April 16, 2014
Dear Harold Schwartz, Director of the Institute of Living at Hartford Hospital
I believe that I was profoundly harmed by the treatment I received in 2013 on Donnelly 2 South at the Institute of Living at Hartford Hospital, and that what the staff did to me was not only unethical and cruel but that it crossed the line into illegality from the very first. Psychiatric patient abuse is a pattern in Connecticut hospitals, but it was most egregious at the Institute of Living because the staff told me that they knew what they were doing was wrong but that they would get away with it anyway.
That I know I was a difficult patient never justified staff behavior towards me. I was loud and upset and hard for them to deal with, yes. That is precisely why my Psychiatric Advance Directive (PAD) was written out the way it was, and why I made my medical and psychiatric history online so available. When ill, I am frightened and paranoid, which makes me easily roused to irritability and hostility. I know this, from a distance as it were. But knowing this now does not mean I was in control of my emotions. I am by nature neither temperamental nor prone to temper eruptions or throwing things. In addition, I am extremely modest, hardly one to disrobe or urinate in public. My friends and family have at times variously labeled me “stoic” and “peacemaker,” which should tell you a lot. But that I disrobed and urinated on the floor on Donnelly 2 South both horrifies me and concerns me because these behaviors point to something going on distinct from my psychosis: they point to my having been subject to abuse and trauma at the hospital itself.
Let me make it very clear that if I have behaved in such ways before it was only in response to similar extreme circumstances – as when i was subjected over and over to restraints and seclusion in a horrific and sadistic fashion at Manchester Hospital in 2009 and similarly at Middlesex Hospital in 2010. It is too bad that when Sanjay Banerjee MD and Amy Taylor MD took it upon themselves to violate my HIPAA privacy rights and investigate my previous admissions, without my permission (which I expressly refused to grant) they failed to make the connection between the abuse, and my subsequent behaviors…It turns out all they drew as a conclusion was that if those hospitals could use restraints and seclusion ad libitum, so could they. It didn’t seem to matter to Dr Taylor in particular that in 2009 and 2010 measures such as seclusion and restraints not only didn’t work, they made things worse. Not surprisingly, when Dr Taylor followed these examples I regressed completely, just as my PAD predicted.
I was admitted to Donnelly 2 South, and I came in with a very detailed Psychiatric Advanced Directive as I said. I made it very clear that my online electronic medical record was also available. It included documents such as my narcolepsy diagnostic consult and special documentation assessing my need for a higher than usual dosage of Ritalin, written by my former sleep specialist, Mary B O’Malley, MD PHD who was also my psychiatrist from 2000-2009. Included as well was a letter she wrote to my present psychiatrist, Dr Angela Cappiello, explicitly stating her conviction that I do not have a personality disorder, NOS, borderline traits, or otherwise.
According to Dr. Sanjay Banerjee he read every page of these documents. That is what he told me. He even praised me, saying he wished every patient would come so prepared. Moreover, when he spoke with Dr. Cappiello, he brushed off my concerns about anyone misperceiving me as having a personality disorder. My brother, Philip Spiro, MD, himself a psychiatrist, brought up the same matter when in discussion with Laurie Denenberg, LCSW, but her response was much the same: “Personality disorders are not a part of the picture here. We intend to honor her PAD. We are glad that she has had the foresight to prepare such a document.”
If this was so, then how did it come to pass that Amy Taylor, MD wrote on my history and discharge summary that I have a “long history of Borderline personality disorder” and herself diagnosed “Personality disorder NOS with borderline traits”? I was being treated for four weeks for an active psychotic disorder Axis 1. In any event, she could have no way of knowing whether or not I had a personality disorder, given an active an Axis I diagnosis.
