibly injected with IM Haldol, a so-called first-generation “anti-psychotic.” Call Haldol an antipsychotic if you will or be honest and just call it a behavioral management drug, it subdued me, yes, it did indeed. It stupefied me. And in the end I cried “Uncle.” But before I surrendered and submitted to their demands, I only got worse, regressing to a degree so pathetic I find it hard to believe it now. But that this happened was a connection the doctors and staff never made,, not even when after I was forcibly injected, I would strip, defecate and write on the wall with my feces.
It seems obvious, at least from my experiences, long and manifold, that involuntary treatment does not work, at least not the way people think it will or should. Over the short run, you can indeed make a person take medication (which is what this is all about in the end, drugs, not something like psychotherapy being forced on anyone…). You can threaten a person with hospitalization “or else,” and frighten her into swallowing pills. And if she does refuse, you can hospitalize someone for refusing and medicate her against will just as you do now to certain in-patients.
You can, if coercion is your game, put certain involuntary in-patients into 4-point restraints, pretending that her very resistance makes her a danger to others, punishing her for fighting the team that holds her down. You can even inject her with so-called “depot” drugs that once in the system continue to work for as long as a month.
Clearly, people break, faced with threats and coercion and many eventually come to accept treatment “voluntarily,” at least for a time. They may even appear to “get better”. Nevertheless this sort of improvement is often shaky at best.
Involuntary — forced — treatment is the worst possible thing you can do to a person with a serious psychiatric condition, especially schizophrenia. Symptom improvement will likely be temporary, even with medication “on board.” I have yet to meet anyone who actually gained that magical “insight” via coerced medication… And given the side effects of all the known drugs, very few people who are not voluntarily in the system consent to take them for long — for good reason.
Moreover, as recent research has shown, there is every reason to suspect that psychoactive drugs, especially the so-called antipsychotic drugs, are far less efficacious in promoting real and permanent recovery than we have been told. However, the effects of trauma and the aftermath of involuntary treatment can be disabling, even permanent. I know; I have been there. As a result of my experiences with forced treatment I now suffer from PTSD in addition to the diagnosis of schizophrenia.
Although at present I choose to attend outpatient treatment, I do not always comply with taking medication, especially when it make me feel bad. I won’t even take meds that others claim alleviate my symptoms. If a drug makes me feel horrible inside, I assert the right to refuse it. Sometimes treatment can be worse than the disease. Alas, because of this, I have, while in-patient, all too frequently been subjected to forced medication hearings, hearings which I believe I was pre-determined to lose, the deck being stacked against me.
At the former Hospital of St Raphael’s in New Haven in 2004, I was not only forced to take the atypical antipsychotic drug Zyprexa, despite the fact that the medication had caused me to gain 60 pounds, elevated my cholesterol and triglycerides sky-high, and made me pre-diabetic. The probate judge, on the instigation of my in-patient psychiatrist, also ordered that I undergo involuntary ECT otherwise known as electro-shock treatments. I was so terrified of the side effects and the real brain damage ECT was inflicting on me, that I literally awoke,mornings, with excrement in my underwear.
In the more recent past, my experience at Manchester Memorial Hospital ECHN in Manchester, CT was just as horrendous. This, along with an equally brutal experience, at Middlesex Hospital in Middletown, Connecticut 6 months later combined to such trauma that I was diagnosed with the additional problem of PTSD. As recently as the winter of 2013, at Hartford Hospital’s Institute of Living, I was threatened with forced ECT, kept in seclusion for three weeks and restrained for nearly twenty hours multiple times. Why? Because as the record states, I was unpredictable and “did not follow directions.”
I would like to tell you about the Manchester Hospital experience in a little detail, as I believe it will give you a “taste” of where IOC, when taken to its logical conclusion, can and will lead.
I was admitted there on a 15-day physician’s emergency certificate (PEC), and the attending, a certain Dr Benjamin Zigun, summarily took me off the two-antipsychotic drug combination, plus an anti-seizure medication and the anti-depressant I had come in on. This drug “cocktail” had worked for me since 2007 without distressing side effects. I was not only willing to take it but I felt it helped me function better than I had in years. But the psychiatrist at Manchester Hospital decided, and I quote, “since you are here, by definition your current meds aren’t working. I will put you on something else.” Did it matter to him that I had already been tried on nearly every other drug on the market, old and new, and none worked as well and with as few side effects as the Abilify/Geodon combination I was then taking? No, he was the doctor and the doctor’s decree was law.
As a result of his ministrations, the “offending meds” were removed and I was again ordered to take Zyprexa, despite its known and severe side effects. Over the next few days, I continued to refuse it. Naturally, having been abruptly withdrawn from all my usual medications, I began to decompensate further, having nothing in my system. A forced medication hearing was held. For some reason, Dr Zigun decided I would not be given Zyprexa after all, but one of the oldest neuroleptics in the PDR, Trilafon. When I objected, he said only that if I refused even a single dose, I would be injected in the buttocks with 5mg Haldol.
All too familiar with Trilafon’s side effects — from akathisia’s maddening restlessness to a constant fine tremor in my fingers, I refused to swallow the pills. But neither would I willingly lie down to take a needle full of “vitamin H,” Haldol being a drug just as awful as Trilafon if not worse. So I resisted, physically, when it came to the nursing staff grabbing me and pinning me to the floor. I fought them when they so much as approached me with the punishment hypodermic.
At first, they just overpowered me, injected me and walked away. But after a few such tussles they started calling “a code” to bring in the goon squad. I do not know how many times this happened but the goon squad consisted of several people including uniformed security guards . Without a pause, they would barge into the room, assault, restrain and inject me, despite my terrified screams.
This sort of violent encounter happened so many times, along with predictable and regular use of 4-point restraints and/or solitary confinement, where I would be locked in their dark, cold seclusion room, that I literally lost track of time. Indeed, but for whatever I managed to record in my journal after each episode, and from their single-viewpoint one-sided hospital chart, I would have no idea what happened during most of that entire three week period at Manchester Hospital, though from my bodily reaction when thinking about it, I know something very bad happened.
Why do I tell you this? Because this sort of aggression, even torture is what forced medication and involuntary treatment lead to much more often than you may want to believe.
If H.R. 4302 passes in the Senate and expanded IOC is instituted in the states where it is now allowed, how precisely do people intend to treat a person with a “mental illness” who does not to want treatment? If a person refuses to leave her apartment to be hospitalized, and is able bodied and physically strong, do they propose to assault, even Taser her, though innocent of a crime? Once she is unconscious and no longer able to resist, do they then intend to hospitalize her against her will so that she can be forcibly medicated, with the threat of 4-point restraints as a back-up if she continues to resist. Or perhaps they expect that trauma itself to scare any individual into compliance?
I am not against all psychiatric treatment. I am definitely not against all psychiatric residential treatment facilities ( including hospital psych units…) But we have curtailed the availability of in-patient beds at present to our detriment, even as we have allowed drug company research scientists and providers to focus almost to the point of tunnel vision on the medical model. This has brought us right to this notion that if we institute IOC, and can force a given individual to take medication, we will be working on a problem that has a real and objectively verified solution. In point of fact, however, there is absolutely no proof that antipsychotic drugs lower violence on the streets or have any effect at all on the incidence of violent crime. That said, if a national IOC law mandated forced treatment, and hospitalization, where are the psychiatric beds to follow through on that mandate? Downsized, in most states to ghosts of their former abundance.
If this is what supporters of H.R, 4302 anticipate and believe in: IM injections, four-point restraints and all, then I must ask: When will you learn that you cannot treat anyone with violence and expect the outcome to be a desirable one? What you propose to do is to subject persons with psychiatric disorders to more trauma and violence than ever. You want to expose them to a“treatment” that is just euphemism for brutality.
I fought back, tooth and nail, biting and clawing the goon squads that descended upon me and attacked me, intending to shackle me by the wrists and ankles to a bed, because as they told me, “ I didn’t follow directions. Yes, I resisted. Who would not have? I was terrified. What did they expect me to do, politely thank them?