On or around February 4, 2013, I walked in frustration away from the quiet room where I had been held captive for nearly three weeks, strolled down the hall, looked out the window and slowly retraced my steps back to the quiet room, which I had been expressly told was NOT a seclusion room (the definition at Hartford Hospital’s Institute of Living of a seclusion room is a “room to which the door is locked.”) But when I arrived I was confronted by a cohort of staff who proceeded to 4-point restrain me to the bed, even though I was quiet and put up no resistance. Not wanting to give them any reason or justification, I passively lay down on the bed and placed my own limbs out for the restraint cuffs, saying, (I quote my journal entry made later that evening): “For shame. You ought to be ashamed of yourselves. I am not and never was a danger to myself or others.” Their response was “ You refuse to follow directions so we do not know what you will do. This is not punishment, Pamela, this is what your behavior brings on every time.”
From that point on, the threshold for restraints was extremely low. They always restrained me, spread-eagled, so tightly I couldn’t move a muscle. They never permitted bathroom breaks or even used a bedpan, instead they made me defecate in my clothing. They never even let my hands free to eat. I would fall asleep rapidly after three routine punishment needles in the buttocks: Haldol, Ativan and Benadryl—whether I just had my regular meds or not, and they would invent reasons to maintain me in restraints even after I had been asleep for hours. When I woke, groggy and hardly dangerous to anyone, they would grill me with questions that I could not answer. They would then use my inability to respond as reason not to let me out, even when I asked, as the chart recorded, in a “soft sedated voice” for release. They would re-inject me, to put me back to sleep instead.
In the evening on Jan 5th, for the second time that day, they brutally restrained me for throwing half a graham cracker at the wall. Then, as usual, they left me like that for six hours, even after I fell asleep. But in point of fact, though, I could never earn my way to release from restraints by good behavior or quietly, calmly asking for release. I had never done anything to earn my way into them in the first place. I was never violent until they threatened me. They refused to release me until I literally cried, “Uncle” when they told me to.
As to those vaunted “shows of force” what did they expect? Presented with a cohort of threatening staff personnel I saw one thing: an impending assault. I know they anticipated my panic; they said as much in my chart. Isn’t that the point of a planned “show of force” – to induce fear and panic? Why else do it? So why should it be any surprise, when I defended myself when they forcibly, physically grabbed me? When they stuffed me into a body bag and were trying to tighten the straps, surely you can understand why anyone would bite the hand of an attacker whose digits came near the face. I had done nothing but refuse to enter the body bag willingly. I simply was passive. I did not fight or resist until they grabbed my body and assaulted me.
But none of it should have happened. My Advanced Directive explained in exquisite detail exactly what to do and what I respond to better than fear tactics and force. In fact, It is beyond me, knowing that one of the admission diagnoses I came in with was PTSD, how anyone could possibly approve in advance, permission to use restraints and seclusion “just in case they are needed”. Why not counsel the person asking for this advance “right to restrain” to do all in his power not to restrain me and to work with the PAD instead?
Here’s what SAMHSA the substance abuse and mental health services administration publication has to say on seclusion and trauma:
“Studies suggest that restraints and seclusion can be harmful and is often re-traumatizing for an individual who has suffered previous trauma…
“Further, there is a common misconception that seclusion and restraint are used only when absolutely necessary as crisis response techniques. In fact, seclusion and restraint are most commonly used to address loud, disruptive, noncompliant behavior and generally originate from a power struggle between consumer and staff. The decision to apply seclusion or restraint techniques is often arbitrary, idiosyncratic, and generally avoidable.
“Moreover, some studies indicate that seclusion and restraint use leads to an increase in the behaviors that staff members are attempting to control or eliminate.
I have been traumatized, and not just by hospitals. I was date-raped three times in my twenties and experienced traumatic domestic abuse by a long-term roommate. The cover sheet on the PAD made very clear that due to these trauma issues, I could not tolerate being secluded or restrained without serious consequences: regression and serious worsening of symptoms. Unfortunately, as soon as the staff saw fit to use physical methods of coercion and control on me from the first time a staff member grabbed me and pushed me with his lower torso, I ceased improving, and my symptoms went downhill. Did they really think they were being kind and compassionate?
Staff violence begets violence….