This sort of coercion and cruelty masquerading as care doesn’t help anyone get better, it only chases them the heck out of Dodge and as far away from “treatment” as they can get. Oddly enough, little do “Escapees” from treatment such as these know that they might be the lucky ones. As longitudinal studies of treated and untreated individuals with schizophrenia are coming to light, it has become apparent –even Thomas Insel, head of the NIMH admitted this on his blog — that treating – medicating — schizophrenia long-term has had unintended consequences, one of which has been to inhibit complete recovery. By contrast, those persons who walked out or were forced out of treatment, “back wards patients,” seemingly hopeless — it turns out that these people to a much greater degree than those who stayed in the system, recovered on their own, without help, largely by stopping their medications.
A majority of these “lost souls” found themselves only after they ceased taking medication and ceased consuming mental health services. Because they became wage-earning, productive citizens and not mental health service users, many are now “lost” to the mental health system. To experience so few symptoms as to be unknown the to provider community despite past illness, surely this must be accounted the best of all possible outcomes.
IOC works — or doesn’t work — according to a medical model that imposes medication on the unwilling, with no end point, insisting that mental illness is no different from diabetes. But as Dr Insel has admitted, this is not true and apparently never was. New models are needed. Violence is no solution, nor does it cure anyone to impose treatments of dubious value and great harm on those who are different from some mythical “norm. ”
(I sent a version of this to Connecticut’s Senator Blumenthal and several other people, including the New York Times, without response, so I am posting it here for public consumption and comment.)
Trying again…
Still not playable on ipads or iphones, not sure why. I think the sound will work. for what its worth…
Youtube video with sound available for all devices here:
No music or sound, sorry. Best viewed in small screen as the conversion to Quick-time made the files smaller and hence less crisp when seen on a large screen…I’m sorry but this doesn’t seem to be viewable on an ipad..Dunno about android devices. At least I notice that the controls are unavailable on my ipad at any rate…Will try to find another format that will work and re do it…SO SORRY!
Youtube video with sound here :
Continued from yesterday:
Ah, what was Hope always saying? Life is a beach? He hadn’t quite understood her before, but now he did and it surely was. Life is a beach. But it isn’t any pure coral white beach, with sunny skies and clear azure waves. It’s just an old beach of a beach and then you die.
Fuck.
Prem rarely used profanity, so when he thought this word, it appeared in his mind separated out, as if in a paragraph of its own, highlighted, in bold.
Fuck.
What was the point in living if you were only going to die, ignominiously, and end up with your toe tagged in the morgue like any television corpse. It hardly seemed worth it. What was he doing, why did he bother worrying about all these people in Building 22, who were just going to die and end up tagged at the toe themselves? How was it worth it, trying to hold the building together that was trying to fall apart after a hundred years of being mortared and bricked into existence? And how worth it was it anyway, just to upkeep a community of twelve individuals who many of them had rarely-to-never paid a cent into society, but only drew from it like the proverbial parasites that some, like Martin the skinhead, called them.
Martin had hardly a peg-leg to tap out that tune with, however, being something of “parasite” himself, Prem observed. But being copper had never stopped one saucepan from calling another tarnished, not in Prem’s experience. And just why hadn’t the disabled paid into society? Had any of them ever tried to get off disability? Was it their fault? Or was it the fault of a society that encouraged, even forced permanent disabled status on them, and with it concomitant poverty? Who could get out of the disability snare once caught in it? No one who had lived in Building 22 had ever, so far as Prem knew, outgrown or out-earned disability. In fact, the residents were forever finagling ways to earn just up to, but not beyond the strict earning limits placed on them, just so they could maintain disability and their subsidies and their small but stable incomes.
What a miserable trap. You could get a regular but miserably small income for life, if you agreed to be disabled by the system. But in order to get out of the trap, in order to try to earn a living and make your own way, you would in a stroke lose both the place you lived and your regular income, all for a life of insecurity and instability. And this at a time when nothing was secure or stable except the fact that there was no safety net, and no one cared about people in need except a handful of overused charities and churches. So who could blame a disabled person for deciding not to even try to work but to stay on disability and remain impoverished? Who could blame them when that meant at a minimum a roof over their heads and food on the table. It was a devil’s bargain, but Prem could see how sometimes the devil could appear a better partner than the faceless ghoul of potential homelessness and hunger.
“Earth to Prem, earth to Prem,” called Ernie while Beanie smacked her bony hands and made a resounding clap in the tiled lobby, startling Prem from continuing his thoughts. He stared at them, realizing that of course the two women in their own persons made hash of his argument: They had both had had long working lives and deserved more rather than less of what they got out of the system. Nevertheless, it did not completely detract from his argument that two elderly women on social security were trapped in poverty just as the non-working disabled were.
“What were you thinking that took you so far away?” demanded Ernie, never one to keep questions to herself.
“I, I,–“ Prem didn’t know how to respond.
“Aha! You really were thinking something. It must have been juicy!” Together the two ladies crowed.
Suddenly, Prem decided to take the question seriously. “Actually I was thinking about something. It wasn’t juicy, not the way you think, but it was – I don’t know how to put it. Can I ask you a question?”
“Sure.” The two spoke at one time.
“Okay, then. Tell me when you disagree with me. First of all, this is a society of “haves” and “have-nots,” right? I mean, we have huge inequality, you can see it right here — this building, Number 22, compared to others down the street is just one example.” Prem stopped as if one of the women had spoken. But he saw at once that they were simply waiting for him to go on so he continued, “Clearly it’s no good simply to give a “have-not” everything he or she needs. That’s just what we do now, and in my opinion it leads nowhere but to misery and protracted disability.”
“What if the “have-not” isn’t disabled, but just old? What if the “have-not” works full-time but isn’t paid enough to live on? There are a lot of other ways to be a “have-not” than to be disabled.” These objections came from Beatrice Bean, whose fingers held an imaginary cigarette. She pretended to suck on it, then flick the ashes.
“You’re right. I guess I am a little obsessed with the disability issue. But let me go with just that part of it. If the “haves” somehow could help the disabled “have-nots” gain a set of skills – any set of skills — to become “haves” like themselves, wouldn’t that be better? There are plenty of skills that can be marketed. You don’t need to go to a regular workplace these days to earn a living.”
“I really hate that word, ‘marketed’,” Ernie interjected. “Why does everything have to be for sale? Why must everything be reduced to a matter of money?”
“Because it’s a capitalistic world, that’s why. You and I may not agree with it but we’re stuck with it, and until we can live in a world without money, the have-nots need to learn how to earn.” For all the conviction in his voice, Prem was not that comfortable defending capitalism, especially knowing how avarice had despoiled the natural world he loved so much. But he knew that capitalism had ruled for centuries, and that it wasn’t going to change in his lifetime or the lives of these two women, so it was to all intents and purposes, a fact of life.
“So you are going to teach all the disabled people in Building 22 how to get a paying job? Good luck!” said Beanie with a wry smile. “I don’t personally think anyone here is going to thank you very kindly for it.”
“But don’t you see? That’s precisely what I mean.”
“What do you mean? Why should anyone thank you? If you have an apartment, a social worker, food stamps…you have it made in the shade. Why should you want to work?”
“Because people would feel better about themselves if they could work, that’s why…” Prem said, lamely. He then realized that he had made the mistake of so many do-gooder liberals, believing he knew what was good for those he wanted to help better than they did themselves. But how could he know how they felt without asking them? How could he know whether they felt bad about themselves now or would feel better about themselves working? He hadn’t spoken to most of the residents about the matter. In fact, it had only been Hope, the second floor resident and artist, with whom he had spoken in any depth. It was she who had been so passionately outspoken about feeling trapped in “the System.”
Even as he thought about it Prem realized that things were complicated. Yes, Hope was an artist, and he felt she should be able to sell her work and keep the income at the same time, but wasn’t she also often ill and unstable? It seemed to him that she was hospitalized for weeks at a time, and as frequently as twice a year. What would she do without disability payments when she was ill, he wondered, and how would she survive or cope even as an artist during the inevitable lean times if her disability payments were cut off? Yet she was the tenant who resisted staying on disability, even as it was clear to him that she could not afford to chance getting off it, not unless she could sell paintings regularly or for large sums of money, something that was not likely to happen. People like Hope weren’t discovered by museums or fêted by the rich and famous to be made rich and famous. No, they simply did art and made art alone, steadily, keeping the faith that it was worth it simply because art to them was like food for the rest of us.