I tried to get help even when on the unit, at least I tried when I was free to, to make calls or leave my seclusion… that is to say, forced three -week-long stay in the quiet room last winter. I made many calls to the hospital’s patient advocate office, but the sole time anyone made contact was when the advocate came to hand me some paperwork – I believe I was actually in 4-point restraints at the time — papers I could not read about the forced medication hearing. I needed her advocacy, but she never responded to my panicked calls in any way that was helpful to me. I wanted her help, but she never came by to ask me what I needed. She was less than useful, the fact that I had to go through her, essentially a hospital employee, and her refusal to respond, contributed to my ongoing panic and desperate feelings of aloneness and depression. No wonder Dr. Sanjay Banerjee attempted to force ECT on me, without any prior discussion of it with me whatsoever.
And where did the ECT discussion come from? My PAD states in no uncertain terms that I will refuse ECT under any and every circumstance. My brother would be my conservator if Banerjee had sought to go down that road, and he would never have made any decision to counter my wishes on that subject. If Banerjee really read my PAD, he would have known that. I have already had FORCED ECT and it traumatized me terribly. Also it failed to work.
Banerjee had stopped my 75mg of the antidepressant Zoloft during the first or second week I was there. “Do you really need that?” he had asked, “You don’t seem depressed to me.” Obedient, and in any event glad to get off any medication at any time, I shook my head, assenting to the change. A week later, instead of reinstating the Zoloft, Banerjee blamed my sudden “depression” on my refusal of the anti-seizure medication, Lamictal, a drug I had not taken in 6 months. Now he was applying to force me to take ECT, something I was terrified of, and to have calculated brain damageIt was this threat, and the brutality with which the decision was handed down, that started the downhill course of my IOL stay.
The very next weekday, all hell broke loose. When I entered the conference room, I pushed some important notes across the table that I wanted Dr Banerjee and Laurie Dennenberg to read. They refused, claiming that I threw the papers at them. Instead, Dr Banerjee proceeded to berate me, and told me how he had consulted with other hospitals and providers and had read my records against my instructions and Advance Directive, thus violating my HIPAA rights. Moreover, he threatened me with a behavioral treatment plan that would not permit me to do art or writing unless I “behaved.”
I hit the roof, telling him I would sue the hospital and complain to JCAHO, then summarily left, slamming the door, an act that stemmed from feelings of utter impotence, because I couldn’t actually say in words anything more effective.
It could have ended there. I could have been left alone, to cool down and calm myself. But, no, Dr Banerjee had to write for stat meds again, and even though I was on the phone and trying to find someone to talk to, to calm myself, I had to be physically dragged off the chair I sat on, away from the phone and brought to the floor in a physical struggle (because they had attacked first, i.e. physically grabbed me, I defended myself, instinctually). They could have waited for me to finish the call. They could have waited to see if I calmed myself. I was not hurting anyone or even threatening anyone or myself with harm. All that I had done, in terms of physical threats, was to throw a lightweight chair at the wall. And that, it was clear to everyone, was intended not as a threat to anyone. Furthermore, it was done and over with. I had left that area and gone to my room. I had then come back and now sat on the chair by the phone, speaking to my interlocutor on the other end. There was no need to pick a fight or encourage a struggle. A wait-and-see policy could have successfully guided the situation to a better resolution not only for the situation at hand but for the entire hospital stay. As the poem by Dylan Thomas goes: “After the first death, there is other.” Once they decided to use four—point restraints, there was no going back. The first time broke everything, So they used them again, and again, and more and more freely and without justification but for convenience and punishment.
Back to Feb 5 or 6, after sleeping for six hours, I was taken out of restraints conveniently just in time for a visit from Dr. Angela Cappiello, my outside psychiatrist. Observed by my 1:1 monitor, I only dared whisper and dared not tell the doctor the full extent of the abuse that had been happening. Nevertheless, she took one look at Amy Taylor MD’s behavioral treatment plan posted on my wall, and told me that it would be impossible for anyone, even someone who was well, to follow it properly. She was so worried about me, and about my ability to complete the treatment plan’s requirements, even for the required “24 hours,” that she intervened. The next day, the single day that Dr. Taylor planned to be out of town, Dr. Cappiello asked Dr. Mehendru to evaluate me for discharge, telling her that she feared a power struggle had been set up that I could never win.