Hope wasn’t going to quit painting or making her sculptures just because no one “discovered” her. Hope did art because she had to do art or die. Period. If it sold, well then, good. But so far as Prem knew, Hope had never tried to advertise or sell in the manifold ways that “working artists” sold their art: by marketing themselves and their art in such a way that people come looking to buy. It wasn’t that she would not sell. Prem thought she might be very happy if someone wanted to buy a piece of her artwork. It was simply that she had other things on her mind than making art in order to suit the purchasing public. And what about the others in Building 22 – were they so very different? What did he know? Did he know enough to draw any conclusions at all?
“It’s just such a vicious cycle,” he said, as if finishing a thought he had started aloud.
Beanie seemed to have followed him. “Yah, I agree. But some of these folks have two or three strikes against them before they started out in life. Can you blame them for seeing a tiny fixed income for life better than the insecurity of not knowing whether you can earn anything at all?”
Ernestine Baker seemed to disagree. She counted off on her fingers, as if reciting a litany, “Darryl, Kashina, Bryony, Giorgio, Feder…and that strange woman, Hope. What cases. I wouldn’t want to be in their shoes for a second. I can’t imagine being one of them for a day, not even if you paid me. Talk about unfulfilled lives and unrealized potential!”
“But what are you saying?” remonstrated Prem. “That their lives are wasted? And if they are wasted, whose fault is that? Why have the disabled been allowed not to do something with their lives? That’s my entire point. Look at Giorgio. He was a talented auto mechanic. He wasn’t in the system all his life. He has skills. He just can’t use those skills right now. Feder has savant expertise that surely could be used somewhere productively. Bryony already works three days a week, and Kashinda is so young that it would indeed be a terrible waste if she never learned to do something with her life, except smoke pot. We created a real monster with Federal disability benefits: the same limitations that promote permanent poverty promote never getting better.” Prem could feel himself getting passionate, and wondered just where that came from. Why did he care so much? Why he sounded almost hysterical…
“Okay, what’s going on, Prem?” asked Beanie, peering at him with more than a little concern. “Why don’t you draw up a chair, sit down with us, take a load off…”
Baker, abashed, chimed in, “You want a drink, Prem? The beer is on me.”
His face warm, Prem had felt a sudden but urgent need to be gone. To be anywhere but here. Ashamed of himself, he apologized to the two older women and literally backed away even he spoke, forgetting entirely why he had returned to Building 22 at such an hour in the first place. By the time he remembered the water pressure situation that had occurred just that morning, he was halfway down the block with an old cassette tape playing Dave Mallett’s “Pennsylvania Sunrise,” a song that always made him yearn to hop a train and go places, never to return.
Pennsylvania sunrise…ten degrees at best.
Peerin’ from the window of a club car heading west.
After mornin’ glory…money for the miles.
Someone said I’ll do this for a while.
_____________
I promise more action in the segments I will share in upcoming days. I won’t share the entire novel but I will share some parts of it, enough to entice. I now have c 120 pp. double spaced 37000wds.
Ceterum censeo MAGA esse delendam.
The opinions expressed are those of the author. You go get your own opinions.
Kate Greenough's daily drawings
Réussissez toutes vos certifications de langues
Not your third grade paper mache
Portrait Art and Paintings by Jon Amdall
Books, papers and blogs by Joanna Moncrieff
"While I breathe, I hope"
My Life After Narcissistic Abuse
An intellectual, emotional and spiritual spittoon.
The latest news on WordPress.com and the WordPress community.
Everything Matters
Ceterum censeo MAGA esse delendam.
The opinions expressed are those of the author. You go get your own opinions.
Kate Greenough's daily drawings
Réussissez toutes vos certifications de langues
Not your third grade paper mache
Portrait Art and Paintings by Jon Amdall
Books, papers and blogs by Joanna Moncrieff
"While I breathe, I hope"
My Life After Narcissistic Abuse
An intellectual, emotional and spiritual spittoon.
The latest news on WordPress.com and the WordPress community.
Everything Matters