When Dr. Mehendru came to see me, at first I was angry, as the chart indicates, thinking she was just another Taylor flunky, preparing to use more restraints and seclusion, But when she asked if I would like to go home, I took one look at her, saw sincerity in her eyes, and burst into a smile, ready to say yes to anything. Miraculously “cured,” I left the IOL that very same day, less than 12 hours after being released from 4-point restraints and not 4 hours out of seclusion.
However, I was not well. Within two weeks time, I was back in the hospital, this time admitted to Yale New Haven Psychiatric Hospital, via their emergency room. Over the next 3 weeks I experienced an entirely different kind of care. At Yale I did not find a staff ready to fight or try to seclude or restrain me.
I was still the same person with the same problems, loud and angry at times, even “violent” to property in my frustration, and still psychotic, yet they never responded with a show of force. Why would they? At Yale it would be absolutely anathema to deliberately frighten a patient. What would be the purpose in that, they would think. They also never pushed me into a seclusion room or strapped me down in punitive 4-point restraints, or any of the other ill-advised responses that my PAD explains are the worst things to do to anyone who is struggling, scared and paranoid. In point of fact, Yale Psychiatric Hospital’s Washington Square unit does not have a seclusion room. They also have a “restraints-free” policy, so they didn’t use those at all either.
The Institute of Living on the other hand with its “We only use restraints and seclusion if we have to” policy, restrained me countless times, and for many more hours than was even legal. When I woke up that last morning, the room opposite me was occupied by yet another person in 4-point restraints! That is because once you allow staff to use restraints a little, it only takes a little to use them a lot. And once you sanction the use of restraints and seclusion at all, it is only time before someone abuses them and abuse becomes the norm.
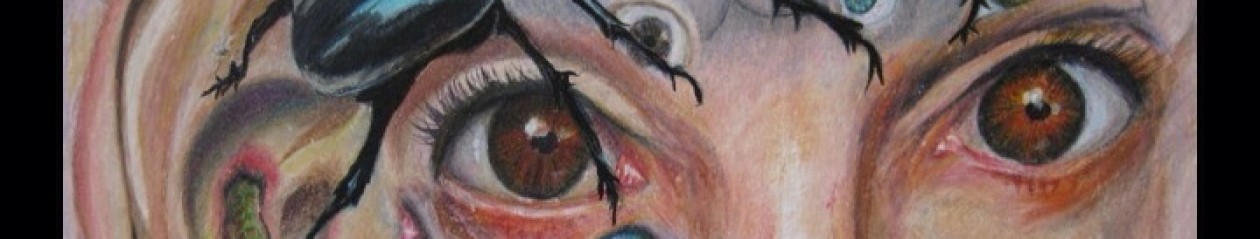
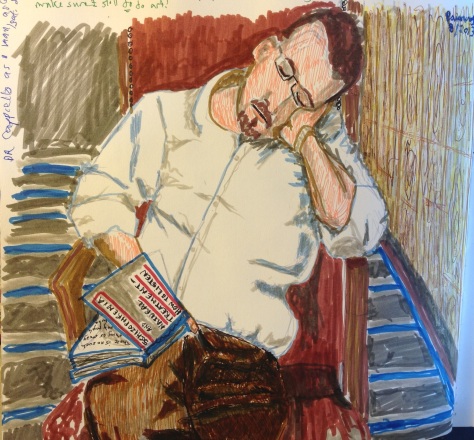
I would like your response to this letter, I have sent it to many people within the state government and outside of it, But you may have the first response. Also you may be interested in the youtube video of my artwork which can be found at this site:
Prior to when you allowed the staff to body bag and restrain me, when I had done nothing wrong but leave the non seclusion quiet room, and you refused to come to my assistance, you had asked to see my artwork. Instead you left me to be tortured. Well, here is some of the art you might have seen had you rescued me from my abusers.:
Sincerely
Pamela Spiro Wagner
The final one you never saw in featured in the post below this one.